Pulmonary embolism pathophysiology: Difference between revisions
No edit summary |
m (Categories) |
||
| (59 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{| class="infobox" style="float:right;" | |||
|- | |||
| [[File:Siren.gif|30px|link=Pulmonary embolism resident survival guide]]|| <br> || <br> | |||
| [[Pulmonary embolism resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] | |||
|} | |||
{{Pulmonary embolism}} | {{Pulmonary embolism}} | ||
{{CMG}} {{ATI}}; {{AE}} {{Rim}} | |||
==Overview== | ==Overview== | ||
Pulmonary embolism (PE) occurs when there is an acute obstruction of the pulmonary artery | Pulmonary embolism (PE) occurs when there is an acute obstruction of the pulmonary artery or one of its branches. It is commonly caused by a venous thrombus that has dislodged from its site of formation and embolized to the arterial blood supply of one of the lungs. The process of clot formation and embolization is termed [[thromboembolism]]. PE results in the elevation of the pulmonary vessel resistance as a consequence of not only mechanical obstruction of the [[capillary]] by the [[embolism]], but also due to pulmonary vasoconstriction. When pulmonary vascular resistance occurs following an acute PE, the rapid increase in the right ventricular [[afterload]] might lead to the dilatation of the right ventricular wall and subsequent [[right heart failure]].<ref name="pmid3916797">{{cite journal| author=Wiedemann HP, Matthay RA| title=Acute right heart failure. | journal=Crit Care Clin | year= 1985 | volume= 1 | issue= 3 | pages= 631-61 | pmid=3916797 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3916797 }} </ref><ref name="pmid7484782">{{cite journal| author=Lualdi JC, Goldhaber SZ| title=Right ventricular dysfunction after acute pulmonary embolism: pathophysiologic factors, detection, and therapeutic implications. | journal=Am Heart J | year= 1995 | volume= 130 | issue= 6 | pages= 1276-82 | pmid=7484782 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7484782 }} </ref> | ||
==Pathophysiology== | == Pathophysiology == | ||
=== Clot Formation === | |||
* Most PE commonly originate from a [[thrombus]] that has formed in the [[iliofemoral vein]], deep within the vasculature of the lower extremity. | |||
* Less commonly, a PE may also arise from a [[thrombus]] in the upper extremity veins, renal veins, or pelvic veins. | |||
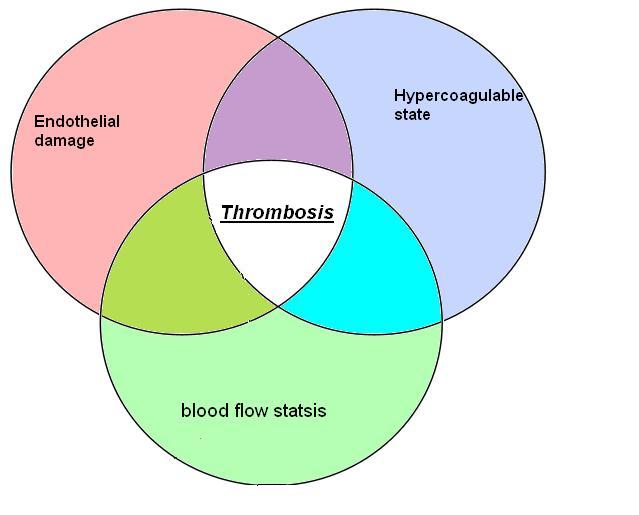
* The development of thrombosis is classically due to a group of conditions referred to as [[Virchow's triad]]. Virchow's triad includes alterations in [[blood flow]], factors in the vessel wall, and factors affecting the properties of the [[blood]]. It is common for more than one risk factor to be present. Shown below is an image depicting [[Virchow's triad]]. | |||
[[File:VTE Pathophysisology Virchow's triad.JPG|300x400px]] | |||
=== Embolization === | |||
* After its formation, a thrombus might dislodge from the site of origin and circulate through the [[inferior vena cava]], into the right ventricle, and into the pulmonary vasculature.<ref name="McGill">McGill University. (2004, June 24). Pulmonary Embolism. Retrieved May 7, 2012, from McGill Virtual Stethoscope Pathophysiology.</ref> | |||
=== Hemodynamic Consequences === | |||
*Hemodynamic complications and the nature of the clinical manifestations of a PE depend on a number of factors:<ref name="Hellas">Kostadima, E., & Zakynthinos, E. (2007). Pulmonary Embolism: Pathophysiology, Diagnosis, Treatment. Hellenic Journal of Cardiology, 94-107.</ref> | |||
* | ** The size of the [[embolus]] and the degree to which it occludes the vascular tree and its subsequent branches | ||
* | ** The presence of any preexisting cardiopulmonary conditions | ||
** The role of chemical [[vasoconstriction]] as it is insinuated by [[platelets]] releasing [[serotonin]] and [[thromboxane]] in addition to other vasoconstrictors | |||
** The presence of pulmonary artery dilatation and subsequent [[vasoconstriction|reflex vasoconstriction]] | |||
* PE results in the elevation of the pulmonary vessel resistance as a consequence of not only mechanical obstruction of the [[capillary]] by the [[embolism]], but also due to pulmonary vasoconstriction. Pulmonary vasoconstriction can be either biochemically mediated, hypoxia induced, or reflex-induced.<ref name="pmid1555481">{{cite journal| author=Elliott CG| title=Pulmonary physiology during pulmonary embolism. | journal=Chest | year= 1992 | volume= 101 | issue= 4 Suppl | pages= 163S-171S | pmid=1555481 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1555481 }} </ref><ref name="pmid11033105">{{cite journal| author=Smulders YM| title=Pathophysiology and treatment of haemodynamic instability in acute pulmonary embolism: the pivotal role of pulmonary vasoconstriction. | journal=Cardiovasc Res | year= 2000 | volume= 48 | issue= 1 | pages= 23-33 | pmid=11033105 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11033105 }} </ref> | |||
* Several mediators are involved the pulmonary [[vasoconstriction]] that occurs in the setting of acute PE, such as: | |||
** [[Thromboxane A2]] (end product of [[arachidonic acid]] metabolism)<ref name="pmid11033105">{{cite journal| author=Smulders YM| title=Pathophysiology and treatment of haemodynamic instability in acute pulmonary embolism: the pivotal role of pulmonary vasoconstriction. | journal=Cardiovasc Res | year= 2000 | volume= 48 | issue= 1 | pages= 23-33 | pmid=11033105 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11033105 }} </ref> | |||
** [[Serotonin]] (vasoconstrictor in the pulmonary circulation and vasodilator in the systemic circulation)<ref name="pmid11033105">{{cite journal| author=Smulders YM| title=Pathophysiology and treatment of haemodynamic instability in acute pulmonary embolism: the pivotal role of pulmonary vasoconstriction. | journal=Cardiovasc Res | year= 2000 | volume= 48 | issue= 1 | pages= 23-33 | pmid=11033105 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11033105 }} </ref> | |||
** [[Endothelin 1]]<ref name="pmid11033105">{{cite journal| author=Smulders YM| title=Pathophysiology and treatment of haemodynamic instability in acute pulmonary embolism: the pivotal role of pulmonary vasoconstriction. | journal=Cardiovasc Res | year= 2000 | volume= 48 | issue= 1 | pages= 23-33 | pmid=11033105 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11033105 }} </ref> | |||
** [[Prostaglandin F2α]]<ref name="pmid11033105">{{cite journal| author=Smulders YM| title=Pathophysiology and treatment of haemodynamic instability in acute pulmonary embolism: the pivotal role of pulmonary vasoconstriction. | journal=Cardiovasc Res | year= 2000 | volume= 48 | issue= 1 | pages= 23-33 | pmid=11033105 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11033105 }} </ref> | |||
** [[Thrombin]]<ref name="pmid14656907">{{cite journal| author=Goldhaber SZ, Elliott CG| title=Acute pulmonary embolism: part I: epidemiology, pathophysiology, and diagnosis. | journal=Circulation | year= 2003 | volume= 108 | issue= 22 | pages= 2726-9 | pmid=14656907 | doi=10.1161/01.CIR.0000097829.89204.0C | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14656907 }} </ref> | |||
** [[Histamine]]<ref name="pmid14656907">{{cite journal| author=Goldhaber SZ, Elliott CG| title=Acute pulmonary embolism: part I: epidemiology, pathophysiology, and diagnosis. | journal=Circulation | year= 2003 | volume= 108 | issue= 22 | pages= 2726-9 | pmid=14656907 | doi=10.1161/01.CIR.0000097829.89204.0C | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14656907 }} </ref> | |||
* While [[serotonin]] and [[thromboxane A2]] are mainly produced by activated [[platelets]], the vascular wall and pulmonary neuroendocrine cells might also be the source of some [[vasoconstrictor]]s.<ref name="pmid11033105">{{cite journal| author=Smulders YM| title=Pathophysiology and treatment of haemodynamic instability in acute pulmonary embolism: the pivotal role of pulmonary vasoconstriction. | journal=Cardiovasc Res | year= 2000 | volume= 48 | issue= 1 | pages= 23-33 | pmid=11033105 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11033105 }} </ref> | |||
* [[Prostacyclin]] is a vasodilator produced by the [[endothelial cells]] in response to the hemodynamic changes induced by the acute PE.<ref name="pmid11033105">{{cite journal| author=Smulders YM| title=Pathophysiology and treatment of haemodynamic instability in acute pulmonary embolism: the pivotal role of pulmonary vasoconstriction. | journal=Cardiovasc Res | year= 2000 | volume= 48 | issue= 1 | pages= 23-33 | pmid=11033105 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11033105 }} </ref> | |||
{{ | |||
* When pulmonary vascular resistance occurs following an acute PE, the rapid increase in the right ventricular [[afterload]] might lead to the dilatation of the right ventricular wall and subsequent [[right heart failure]]. In addition, the elevated pulmonary vascular resistance causes a decrease in the [[LV|left ventricular]] [[preload]] and consequently leads to systemic [[hypotension]].<ref name="pmid3916797">{{cite journal| author=Wiedemann HP, Matthay RA| title=Acute right heart failure. | journal=Crit Care Clin | year= 1985 | volume= 1 | issue= 3 | pages= 631-61 | pmid=3916797 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3916797 }} </ref><ref name="pmid7484782">{{cite journal| author=Lualdi JC, Goldhaber SZ| title=Right ventricular dysfunction after acute pulmonary embolism: pathophysiologic factors, detection, and therapeutic implications. | journal=Am Heart J | year= 1995 | volume= 130 | issue= 6 | pages= 1276-82 | pmid=7484782 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7484782 }} </ref> In patients with underlying cardiopulmonary disease, the [[cardiac output]] suffers substantial deterioration in overall output as compared to otherwise healthy individuals. | |||
* [[Right heart failure]], as well as systemic [[hypotension]], can attenuate coronary perfusion and contribute to subsequent [[coronary ischemia]].<ref name="pmid3916797">{{cite journal| author=Wiedemann HP, Matthay RA| title=Acute right heart failure. | journal=Crit Care Clin | year= 1985 | volume= 1 | issue= 3 | pages= 631-61 | pmid=3916797 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3916797 }} </ref><ref name="pmid7484782">{{cite journal| author=Lualdi JC, Goldhaber SZ| title=Right ventricular dysfunction after acute pulmonary embolism: pathophysiologic factors, detection, and therapeutic implications. | journal=Am Heart J | year= 1995 | volume= 130 | issue= 6 | pages= 1276-82 | pmid=7484782 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7484782 }} </ref> | |||
* In summary, the hemodynamic consequences of PE include: | |||
**[[Pulmonary hypertension]] | |||
**[[Right ventricular strain]] | |||
**[[Right heart failure]] | |||
**[[Systemic hypotension]] | |||
===Abnormalities in Gas Exchange=== | |||
* In PE, [[hypoxemia]] occurs mainly due to the ventilation perfusion mismatch.<ref name="pmid14656907">{{cite journal| author=Goldhaber SZ, Elliott CG| title=Acute pulmonary embolism: part I: epidemiology, pathophysiology, and diagnosis. | journal=Circulation | year= 2003 | volume= 108 | issue= 22 | pages= 2726-9 | pmid=14656907 | doi=10.1161/01.CIR.0000097829.89204.0C | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14656907 }} </ref> In fact, in the setting of an acute PE, the ventilation to perfusion ratio (V/Q) increases and the dead space enlarges.<ref name="pmid12468507">{{cite journal| author=Itti E, Nguyen S, Robin F, Desarnaud S, Rosso J, Harf A et al.| title=Distribution of ventilation/perfusion ratios in pulmonary embolism: an adjunct to the interpretation of ventilation/perfusion lung scans. | journal=J Nucl Med | year= 2002 | volume= 43 | issue= 12 | pages= 1596-602 | pmid=12468507 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12468507 }} </ref> | |||
* In addition, the occurrence of [[right to left shunt]] also contributes to the [[hypoxemia]] among patients with PE. When [[right to left shunt]] occurs, the administration of oxygen to the patient fails to correct the [[hypoxemia]].<ref name="pmid14656907">{{cite journal| author=Goldhaber SZ, Elliott CG| title=Acute pulmonary embolism: part I: epidemiology, pathophysiology, and diagnosis. | journal=Circulation | year= 2003 | volume= 108 | issue= 22 | pages= 2726-9 | pmid=14656907 | doi=10.1161/01.CIR.0000097829.89204.0C | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14656907 }} </ref> | |||
* [[Hypocapnia]] occurs among patients with PE secondary to a compensatory increase in the [[minute ventilation]].<ref name="pmid14656907">{{cite journal| author=Goldhaber SZ, Elliott CG| title=Acute pulmonary embolism: part I: epidemiology, pathophysiology, and diagnosis. | journal=Circulation | year= 2003 | volume= 108 | issue= 22 | pages= 2726-9 | pmid=14656907 | doi=10.1161/01.CIR.0000097829.89204.0C | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14656907 }} </ref> | |||
==References== | ==References== | ||
{{ | {{Reflist|2}} | ||
[[Category:Hematology]] | [[Category:Hematology]] | ||
| Line 56: | Line 69: | ||
[[Category:Up-To-Date]] | [[Category:Up-To-Date]] | ||
[[Category:Up-To-Date cardiology]] | [[Category:Up-To-Date cardiology]] | ||
[[Category:Intensive care medicine]] | |||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
Latest revision as of 18:08, 7 June 2016
| Resident Survival Guide |
|
Pulmonary Embolism Microchapters |
|
Diagnosis |
|---|
|
Pulmonary Embolism Assessment of Probability of Subsequent VTE and Risk Scores |
|
Treatment |
|
Follow-Up |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Pulmonary embolism pathophysiology On the Web |
|
Directions to Hospitals Treating Pulmonary embolism pathophysiology |
|
Risk calculators and risk factors for Pulmonary embolism pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] The APEX Trial Investigators; Associate Editor(s)-in-Chief: Rim Halaby, M.D. [2]
Overview
Pulmonary embolism (PE) occurs when there is an acute obstruction of the pulmonary artery or one of its branches. It is commonly caused by a venous thrombus that has dislodged from its site of formation and embolized to the arterial blood supply of one of the lungs. The process of clot formation and embolization is termed thromboembolism. PE results in the elevation of the pulmonary vessel resistance as a consequence of not only mechanical obstruction of the capillary by the embolism, but also due to pulmonary vasoconstriction. When pulmonary vascular resistance occurs following an acute PE, the rapid increase in the right ventricular afterload might lead to the dilatation of the right ventricular wall and subsequent right heart failure.[1][2]
Pathophysiology
Clot Formation
- Most PE commonly originate from a thrombus that has formed in the iliofemoral vein, deep within the vasculature of the lower extremity.
- Less commonly, a PE may also arise from a thrombus in the upper extremity veins, renal veins, or pelvic veins.
- The development of thrombosis is classically due to a group of conditions referred to as Virchow's triad. Virchow's triad includes alterations in blood flow, factors in the vessel wall, and factors affecting the properties of the blood. It is common for more than one risk factor to be present. Shown below is an image depicting Virchow's triad.
Embolization
- After its formation, a thrombus might dislodge from the site of origin and circulate through the inferior vena cava, into the right ventricle, and into the pulmonary vasculature.[3]
Hemodynamic Consequences
- Hemodynamic complications and the nature of the clinical manifestations of a PE depend on a number of factors:[4]
- The size of the embolus and the degree to which it occludes the vascular tree and its subsequent branches
- The presence of any preexisting cardiopulmonary conditions
- The role of chemical vasoconstriction as it is insinuated by platelets releasing serotonin and thromboxane in addition to other vasoconstrictors
- The presence of pulmonary artery dilatation and subsequent reflex vasoconstriction
- PE results in the elevation of the pulmonary vessel resistance as a consequence of not only mechanical obstruction of the capillary by the embolism, but also due to pulmonary vasoconstriction. Pulmonary vasoconstriction can be either biochemically mediated, hypoxia induced, or reflex-induced.[5][6]
- Several mediators are involved the pulmonary vasoconstriction that occurs in the setting of acute PE, such as:
- Thromboxane A2 (end product of arachidonic acid metabolism)[6]
- Serotonin (vasoconstrictor in the pulmonary circulation and vasodilator in the systemic circulation)[6]
- Endothelin 1[6]
- Prostaglandin F2α[6]
- Thrombin[7]
- Histamine[7]
- While serotonin and thromboxane A2 are mainly produced by activated platelets, the vascular wall and pulmonary neuroendocrine cells might also be the source of some vasoconstrictors.[6]
- Prostacyclin is a vasodilator produced by the endothelial cells in response to the hemodynamic changes induced by the acute PE.[6]
- When pulmonary vascular resistance occurs following an acute PE, the rapid increase in the right ventricular afterload might lead to the dilatation of the right ventricular wall and subsequent right heart failure. In addition, the elevated pulmonary vascular resistance causes a decrease in the left ventricular preload and consequently leads to systemic hypotension.[1][2] In patients with underlying cardiopulmonary disease, the cardiac output suffers substantial deterioration in overall output as compared to otherwise healthy individuals.
- Right heart failure, as well as systemic hypotension, can attenuate coronary perfusion and contribute to subsequent coronary ischemia.[1][2]
- In summary, the hemodynamic consequences of PE include:
Abnormalities in Gas Exchange
- In PE, hypoxemia occurs mainly due to the ventilation perfusion mismatch.[7] In fact, in the setting of an acute PE, the ventilation to perfusion ratio (V/Q) increases and the dead space enlarges.[8]
- In addition, the occurrence of right to left shunt also contributes to the hypoxemia among patients with PE. When right to left shunt occurs, the administration of oxygen to the patient fails to correct the hypoxemia.[7]
- Hypocapnia occurs among patients with PE secondary to a compensatory increase in the minute ventilation.[7]
References
- ↑ 1.0 1.1 1.2 Wiedemann HP, Matthay RA (1985). "Acute right heart failure". Crit Care Clin. 1 (3): 631–61. PMID 3916797.
- ↑ 2.0 2.1 2.2 Lualdi JC, Goldhaber SZ (1995). "Right ventricular dysfunction after acute pulmonary embolism: pathophysiologic factors, detection, and therapeutic implications". Am Heart J. 130 (6): 1276–82. PMID 7484782.
- ↑ McGill University. (2004, June 24). Pulmonary Embolism. Retrieved May 7, 2012, from McGill Virtual Stethoscope Pathophysiology.
- ↑ Kostadima, E., & Zakynthinos, E. (2007). Pulmonary Embolism: Pathophysiology, Diagnosis, Treatment. Hellenic Journal of Cardiology, 94-107.
- ↑ Elliott CG (1992). "Pulmonary physiology during pulmonary embolism". Chest. 101 (4 Suppl): 163S–171S. PMID 1555481.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 Smulders YM (2000). "Pathophysiology and treatment of haemodynamic instability in acute pulmonary embolism: the pivotal role of pulmonary vasoconstriction". Cardiovasc Res. 48 (1): 23–33. PMID 11033105.
- ↑ 7.0 7.1 7.2 7.3 7.4 Goldhaber SZ, Elliott CG (2003). "Acute pulmonary embolism: part I: epidemiology, pathophysiology, and diagnosis". Circulation. 108 (22): 2726–9. doi:10.1161/01.CIR.0000097829.89204.0C. PMID 14656907.
- ↑ Itti E, Nguyen S, Robin F, Desarnaud S, Rosso J, Harf A; et al. (2002). "Distribution of ventilation/perfusion ratios in pulmonary embolism: an adjunct to the interpretation of ventilation/perfusion lung scans". J Nucl Med. 43 (12): 1596–602. PMID 12468507.