Mitral regurgitation resident survival guide: Difference between revisions
No edit summary |
Sergekorjian (talk | contribs) |
||
| (183 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div style="-webkit-user-select: none;"> | |||
<div style="width: 80%;"> | |||
__NOTOC__ | __NOTOC__ | ||
{{ | {{CMG}}; {{AE}} {{M.P}} | ||
{{ | |||
{| class="infobox" style="margin: 0 0 0 0; border: 0; float: right; width: 100px; background: #A8A8A8; position: fixed; top: 250px; right: 21px; border-radius: 0 0 10px 10px;" cellpadding="0" cellspacing="0"; | |||
|- | |||
! style="padding: 0 5px; font-size: 85%; background: #A8A8A8" align=center| {{fontcolor|#2B3B44|Mitral Regurgitation Resident Survival Guide Microchapters}} | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral regurgitation resident survival guide#Overview|Overview]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral regurgitation resident survival guide#Causes|Causes]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral regurgitation resident survival guide#FIRE: Focused Initial Rapid Evaluation|FIRE]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral regurgitation resident survival guide#Complete Diagnostic Approach to Mitral Regurgitation|Complete Diagnostic Approach]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral regurgitation resident survival guide#Treatment|Treatment]] | |||
:[[Mitral regurgitation resident survival guide#Treatment of Acute Mitral Regurgitation|Acute MR]] | |||
:[[Mitral regurgitation resident survival guide#Treatment of Chronic Mitral Regurgitation|Chronic MR]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral regurgitation resident survival guide#Do's|Do's]] | |||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Mitral regurgitation resident survival guide#Don'ts|Don'ts]] | |||
|} | |||
==Overview== | ==Overview== | ||
Mitral regurgitation is a disorder of the valve | [[Mitral regurgitation]] ([[MR]]) is a disorder of the heart characterized by failure of the [[mitral valve]] to close properly during [[systole]] leading to blood leakage from the [[left ventricle]] to the [[left atrium]] during [[systole]]. Individuals with [[acute mitral regurgitation]] may present with significant hemodynamic instability due to the sudden drop in [[cardiac output]], leading to acute pulmonary edema, hypotension and possible cardiogenic shock. Individuals with chronic compensated mitral regurgitation may be asymptomatic, with a normal exercise tolerance and no evidence of [[heart failure]], or may present with fatigue, dyspnea on exertion, orthopnea, and paroxysmal nocturnal dyspnea.<ref name="pmid19564568">{{cite journal| author=Stout KK, Verrier ED| title=Acute valvular regurgitation. | journal=Circulation | year= 2009 | volume= 119 | issue= 25 | pages= 3232-41 | pmid=19564568 | doi=10.1161/CIRCULATIONAHA.108.782292 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19564568 }} </ref> The management of [[MR]] includes afterload reduction with careful monitoring of fluid status, management of the underlying disease (CAD, mitral valve prolapse, rheumatic heart disease), and early surgical intervention in severe cases. Ultimately, the management of MR depends on the anatomy of the mitral valve, the acuteness of the disease process, and the severity of presentation. <ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref> | ||
==Causes== | |||
===Life Threatening Causes=== | |||
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated. | |||
* [[Acute myocardial infarction]] | |||
* [[chest trauma|Blunt chest trauma]] | |||
* [[Infective endocarditis]] | |||
===Common Causes=== | |||
====Acute Mitral Regurgitation==== | |||
* [[Papillary muscle rupture]]: | |||
** [[Acute myocardial infarction]] | |||
** [[Chest trauma]] | |||
* [[Myocardial rupture|Ruptured mitral chordae tendinae]]: | |||
** [[Acute rheumatic fever]]<ref name="pmid17854408">{{cite journal| author=Anderson Y, Wilson N, Nicholson R, Finucane K| title=Fulminant mitral regurgitation due to ruptured chordae tendinae in acute rheumatic fever. | journal=J Paediatr Child Health | year= 2008 | volume= 44 | issue= 3 | pages= 134-7 | pmid=17854408 | doi=10.1111/j.1440-1754.2007.01214.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17854408 }} </ref> | |||
** [[Chest trauma]]<ref name="pmid9580528">{{cite journal| author=Grinberg AR, Finkielman JD, Piñeiro D, Festa H, Cazenave C| title=Rupture of mitral chorda tendinea following blunt chest trauma. | journal=Clin Cardiol | year= 1998 | volume= 21 | issue= 4 | pages= 300-1 | pmid=9580528 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9580528 }} </ref> | |||
** [[Mitral valve prolapse]]<ref name="pmid6837414">{{cite journal| author=Grenadier E, Alpan G, Keidar S, Palant A| title=The prevalence of ruptured chordae tendineae in the mitral valve prolapse syndrome. | journal=Am Heart J | year= 1983 | volume= 105 | issue= 4 | pages= 603-10 | pmid=6837414 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6837414 }} </ref> | |||
** [[Infective endocarditis]] | |||
** Spontaneous rupture | |||
== | ====Chronic Primary Mitral Regurgitation==== | ||
Mitral regurgitation | * [[Marfan's syndrome]] | ||
* [[Mitral annular calcification]]<ref name="pmid11547744">{{cite journal| author=Otto CM| title=Clinical practice. Evaluation and management of chronic mitral regurgitation. | journal=N Engl J Med | year= 2001 | volume= 345 | issue= 10 | pages= 740-6 | pmid=11547744 | doi=10.1056/NEJMcp003331 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11547744 }} </ref> | |||
* [[Mitral valve prolapse]] | |||
* [[Myxomatous degeneration]] | |||
== | ====Chronic Secondary Mitral Regurgitation==== | ||
Mitral | * [[Dilated cardiomyopathy]] | ||
* [[ | |||
* [[Infective endocarditis]] | * [[Infective endocarditis]] | ||
* [[Ischemic heart disease]] | * [[Ischemic heart disease]]<ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref> | ||
Click '''[[Mitral regurgitation causes|here]]''' for the complete list of causes. | |||
==FIRE: Focused Initial Rapid Evaluation== | |||
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention. | |||
<span style="font-size:85%">Boxes in red color signify that an urgent management is needed.</span> | |||
<span style="font-size:85%">'''Abbreviations:''' '''ARBs''': Angiotensin II receptor antagonist; '''CABG''': Coronary artery bypass surgery; '''HF''': Heart failure; '''IE''': Infective endocarditis; '''LVEF''': Left ventricular ejection fraction; '''LV''': Left ventricle; '''MR''': Mitral regurgitation; '''S1''': First heart sound; '''S2''': Second heart sound </span> <br> | |||
{{Family tree/start}} | |||
{{familytree | | | | | | | | | A01 | | | | | | | | | A01=<div style="width:25em">'''Identify cardinal findings that increase the pretest probability of mitral regurgitation:'''</div><br><div style="width:22em; text-align:left"> | |||
❑ [[Murmur]]: | |||
:❑ Soft, low pitched and decrescendo (in acute [[MR]] due to diminished pressure gradient between the [[left atrium]] and [[ventricle]]) | |||
:❑ High pitched and blowing [[holosystolic murmur]] best heard over the [[apex]] radiating to the [[axilla]] and back | |||
:❑ Silent (in acute [[ischemic MR]]) | |||
❑ [[Heart sounds]]: | |||
:❑ [[S1]] is diminished (typical) | |||
:❑ Wide splitting of [[S2]] (low forward flow causing early [[A2]]) | |||
</div> }} | |||
{{familytree | | | | | | | | | |!| | | | | | | | | | }} | |||
{{familytree | | | | | | | | | A01 | | | | | | | | | | A01= <div style="text-align: left; width: 18em; padding: 1em;">'''Does the patient have any of the following findings of acute mitral regurgitation with instability?'''<br> | |||
❑ Sudden onset and rapid progression of [[pulmonary edema]]: <br> | |||
:❑ [[Shortness of breath]]<br> | |||
:❑ [[Tachypnea]]<br> | |||
:❑ [[Crackles]] or [[rales]] <br> | |||
❑ [[Cardiogenic shock physical examination|Signs and symptoms of cardiogenic shock]]: <BR> | |||
:❑ [[Tachycardia]] <br> | |||
:❑ [[Hypotension]]<br> | |||
:❑ [[Altered mental status]]<br> | |||
:❑ [[Oliguria]]<br> | |||
:❑ [[Diaphoresis]] | |||
:❑ [[Cold extremities]] | |||
:❑ [[Peripheral cyanosis]] | |||
:❑ [[Mottling]] | |||
</div>}} | |||
{{familytree | | | | | | | |,|-|^|-|.| | | | |}} | |||
{{familytree |boxstyle= padding: 0; background: #FA8072; text-align: center;| | | | | | A01 | | | A02 | | | | |A01={{fontcolor|#F8F8FF|'''Yes'''}}| A02=<div style="text-align: center; background: #FFFFFF; height: 25px; line-height: 25px;">'''No'''</div>}} | |||
{{familytree | | | | | | | |!| | | |!| | }} | |||
{{familytree | | | | | | | |!| | | A02 | | | | | | A02= [[Mitral regurgitation resident survival guide#Complete Diagnostic Approach|'''Continue with complete diagnostic approach below''']]}} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | | | A01 | | | | | | A01=<div style="float: left; text-align: left; width: 25em; padding:1em;"> '''Initiate resuscitative measures:'''<br> | |||
❑ Secure airway <br> | |||
❑ Administer O2 <br> | |||
❑ Establish 2 wide bore IV access <br> | |||
❑ Establish an arterial line<br> | |||
❑ Connect to ECG monitor<br> | |||
❑ Monitor vitals continuously<br> | |||
❑ Consider ICU admission<br> | |||
❑ Consider [[mechanical ventilation|<span style="color:white;">mechanical ventilation</span>]]<br> | |||
❑ Consider [[pulmonary artery catheterization|<span style="color:white;">pulmonary artery catheterization</span>]] | |||
---- | |||
'''Order imaging and blood tests (urgent):'''<br> | |||
❑ [[Transthoracic echocardiography|<span style="color:white;">Transthoracic echocardiography</span>]] ([[TTE|<span style="color:white;">TTE</span>]])<br> | |||
❑ [[Chest X-ray|<span style="color:white;">Chest X-ray</span>]]<br> | |||
❑ [[CBC|<span style="color:white;">CBC</span>]] <br> | |||
❑ [[Serum electrolytes|<span style="color:white;">Serum electrolytes</span>]]<br> | |||
❑ [[Blood cultures|<span style="color:white;">Blood cultures</span>]] (in case of fever) <br> | |||
❑ Serum cardiac [[troponin|<span style="color:white;">troponin</span>]] I and T <br> | |||
❑ [[Creatine kinase|<span style="color:white;">Creatine kinase</span>]] (CK-MB) <br> | |||
❑ Serum [[urea|<span style="color:white;">urea</span>]] and [[creatinine|<span style="color:white;">creatinine</span>]] <br> | |||
</div>}} | |||
{{familytree | | | | | | | |!| | | | | | }} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | | | A01 | | | | | A01='''Does the patient has any evidence of MR in TTE?'''}} | |||
{{familytree | | | | | |,|-|^|-|.| | | | }} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | A01 | | A02 | | | A01=Yes| A02=No}} | |||
{{familytree | | | | | |!| | | |!| | | | }} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | A01 | | A02 | | | A01= <div style="text-align: left; width: 18em; padding: 1em;"> | |||
'''Stabilize the patient:'''<br> | |||
❑ Initiate medical stabilization: | |||
:❑ [[Vasodilator|<span style="color:white;">Vasodilator</span>]] (IV [[nitroprusside|<span style="color:white;">nitroprusside</span>]]) '''PLUS''' inotropic agents (IV [[dobutamine|<span style="color:white;">dobutamine</span>]]) <br> | |||
❑ Establish [[intra-aortic balloon pump|<span style="color:white;">intra-aortic balloon pump</span>]]:<br> | |||
:❑ If medical therapy is not effective to maintain hemodynamic stability<br> | |||
---- | |||
'''Initiate treatment for specific etiologies:'''<br> | |||
❑ [[Aspirin|<span style="color:white;">Aspirin</span>]] in case of myocardial infarction<br> | |||
❑ Antibiotics in case of [[Infective endocarditis resident survival guide|<span style="color:white;">infective endocarditis</span>]] | |||
</div>| A02= <div style="text-align: left; width: 18em; padding: 1em;">'''Consider other possible diagnosis:'''<br> | |||
❑ [[Acute respiratory distress syndrome|<span style="color:white;">Acute respiratory distress syndrome</span>]] | |||
❑ [[Sepsis|<span style="color:white;">Sepsis</span>]]<br> | |||
</div>}} | |||
{{familytree | | | | | |!| | | | | | }} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | | | A01 | | | | | | A01= <div style="text-align: left; width: 18em; padding: 1em;">'''Does the patient have any findings on TTE that require mitral valve surgery?'''<br> | |||
❑ Flail mitral leaflet (papillary muscle or chordal rupture)<br> | |||
❑ Any signs of [[endocarditis|<span style="color:white;">endocarditis</span>]] <br> | |||
:❑ Vegetations on the leaflets | |||
:❑ Paravalvular abscess | |||
❑ Moderate to severe ischemic MR <br></div>}} | |||
{{familytree | | | |,|-|^|-|.| | | | }} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | A01 | | A02 | | | | A01=Yes| A02=No}} | |||
{{familytree | | | |!| | | |!| | | | | }} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | A01 | | A02 | | | | A01=<div style="text-align: left; width: 18em; padding: 1em;">'''Perform mitral valve surgery:'''<br> | |||
❑ [[Mitral valve repair|<span style="color:white;">Mitral valve repair</span>]]: <br> | |||
:❑ Most preferred | |||
:❑ Done in absence of [[papillary muscle|<span style="color:white;">papillary muscle</span>]] necrosis | |||
❑ [[Mitral valve replacement|<span style="color:white;">Mitral valve replacement</span>]]: | |||
:❑ Performed in cases of complex MR with extensive tissue destruction | |||
:❑ Performed in cases of MR with lateral LV wall motion abnormality | |||
</div>| A02=<div style="text-align: left; width: 18em; padding: 1em;">'''Perform reperfusion or revascularization:'''<br> | |||
---- | |||
❑ In patients with acute coronary syndrome, [[CABG|<span style="color:white;">CABG</span>]] or [[coronary angioplasty|<span style="color:white;">coronary angioplasty</span>]] should be performed<br> | |||
❑ Early reperfusion for [[myocardial infarction|<span style="color:white;">myocardial infarction</span>]] can reduce localized [[LV|<span style="color:white;">LV</span>]] remodeling and hence [[MR|<span style="color:white;">MR</span>]] | |||
</div>}} | |||
{{familytree | | | |!| | | | | | | | }} | |||
{{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | A01 | | | | | | A01=<div style="text-align: left; width: 18em; padding: 1em;">'''Perform reperfusion or revascularization:'''<br> | |||
❑ Perform [[CABG|<span style="color:white;">CABG</span>]] or [[coronary angioplasty|<span style="color:white;">coronary angioplasty</span>]] at the time of mitral valve surgery in patients with myocardial infarction<br> | |||
---- | |||
'''Consider cardiac transplantation:'''<br> | |||
❑ On some occasions with no contraindication for surgery<br> | |||
❑ For patients with severe LV dysfunction | |||
</div>}} | |||
{{Family tree/end}} | |||
==Complete Diagnostic Approach to Mitral Regurgitation== | |||
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.<ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref>.<br> | |||
<span style="font-size:85%">'''Abbreviations:''' '''AF''': Atrial fibrillation; '''MR''': Mitral regurgitation; '''EKG''': Electrocardiogram; '''EF''': Ejection fraction; '''S1''': First heart sound; '''S2''': Second heart sound; '''S3''': Third heart sound; '''LV''': Left ventricle; '''MVP''': Mitral valve prolapse</span> <br> | |||
{{family tree/start}} | |||
{{family tree| | | | | | | A01 | | | | | A01= <div style="float: left; text-align: left; width:25em; padding:1em;">'''Characterize the symptoms:'''<br> | |||
'''Acute mitral regurgitation:''' | |||
❑ '''Symptoms of [[shock]] and [[pulmonary edema]]:'''<br> | |||
:❑ [[Shortness of breath]]<br> | |||
:❑ [[Orthopnea]]<br> | |||
:❑ [[Paroxysmal nocturnal dyspnea]]<br> | |||
:❑ [[Cough]]<br> | |||
:❑ [[Altered mental status]]<br> | |||
:❑ [[edema|Pedel edema]] | |||
:❑ [[Oliguria]]<br> | |||
:❑ [[Cyanosis]] | |||
:❑ [[Pallor]] | |||
:❑ [[Diaphoresis]] | |||
:❑ [[Abdominal pain]] (may be suggestive of [[mesenteric ischemia]]) | |||
❑ '''Symptoms suggestive of precipitating events:'''<br> | |||
:❑ [[Chest pain]] (suggestive of [[myocardial ischemia]]) | |||
:❑ [[Fever]] (suggestive of [[infective endocarditis]]) | |||
:❑ [[Petechiae]], [[Osler's nodes]], [[Janeway lesions]] (suggestive of [[infective endocarditis]]) | |||
---- | |||
'''Chronic mitral regurgitation:''' | |||
❑ [[Asymptomatic]] | |||
:❑ Typical in isolated mild to moderate [[MR]] | |||
:❑ Severe MR until there is [[left ventricular failure]], [[pulmonary hypertension]] or [[atrial fibrillation]] | |||
❑ '''Symptoms associated with decreased forward flow and increased backflow across mitral valve (left ventricular failure):'''<br> | |||
:❑ [[Exertional dyspnea]]<br> | |||
:❑ [[Orthopnea]]<br> | |||
:❑ [[Paroxysmal nocturnal dyspnea]]<br> | |||
:❑ [[Exercise intolerance]]<br> | |||
:❑ [[Fatigue]]<br> | |||
:❑ [[Light-headedness]]<br> | |||
:❑ [[syncope|Exertional syncope]]<br> | |||
:❑ [[angina|Exertional angina]]<br> | |||
:❑ [[Cough]]<br> | |||
❑ '''Symptoms associated with complications:'''<br> | |||
:❑ [[Palpitations]] (suggestive of [[atrial fibrillation]])<br> | |||
:❑ [[Hoarseness]] ([[recurrent laryngeal nerve]] compression due to [[left atrium]] enlargement) <br> | |||
:❑ [[Fever]] (suggestive of [[infective endocarditis]])<br> | |||
:❑ [[Stroke]] (suggestive of [[thromboembolism]])<br> | |||
:❑ [[Hemoptysis]] (suggestive of [[thromboembolism]])<br> | |||
:❑ [[Flank pain]] and [[hematuria]] (suggestive of [[emboli|septic emboli]] or [[glomerulonephritis]])<br> | |||
:❑ [[Seizures]] (suggestive of [[thromboembolism]])<br> | |||
:❑ Symptoms of [[right heart failure]]:<br> | |||
::❑ [[Ascites]] | |||
::❑ [[edema|Pedel edema]] | |||
::❑ [[Abdominal pain]] ([[hepatomegaly]]) | |||
</div>}} | |||
{{family tree| | | | | | | |!| | | | | | }} | |||
{{family tree| | | | | | | B01 | | | | | B01= <div style="float: left; text-align: left; width:25em; padding:1em;">'''Obtain a detailed history:'''<br> | |||
❑ Past medical history: | |||
:❑ [[Congenital heart disease]] | |||
:❑ [[Rheumatic heart disease]] | |||
:❑ [[Ischemic heart disease]] | |||
:❑ [[Valvular heart disease]] | |||
:❑ [[Cardiomyopathy]] | |||
:❑ [[Cardiac surgery]] | |||
:❑ [[Hypertension]] | |||
:❑ [[Diabetes mellitus]] | |||
:❑ [[Radiation exposure]] | |||
:❑ [[Collagen vascular disease]] | |||
:❑ [[Chest trauma]] | |||
❑ Family history: | |||
:❑ [[Valvular heart disease]] | |||
❑ [[Medications]]: | |||
:❑ [[Obesity medical therapy|Anorectic drug combinations]] | |||
:❑ [[Ergotamine]] | |||
:❑ [[Pergolide]] | |||
:❑ [[Cabergoline]] | |||
</div>}} | |||
{{family tree| | | | | | | |!| | | | | | }} | |||
{{family tree| | | | | | | B01 | | | | | B01= <div style="float: left; text-align: left; width:25em; padding:1em;">'''Examine the patient:'''<br> | |||
'''Vital signs:''' <br> | |||
❑ [[Pulse]] | |||
:❑ Rapid and thready (in [[MR|acute MR]]) | |||
:❑ Low volume with brisk upstroke (in [[MR|chronic MR]]) | |||
:❑ [[Irregularly irregular pulse]] (with onset of [[AF]])<br> | |||
❑ [[Blood pressure]] | |||
:❑ [[Hypotension]] (in [[MR|acute MR]]) | |||
:❑ Normotensive (in [[MR|chronic MR]] with preserved [[ejection fraction]]) | |||
❑ [[Temperature]] | |||
:❑ [[Fever]] (suggestive of [[infective endocarditis]]) | |||
❑ [[Respiratory rate]] | |||
:❑ [[Tachypnea]] (typical)<br> | |||
'''Skin:'''<br> | |||
❑ Cool and clammy (in [[cardiogenic shock]])<br> | |||
❑ [[Cyanosis]]<br> | |||
❑ [[edema|Peripheral edema]] (suggestive of [[right heart failure]])<br> | |||
'''Cardiovascular system:''' <br> | |||
'''Palpation:''' <br> | |||
❑ [[Apical impulse]] | |||
:❑ Leftward displacement (in [[MR|chronic MR]] due enlargement of the [[left ventricle]]) <br> | |||
:❑ Hyperdynamic but in normal location (in [[MR|acute MR]]) <br> | |||
❑ [[Thrill]] (in [[MR|acute MR]] and severe [[MR|chronic MR]])<br> | |||
❑ Elevated [[jugular venous pulse]] | |||
:❑ Sign of elevated right sided pressure <br> | |||
:❑ Seen in [[MR|acute MR]] and severe [[MR|chronic MR]]<br> | |||
'''Auscultation:''' <br> | |||
❑ Heart sounds | |||
:❑ [[S1]] is diminished (suggestive of [[MR]]) | |||
:❑ Wide splitting of [[S2]] (low forward flow causing early [[A2]]) | |||
:❑ Loud and delayed [[P2]] (suggestive of [[pulmonary hypertension]]) | |||
:❑ New [[S3]] (suggestive of left ventricular dilation) | |||
❑ [[Murmur]] | |||
:❑ High pitched and blowing [[holosystolic murmur]] (typical) | |||
:❑ Best heard over the [[apex]] radiating to the [[axilla]] and back | |||
:❑ Starts after [[S1]] and continues up to and sometime beyond and obscuring [[A2]] | |||
:❑ Other types of murmur | |||
::❑ Silent (in cases of [[MR|acute MR]]) | |||
::❑ Mid to late systolic murmur (in case of [[papillary muscle]] prolapse) | |||
::❑ Early diastolic murmur (due to large diastolic flow across severe [[MR]]) | |||
::❑ Mid systolic click (suggestive of [[mitral valve prolapse]]) | |||
'''Respiratory system:''' <br> | |||
❑ [[Crackles]] or [[rales]] (suggestive of [[pulmonary edema]]) <br> | |||
❑ [[Tachypnea]]<br> | |||
'''Abdominal system:''' <br> | |||
❑ Hepatojugular reflex<br> | |||
❑ [[Hepatomegaly]] <br> | |||
❑ [[Ascites]]<br> | |||
'''Neurological system:''' <br> | |||
❑ [[Stroke]] (in case of [[thromboembolism]]) | |||
</div>}} | |||
{{Family tree| | | | | | | |!| | | | | | }} | |||
{{Family tree| | | | | | | D01 | | | | | D01= <div style="float: left; text-align: left; width:25em; padding:1em;">'''Order [[electrocardiogram]] (urgent):''' | |||
❑ In [[MR|acute MR]]<br> | |||
:❑ Mostly normal | |||
:❑ Findings of [[ST elevation myocardial infarction electrocardiogram|myocardial infarction]] | |||
❑ In [[MR|chronic MR]] | |||
:❑ Findings of [[Electrocardiographic findings in left ventricular hypertrophy|left ventricular hypertrophy with strain]] | |||
:❑ Findings of [[Left atrial enlargement electrocardiogram|left atrial enlargement]] | |||
:❑ Findings of [[Pulmonary hypertension electrocardiogram|pulmonary hypertension]] | |||
:❑ Findings of [[Atrial fibrillation electrocardiogram|atrial fibrillation]] complication | |||
[[Image:P mitrale.gif|center|150px|thumb|Left atrial enlargement produces a broad, bifid P wave in lead II ('''P mitrale''')]] | |||
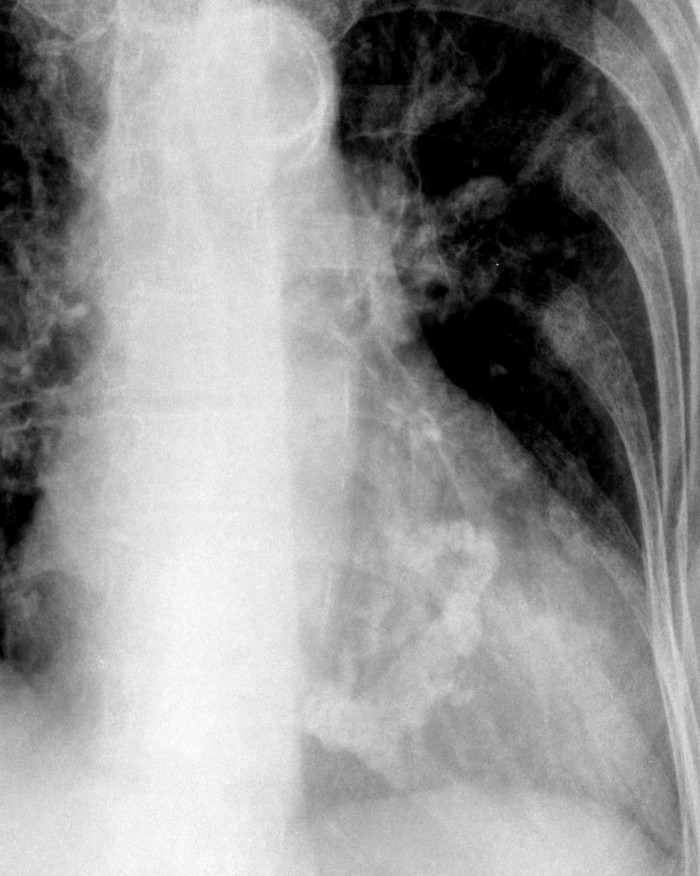
'''Order [[chest X-ray]] (urgent):'''<br> | |||
❑ [[MR|Acute MR]]<br> | |||
:❑ Normal size cardiac silhouette | |||
:❑ Signs of [[pulmonary edema]] | |||
❑ [[MR|Chronic MR]] <br> | |||
:❑ [[Cardiomegaly]] | |||
:❑ Signs of [[pulmonary edema]] if [[left ventricle]] fails | |||
:❑ Calcification of the [[mitral valve annulus]] | |||
[[Image:mitral-valve02.jpg|150px|center|thumb|Calcification of the mitral annulus around the margins of the posterior leaflet forming a “C”]]<br clear="left"/> | |||
'''Order [[transthoracic echocardiography]] ([[TTE]]) (urgent):'''<br> | |||
❑ Confirmatory<br> | |||
❑ To determine severity and assess hemodynamic consequences <br> | |||
❑ To establish etiology<br> | |||
❑ To determine prognosis and evaluate for timing of intervention | |||
'''Order lab tests:'''<br> | |||
❑ [[CBC]]<br> | |||
❑ [[Electrolytes]] <br> | |||
❑ [[ESR]]<br> | |||
❑ [[Troponin|Serum cardiac troponin I and T]] <br> | |||
❑ [[Creatine kinase]] (CK-MB) <br> | |||
❑ [[Blood cultures]] (in case of fever) <br> | |||
❑ Serum [[urea]] and [[creatinine]] <br> | |||
'''Other tests:'''<br> | |||
❑ [[Transesophageal echocardiography]] ([[TEE]] if [[TTE]] is equivocal)<br> | |||
❑ [[Cardiac catheterization]]:<br> | |||
:❑ In stable [[MR|acute MR]] to detect coronary obstruction | |||
:❑ To assess hemodynamic status in symptomatic patients when noninvasive tests are inconclusive | |||
:❑ To assess the severity when there is discrepancy between noninvasive testing and physical examination | |||
❑ Exercise testing: <br> | |||
:❑ Done in asymptomatic severe [[MR]] | |||
:❑ To confirm the absence of symptoms | |||
:❑ To assess the hemodynamic response to exercise | |||
❑ [[MRI|Cardiac MRI]]<br> | |||
:❑ To assess severity when there is a discrepancy between clinical findings and [[echocardiography]]</div>}} | |||
{{familytree | | | | | | | |!| | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | | | A01 | | | | | | | | | | | | | | | | | | | | A01='''Does the patient has acute or chronic [[MR]]?'''}} | |||
{{Family tree| | | |,|-|-|-|^|-|-|-|.| | }} | |||
{{Family tree| | | F01 | | | | | | F02 | | | F01=<div style="float: left; text-align: left; width:25em; padding:1em;">'''Acute MR (Cardinal findings suggestive of [[MR|acute mitral regurgitation]])'''<br> | |||
❑ Sudden onset and rapid progression of [[pulmonary edema]]<br> | |||
❑ [[Cardiogenic shock physical examination|Signs and symptoms of cardiogenic shock]] <BR> | |||
❑ Silent to [[holosystolic murmur]] on auscultation <br> | |||
❑ Normal [[ECG]] <br> | |||
❑ Normal size cardiac silhouette on [[chest X-ray]]<br> | |||
❑ [[Echocardiography]] findings: <br> | |||
:❑ Acute severe [[mitral regurgitation]] | |||
:❑ Normal left ventricular size | |||
:❑ Reduced EF | |||
:❑ Ruptured mitral [[chordae tendinae]] (flail leaflet) | |||
:❑ Ruptured [[papillary muscle]]</div>| F02=<div style="float: left; text-align: left; width:25em; padding:1em;">'''Chronic MR (cardinal findings suggestive of [[MR|chronic mitral regurgitation]])'''<br> | |||
❑ Asymptomatic to chronic symptoms<br> | |||
❑ Pre-existing [[heart disease]]<br> | |||
❑ Classic [[holosystolic murmur]] on auscultation <br> | |||
❑ [[ECG]] findings of [[Electrocardiographic findings in left ventricular hypertrophy|left ventricular hypertrophy with strain]] and [[Left atrial enlargement electrocardiogram|left atrial enlargement]]<br> | |||
❑ [[Cardiomegaly]] on [[chest X-ray]]<br> | |||
❑ [[Echocardiography]] findings:<br> | |||
:❑ [[Mitral regurgitation]] | |||
:❑ [[Left ventricular dilation]] | |||
:❑ Preserved to decreased [[EF]]</div>}} | |||
{{familytree | | | | | | | | | | | |!| | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | | | | | | | F02 | | | | | | | | | | | | | | | | | | | | | F02='''Does the [[mitral valve]] anatomy appear normal in [[TTE]]?'''}} | |||
{{Family tree| | | | | | | | | |,|-|^|-|.| |}} | |||
{{familytree | | | | | | | | | G01 | | G02 | | | | | | | | | | | | | | | | | | | G01=Yes| G02=No}} | |||
{{familytree | | | | | | | | | |!| | | |!| | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | | | | | G01 | | G02 | | | | | | | | | | | | | | | | | | | G02=Chronic primary [[mitral regurgitation]]| G01=Chronic secondary [[mitral regurgitation]]}} | |||
{{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree/end}} | |||
==Treatment== | |||
===Treatment of Acute Mitral Regurgitation=== | |||
Shown below is an algorithm summarizing the approach to the management of acute mitral regurgitation.<ref name="pmid19564568">{{cite journal| author=Stout KK, Verrier ED| title=Acute valvular regurgitation. | journal=Circulation | year= 2009 | volume= 119 | issue= 25 | pages= 3232-41 | pmid=19564568 | doi=10.1161/CIRCULATIONAHA.108.782292 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19564568 }} </ref><ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref>.<br> | |||
<span style="font-size:85%">'''Abbreviations:''' '''IE''': Infective endocarditis; '''LV''': Left ventricle; '''LVEF''': Left ventricular ejection fraction; '''MR''': Mitral regurgitation </span> <br> | |||
{{familytree/start |summary=PE diagnosis Algorithm.}} | |||
{{familytree | | | | | | | | | | | | | B01 | | | | | | | | | | | | | | | | | | | | | | | |B01=<div style="float: left; text-align: left; padding:1em;">'''Does the patient has any signs of hemodynamic instability?''' <br> | |||
❑ [[Hypotension]]<br> | |||
❑ [[Cold extremities]]<br> | |||
❑ [[Cyanosis|Peripheral cyanosis]]<br> | |||
❑ [[Altered mental status]]<br> | |||
</div>}} | |||
{{familytree | | | | | | | | | | |,|-|-|^|-|-|.| | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | | | | | | C01 | | | | C02 | | | | | | | | | | | | | | | | | | | | |C01='''Yes'''|C02='''No'''}} | |||
{{familytree | | | | | | | | | | |!| | | | | |!| | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | | | | | | D01 | | | | D02 | | | | | | | | | | | | | | | | | | | | |D01=<div style="float: left; text-align: left; width:18em; padding:1em;"> '''Initiate resuscitative measures:'''<br> | |||
❑ Secure airway <br> | |||
❑ Administer O2 <br> | |||
❑ Establish 2 wide bore IV access <br> | |||
❑ Establish an arterial line<br> | |||
❑ Connect to [[ECG]] monitor<br> | |||
❑ Monitor vitals continuously<br> | |||
❑ Consider [[ICU]] admission<br> | |||
❑ Consider [[mechanical ventilation]]<br> | |||
❑ Consider [[pulmonary artery catheterization]] | |||
---- | |||
'''Stabilize the patient:'''<br> | |||
❑ Initiate medical stabilization: | |||
:❑ [[Vasodilator]] (IV [[nitroprusside]]) '''PLUS''' inotropic agents (IV [[dobutamine]]) <br> | |||
❑ Establish [[intra-aortic balloon pump]]:<br> | |||
:❑ If medical therapy is not effective to maintain hemodynamic stability<br> | |||
</div>| D02=<div style="float: left; text-align: left; width:18em; padding:1em;"> '''Initiate resuscitative measures:'''<br> | |||
❑ Administer O2 <br> | |||
❑ Establish 2 wide bore IV access <br> | |||
❑ Connect to ECG monitor<br> | |||
❑ Monitor vitals continuously<br> | |||
---- | |||
'''Initiate medical therapy:'''<br> | |||
❑ [[Vasodilator]] therapy: IV [[nitroprusside]]<br></div>}} | |||
{{familytree | | | | | | | | | | |`|-|-|v|-|-|'| | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | |,|-|-|-|-|-|-|-|+|-|-|-|-|-|-|-|.| | | | | | | | | | | | | }} | |||
{{familytree | | | | | I01 | | | | | | I02 | | | | | | I03 | | | | | | | | | | | I02=[[Ischemic mitral regurgitation]]| I03= [[MR]] due to heart failure exacerbation(functional [[MR]])|I01= [[MR]] due to [[IE]] (organic [[MR]])}} | |||
{{familytree | | | | | |!| | | | | | | |!| | | | | | | |!| | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | E01 | | | | | | E02 | | | | | | E03 | | | | | | | | | | | | | | | | |E02=<div style="float: left; text-align: left; width:12em; padding:1em;"> '''Perform reperfusion or revascularization surgery:'''<br> | |||
❑ [[CABG]] or [[coronary angioplasty]] should be done to treat [[acute coronary syndrome]] <br> | |||
❑ Early reperfusion can reduce localized [[LV]] remodeling and hence [[MR]]<br> | |||
</div>| E03=<div style="float: left; text-align: left; width:12em; padding:1em;">'''Initiate treatment for heart failure:''' <br> | |||
❑ Click [[Acute heart failure resident survival guide|here]] for acute heart failure resident survival guide | |||
:❑ [[ACE inhibitors]] or ([[ARBs]]) if LVEF is ≤ 40% | |||
:❑ [[Beta blockers]] | |||
:❑ Intravenous inotropic drugs ([[dobutamine]]) | |||
:❑ [[Diuretic ]]therapy | |||
:❑ IV [[vasodilators]] | |||
</div>| E01=<div style="float: left; text-align: left; width:12em; padding:1em;"> | |||
'''Initiate IE medical therapy:'''<br> | |||
---- | |||
❑ Click [[infective endocarditis resident survival guide|'''here''']] for [[infective endocarditis]] resident survival guide and antimicrobial treatment<br> | |||
</div>}} | |||
{{familytree | | | | | |!| | | | | | | |!| | | | | | | |!| | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | A01 | | | | | | A02 | | | | | | A03 | | | | | | | | | | | | | | A02='''Does the patient has any indications for mitral valve surgery?'''<br> | |||
❑ [[Papillary muscle rupture]]<br> | |||
❑ [[Chordae tendinae rupture]]<br> | |||
❑ Moderate to severe [[ischemic MR]] who are undergoing [[CABG]]<br>| A03='''Does the patient show any hemodynamic improvement to medical therapy?''' | A01='''Does the patient has any indications for mitral valve surgery?'''<br> | |||
❑ Hemodynamic instability<br> | |||
❑ Persistent [[heart failure]]<br> | |||
❑ [[Pulmonary hypertension]]<br> | |||
❑ Early [[mitral valve]] closure<br> }} | |||
{{familytree | | | |,|-|^|-|.| | | |,|-|^|-|.| | | |,|-|^|-|.| | | | | | | | | | | | | | }} | |||
{{familytree | | | A01 | | A02 | | A03 | | A04 | | A05 | | A06 | | | | | | | | | | | | A01=Yes|A02=No|A03=Yes|A04=No|A05=Yes|A06=No}} | |||
{{familytree | | | |!| | | |!| | | |!| | | |!| | | |!| | | |!| | | | | | | | | | | | | }} | |||
{{familytree | | | A01 | | A02 | | A03 | | A04 | | A05 | | A06 | | | | | | | | | | | | A03=<div style="float: left; text-align: left; padding:1em;"> '''Perform mitral valve surgery:'''<br> | |||
❑ Done at the time of reperfusion<br> | |||
❑ [[Mitral valve repair]]: <br> | |||
:❑ Most preferred | |||
❑ [[Mitral valve replacement]]: Preferred in the following groups | |||
:❑ In centers with surgeons who do not have expertise in mitral valve repair techniques | |||
:❑ Very ill patients presenting after an acute [[MI]] | |||
:❑ Complex MR | |||
:❑ In cases of lateral [[LV]] wall motion abnormality | |||
</div>| A04=<div style="float: left; text-align: left; padding:1em;"> | |||
'''Consider medical therapy:'''<br> | |||
❑ In cases of reduced LVEF (ischemic cardiomyopathy)<br> | |||
❑ Medications: <br> | |||
:❑ [[Angiotensin converting enzyme inhibitors]] | |||
:❑ [[Angiotensin II receptor blockers]]<br> | |||
:❑ [[Beta blockers]] | |||
---- | |||
'''Consider cardiac transplantation:'''<br> | |||
❑ On some occasions in patients with severe [[LV]] dysfunction with no contraindication for surgery<br> | |||
</div>| A05= Continue with the [[heart failure]] management and have appropriate follow ups to assess the severity of [[MR]]| A06=<div style="float: left; text-align: left; padding:1em;"> '''Consider mitral valve surgery:'''<br> | |||
❑ [[Mitral valve repair]]: <br> | |||
:❑ Most preferred | |||
❑ [[Mitral valve replacement]]: | |||
:❑ In centers with surgeons who do not have expertise in mitral valve repair techniques | |||
:❑ In cases of lateral [[LV]] wall motion abnormality | |||
</div>|A01=<div style="float: left; text-align: left; width: 16em; padding:1em;"> '''Perform mitral valve surgery:'''<br> | |||
❑ [[Mitral valve replacement]]: | |||
:❑ Mostly done | |||
:❑ Due to extensive tissue destruction in [[IE]] patients | |||
❑ [[Mitral valve repair]]: <br> | |||
:❑ If less [[mitral valve]] destruction | |||
</div>|A02=<div style="float: left; text-align: left; padding:1em;"> | |||
❑ Continue with medical management<br> </div>}} | |||
{{familytree | | | |`|-|v|-|'| | | |!| | | | | | | | | | | |!| | | | | | | | | | | | | }} | |||
{{familytree | | | | | A01 | | | | A04 | | | | | | | | | | A06 | | | | | | | | | | | | A01=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Initiate anticoagulation therapy:'''<br> | |||
---- | |||
❑ For patients undergoing [[mitral valve replacement]]<br> | |||
❑ [[Warfarin]]: Target INR 3 <br> | |||
❑ [[Aspirin]]: 75 to 100 mg/day | |||
---- | |||
'''Educate the patient about [[Endocarditis antibiotic prophylaxis|IE prophylaxis]]:'''<br> | |||
❑ For all patients <br> | |||
❑ Indicated for the following procedures: | |||
:❑ [[Endocarditis antibiotic prophylaxis#Basis for AHA Recommendations Regarding Antibiotic Prophylaxis for Dental Procedures|Dental procedures]] | |||
:❑ [[Endocarditis antibiotic prophylaxis#Antibiotic Prophylaxis For Respiratory Tract Procedures|Respiratory tract procedures]] | |||
:❑ [[Endocarditis antibiotic prophylaxis#Antibiotic Prophylaxis for Gastrointestinal (GI) and Genitourinary (GU) Procedures|GI and GU procedures]] | |||
</div>|A04=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Initiate anticoagulation therapy:'''<br> | |||
---- | |||
❑ For patients undergoing [[mitral valve replacement]]<br> | |||
❑ [[Warfarin]]: Target INR 3 <br> | |||
❑ [[Aspirin]]: 75 to 100 mg/day | |||
---- | |||
'''Educate the patient about [[Endocarditis antibiotic prophylaxis|IE prophylaxis]]:'''<br> | |||
❑ For patients who undergo [[mitral valve replacement]]<br> | |||
❑ Indicated for the following procedures: | |||
:❑ [[Endocarditis antibiotic prophylaxis#Basis for AHA Recommendations Regarding Antibiotic Prophylaxis for Dental Procedures|Dental procedures]] | |||
:❑ [[Endocarditis antibiotic prophylaxis#Antibiotic Prophylaxis For Respiratory Tract Procedures|Respiratory tract procedures]] | |||
:❑ [[Endocarditis antibiotic prophylaxis#Antibiotic Prophylaxis for Gastrointestinal (GI) and Genitourinary (GU) Procedures|GI and GU procedures]] | |||
</div>|A06=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Initiate anticoagulation therapy:'''<br> | |||
---- | |||
❑ For patients undergoing [[mitral valve replacement]]<br> | |||
❑ [[Warfarin]]: Target INR 3 <br> | |||
❑ [[Aspirin]]: 75 to 100 mg/day | |||
---- | |||
'''Educate the patient about [[Endocarditis antibiotic prophylaxis|IE prophylaxis]]:'''<br> | |||
❑ For patients who undergo [[mitral valve replacement]]<br> | |||
❑ Indicated for the following procedures: | |||
:❑ [[Endocarditis antibiotic prophylaxis#Basis for AHA Recommendations Regarding Antibiotic Prophylaxis for Dental Procedures|Dental procedures]] | |||
:❑ [[Endocarditis antibiotic prophylaxis#Antibiotic Prophylaxis For Respiratory Tract Procedures|Respiratory tract procedures]] | |||
:❑ [[Endocarditis antibiotic prophylaxis#Antibiotic Prophylaxis for Gastrointestinal (GI) and Genitourinary (GU) Procedures|GI and GU procedures]] | |||
</div>}} | |||
{{familytree/end}} | |||
===Treatment of Chronic Mitral Regurgitation=== | |||
====Chronic Primary Mitral Regurgitation==== | |||
Shown below is an algorithm summarizing the approach to the management of chronic primary mitral regurgitation.<ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref>.<br> | |||
<span style="font-size:85%">'''Abbreviations:''' '''AF''': Atrial fibrillation; '''IE''': Infective endocarditis; '''LVEF''': Left ventricular ejection fraction; '''LVESD''': Left ventricular end systolic dimension; '''MR''': Mitral regurgitation; '''MVP''': Mitral valve proplapse; '''PASP''': Pulmonary artery systolic pressure; '''RHD''': Rheumatic heart disease </span> <br> | |||
{{familytree/start |summary=PE diagnosis Algorithm.}} | |||
{{familytree | | | | | | | | | A01 | | | | | | | | | | | | | | | | | | | | | | | A01=Determine the severity of [[MR]] on [[TTE]]}} | |||
{{familytree | | | | |,|-|-|-|-|^|-|-|-|-|.| | | | | | | | | | | | | | | | | | |}} | |||
{{familytree | | | | C01 | | | | | | | | C02 | | | | | | | | | | | | | | | | | | | | | | C01=<div style="float: left; text-align: left; width: 18em; padding:1em;">'''Severe [[MR]]''': <br> | |||
❑ Severe [[MVP]] with loss of coaptation<br> | |||
❑ [[Rheumatic fever|RHD]] with loss of central coaptation<br> | |||
❑ [[Left ventricular dilation]]<br> | |||
❑ Regurgitation fraction ≥ 50%<br> | |||
❑ Regurgitation volume ≥ 60ml<br> | |||
❑ Effective regurgitation orifice ≥ 0.4cm²<br> | |||
❑ Vena contracta ≥ 0.7cm | |||
</div>| C02=<div style="float: left; text-align: left; width: 18em; padding:1em;">'''Progressive [[MR]]''' ('''Stage B'''): <br> | |||
❑ Severe [[MVP]] with normal coaptation<br> | |||
❑ [[Rheumatic fever|RHD]] with normal coaptation<br> | |||
❑ No [[Left ventricular dilation]]<br> | |||
❑ Regurgitation fraction < 50%<br> | |||
❑ Regurgitation volume < 60ml<br> | |||
❑ Effective regurgitation orifice < 0.4cm²<br> | |||
❑ Vena contracta < 0.7cm | |||
</div>}} | |||
{{familytree | | |,|-|^|-|-|-|.| | | | | |!| | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | C01 | | | | C02 | | | | |!| | | | | | | | | | | | | | | | | | | | | | | C01=Symptomatic ('''Stage D''')| C02=Asymptomatic ('''Stage C''')}} | |||
{{familytree | | |!| | | | | |!| | | | | |!| | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | |!| | | | | C02 | | | | |!| | | | | | | | | | | | | | | | | | | | | C02=<div style="float: left; text-align: left; width: 18em; padding:1em;">'''Does the patient has any indications for mitral valve surgery?'''<br> | |||
❑ [[LVEF]] 30 to ≤60% '''OR''' [[LVESD]] ≥ 40mm (Stage C2)<br> | |||
❑ [[LVEF]] >60% '''AND''' LVESD < 40mm (Stage C1)<br> | |||
:❑ With likelihood of successful repair > 95% | |||
:❑ With expected mortality < 1% | |||
❑ New onset [[AF]] '''OR''' PASP > 50mmHg (Stage C1) | |||
:❑ With likelihood of successful repair > 95% | |||
:❑ With expected mortality < 1% </div>}} | |||
{{familytree | | |!| | | |,|-|^|-|.| | | |!| }} | |||
{{familytree | | |!| | | C01 | | C02 | | |!| | | | | | | | | | | | | | | | | | | | | C01=Yes|C02=No}} | |||
{{familytree | | |!| | | |!| | | |!| | | |!| | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | C01 | | C02 | | C03 | | C04 | | | | | | | | | | | | | C01=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Initiate medical therapy:'''<br> | |||
❑ [[Vasodialators]]:<br> | |||
:❑ Intravenous [[nitroprusside]] | |||
:❑ [[Hydralazine]] | |||
❑ [[Beta blocker]]<br> | |||
❑ [[Diuretics]]<br> | |||
❑ [[Calcium channel blocker]]<br> | |||
---- | |||
'''Perform mitral valve surgery:'''<br> | |||
❑ [[Mitral valve repair]]: <br> | |||
:❑ Mostly preferred | |||
❑ [[Mitral valve replacement]]: | |||
:❑ In centers with surgeons who do not have expertise in mitral valve repair techniques | |||
:❑ [[Mechanical valve]] in patients <65 years who have long-standing [[AF]] | |||
:❑ [[Bioprosthetic valves]] in patients with contraindications to [[warfarin]] | |||
---- | |||
'''Perform revascularisation:'''<br> | |||
❑ In cases with concurrent [[coronary artery disease]]<br> | |||
❑ Revascularized at the time of [[mitral valve surgery]]<br> | |||
</div>|C02=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Perform mitral valve surgery:'''<br> | |||
❑ [[Mitral valve repair]]: <br> | |||
:❑ Mostly preferred | |||
❑ [[Mitral valve replacement]]: | |||
:❑ In centers with surgeons who do not have expertise in mitral valve repair techniques | |||
:❑ [[Mechanical valve]] in patients <65 years who have long-standing [[AF]] | |||
:❑ [[Bioprosthetic valves]] in patients with contraindications to [[warfarin]] | |||
---- | |||
'''Perform revascularization:'''<br> | |||
❑ For patients with concurrent [[coronary artery disease]]<br> | |||
❑ Revascularized at the time of [[mitral valve surgery]]<br> | |||
</div>| C03=<div style="float: left; text-align: left; width: 20em; padding:1em;"> | |||
'''Periodic monitoring:'''<br> | |||
❑ In stage C1 patients with the following: | |||
:❑ With likelihood of successful repair < 95% | |||
:❑ With expected mortality > 1% | |||
❑ Clinical evaluation: | |||
:❑ Every 3-6 months | |||
❑ [[Echocardiography]]: <br> | |||
:❑ Every 6 months | |||
</div>| C04=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Periodic monitoring:'''<br> | |||
---- | |||
❑ Clinical evaluation: | |||
:❑ Every 3-6 months | |||
❑ [[Echocardiography]]: <br> | |||
:❑ Every 6 months | |||
</div>}} | |||
{{familytree | | |!| | | |`|-|v|-|'| | | |!| | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | A01 | | | | B01 | | | | C01 | | | | | | | | | | | | | | | | | | A01=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Initiate anticoagulation therapy:'''<br> | |||
❑ Indications: | |||
:❑ Rheumatic [[mitral valve disease]] who have a history of systemic [[embolism]] | |||
:❑ Left atrial thrombus | |||
:❑ Paroxysmal or chronic [[atrial fibrillation]] | |||
:❑ [[Mitral valve replacement]] | |||
❑ [[Warfarin]]: | |||
:❑ Target INR 2.5 (range 2.0 to 3.0) | |||
:❑ Target INR 3 (for [[prosthetic valve]]) | |||
❑ [[Aspirin]]: <br> | |||
:❑ 75 to 100 mg/day | |||
:❑ For patients with recurrent [[embolism]] despite adequate [[anticoagulation]] | |||
:❑ For patients with [[prosthetic valve]] | |||
---- | |||
'''Educate the patient about [[Endocarditis antibiotic prophylaxis|IE prophylaxis]]:'''<br> | |||
❑ For patients who undergo [[mitral valve replacement]]<br> | |||
❑ Indicated for the following procedures: | |||
:❑ [[Endocarditis antibiotic prophylaxis#Basis for AHA Recommendations Regarding Antibiotic Prophylaxis for Dental Procedures|Dental procedures]] | |||
:❑ [[Endocarditis antibiotic prophylaxis#Antibiotic Prophylaxis For Respiratory Tract Procedures|Respiratory tract procedures]] | |||
:❑ [[Endocarditis antibiotic prophylaxis#Antibiotic Prophylaxis for Gastrointestinal (GI) and Genitourinary (GU) Procedures|GI and GU procedures]] | |||
</div>|B01=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Initiate anticoagulation therapy:'''<br> | |||
❑ Indications: | |||
:❑ Rheumatic [[mitral valve disease]] who have a history of systemic [[embolism]] | |||
:❑ Left atrial thrombus | |||
:❑ Paroxysmal or chronic [[atrial fibrillation]] | |||
:❑ [[Mitral valve replacement]] | |||
❑ [[Warfarin]]: | |||
:❑ Target INR 2.5 (range 2.0 to 3.0) | |||
:❑ Target INR 3 (for [[prosthetic valve]]) | |||
❑ [[Aspirin]]: <br> | |||
:❑ 75 to 100 mg/day | |||
:❑ For patients with recurrent [[embolism]] despite adequate [[anticoagulation]] | |||
:❑ For patients with [[prosthetic valve]] | |||
---- | |||
'''Educate the patient about [[Endocarditis antibiotic prophylaxis|IE prophylaxis]]:'''<br> | |||
❑ For patients who undergo [[mitral valve replacement]]<br> | |||
❑ Indicated for the following procedures: | |||
:❑ [[Endocarditis antibiotic prophylaxis#Basis for AHA Recommendations Regarding Antibiotic Prophylaxis for Dental Procedures|Dental procedures]] | |||
:❑ [[Endocarditis antibiotic prophylaxis#Antibiotic Prophylaxis For Respiratory Tract Procedures|Respiratory tract procedures]] | |||
:❑ [[Endocarditis antibiotic prophylaxis#Antibiotic Prophylaxis for Gastrointestinal (GI) and Genitourinary (GU) Procedures|GI and GU procedures]] | |||
</div>| C01=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Initiate anticoagulation therapy:'''<br> | |||
❑ Indications: | |||
:❑ Rheumatic [[mitral valve disease]] who have a history of systemic [[embolism]] | |||
:❑ Left atrial thrombus | |||
:❑ Paroxysmal or chronic [[atrial fibrillation]] | |||
:❑ [[Mitral valve replacement]] | |||
❑ [[Warfarin]]: | |||
:❑ Target INR 2.5 (range 2.0 to 3.0) | |||
:❑ Target INR 3 (for [[prosthetic valve]]) | |||
❑ [[Aspirin]]: <br> | |||
:❑ 75 to 100 mg/day | |||
:❑ For patients with recurrent [[embolism]] despite adequate [[anticoagulation]] | |||
:❑ For patients with [[prosthetic valve]]</div>}} | |||
{{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree/end}} | |||
====Chronic Secondary Mitral Regurgitation==== | |||
Shown below is an algorithm summarizing the approach to the management of chronic secondary mitral regurgitation.<ref name="pmid24589852">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=Circulation | year= 2014 | volume= | issue= | pages= | pmid=24589852 | doi=10.1161/CIR.0000000000000029 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24589852 }} </ref>.<br> | |||
== | <span style="font-size:85%">'''Abbreviations:''' '''AF''': Atrial fibrillation; '''CAD''': Coronary artery disease; '''HF''': Heart failure; '''IE''': Infective endocarditis; '''LV''': Left ventricle; '''MR''': Mitral regurgitation </span> <br> | ||
{{familytree/start |summary=PE diagnosis Algorithm.}} | |||
{{familytree | | | | | | | | | | | | | | }} | |||
{{familytree | | | | | | | A01 | | | | | | | | | | | | | | | | | | | | | | | |A01= Determine the etiology and initiate specific treatment}} | |||
{{familytree | | | |,|-|-|-|+|-|-|-|.| | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | | A01 | | A02 | | A03 | | | | | | | | | | | | | | | A01=<div style="float: left; text-align: left; width: 18em; padding:1em;">'''Heart failure:''' <br> | |||
❑ Click [[Acute heart failure resident survival guide|here]] for heart failure resident survival guide | |||
:❑ [[ACE inhibitors]] | |||
:❑ [[ARBs]] | |||
:❑ [[Beta blockers]] | |||
:❑ Intravenous inotropic drugs ([[dobutamine]]) | |||
:❑ [[Diuretic]] therapy | |||
:❑ IV [[vasodilators]] | |||
</div>| A02=<div style="float: left; text-align: left; width: 18em; padding:1em;">'''Coronary artery disease:''' <br> | |||
❑ Click [[Chronic stable angina medical therapy|here]] for [[coronary artery disease]] medical therapy | |||
:❑ [[Aspirin]] | |||
:❑ [[ACE inhibitors]] | |||
:❑ [[Beta blockers]] | |||
❑ [[Coronary angiography]] <br> | |||
❑ Click [[Chronic stable angina revascularization|here]] for [[revascularization]] therapy <br> | |||
</div>| A03=<div style="float: left; text-align: left; width: 18em; padding:1em;">'''Functional [[MR]] with ventricular dyssynchrony:'''<br> | |||
❑ [[Cardiac resynchronization therapy]] with biventricular pacing: | |||
:❑ To reduce LV end-systolic and end-diastolic dimensions | |||
:❑ To reduce mitral regurgitant jet area | |||
</div>}} | |||
{{familytree | | | |`|-|-|-|+|-|-|-|'| | | | | | | | | | | | | | }} | |||
{{familytree | | | | | | | A01 | | | | | A01=Assess the severity of [[MR]] on [[TTE]]}} | |||
{{familytree | | | | |,|-|-|^|-|-|.| | | | | | | | | | | | | | | }} | |||
{{familytree | | | | A01 | | | | A02 | | | | | | | | | | | | | | | | | | | | | | A01=<div style="float: left; text-align: left; width: 18em; padding:1em;">'''Severe [[MR]]''': <br> | |||
❑ Regional wall motion abnormalities with severe tethering of mitral leaflet<br> | |||
❑ Annular dilation with severe loss of central coaptation of the mitral leaflets<br> | |||
❑ LV dilation and [[systolic dysfunction]] due to primary myocardial disease<br> | |||
❑ Regurgitation fraction ≥ 50%<br> | |||
❑ Regurgitation volume ≥ 30ml<br> | |||
❑ Effective regurgitation orifice ≥ 0.2 cm²<br> | |||
</div>| A02=<div style="float: left; text-align: left; width: 18em; padding:1em;">'''Progressive [[MR]]:''' <br> | |||
❑ Regional wall motion abnormalities with mild tethering of mitral leaflets<br> | |||
❑ Annular dilation with mild loss of central coaptation of the mitral leaflets<br> | |||
❑ LV dilation and [[systolic dysfunction]] due to primary myocardial disease<br> | |||
❑ Regurgitation fraction < 50%<br> | |||
❑ Regurgitation volume < 30ml<br> | |||
❑ Effective regurgitation orifice < 0.2 cm²<br> | |||
</div>}} | |||
{{familytree | | | | |!| | | | | |!| | | | | | | | | | | | | | | | | | | | | |}} | |||
{{familytree | | | | A01 | | | | A02 | | | | | | | | | | | | | | | | | | | | | A01= '''Does the [[HF]] symptoms due to [[MR]] persist even after [[revascularization]] and medical therapy?'''|A02=[[HF]] and [[coronary ischemia]] symptoms respond to [[revascularization]] and medical herapy}} | |||
{{familytree | | |,|-|^|-|.| | | |!| | | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | A01 | | A02 | | A03 | | | | | | | | | | | | | | | | | | | | | | A01= Yes ('''Stage D''')| A02= No ('''Stage C''')| A03= '''Stage B'''}} | |||
{{familytree | | |!| | | |!| | | |!| | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | A01 | | A02 | | A03 | | | | | | | | | | | | | | | | | | | | | | A01=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Perform mitral valve surgery:'''<br> | |||
❑ [[Mitral valve repair]]: <br> | |||
:❑ Mostly preferred | |||
❑ [[Mitral valve replacement]]: | |||
:❑ In centers with surgeons who do not have expertise in mitral valve repair techniques | |||
:❑ [[Mechanical valve]] in patients <65 years who have long-standing [[AF]] | |||
:❑ [[Bioprosthetic valves]] in patients with contraindications to [[warfarin]] | |||
</div>|A02=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Periodic monitoring:'''<br> | |||
❑ Clinical evaluation: | |||
:❑ Every 3-6 months | |||
❑ [[Echocardiography]]: <br> | |||
:❑ Every 6 months | |||
---- | |||
'''Consider mitral valve surgery:'''<br> | |||
❑ Only for patients undergoing other [[cardiac surgery]]<br> | |||
</div>| A03=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Periodic monitoring:'''<br> | |||
❑ Clinical evaluation: | |||
:❑ Every 3-6 months | |||
❑ [[Echocardiography]]: <br> | |||
:❑ Every 6 months | |||
---- | |||
'''Consider mitral valve surgery:'''<br> | |||
❑ Only for patients undergoing other [[cardiac surgery]]<br> | |||
</div>}} | |||
{{familytree | | |!| | | |!| | | |!| | | | | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree | | A01 | | A02 | | A03 | | | | | | | | | | | | | | | | | | | | | | A01=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Initiate anticoagulation therapy:'''<br> | |||
❑ Indications: | |||
:❑ History of systemic [[embolism]] | |||
:❑ Left atrial thrombus | |||
:❑ Paroxysmal or chronic [[atrial fibrillation]] | |||
:❑ [[Mitral valve replacement]] | |||
❑ [[Warfarin]]: | |||
:❑ Target INR 2.5 (range 2.0 to 3.0) | |||
:❑ Target INR 3 (for [[prosthetic valve]]) | |||
❑ [[Aspirin]]: <br> | |||
:❑ 75 to 100 mg/day | |||
:❑ For patients with recurrent [[embolism]] despite adequate [[anticoagulation]] | |||
:❑ For patients with [[prosthetic valve]] | |||
---- | |||
'''Educate the patient about [[Endocarditis antibiotic prophylaxis|IE prophylaxis]]:'''<br> | |||
❑ For patients who undergo [[mitral valve replacement]]<br> | |||
❑ Indicated for the following procedures: | |||
:❑ [[Endocarditis antibiotic prophylaxis#Basis for AHA Recommendations Regarding Antibiotic Prophylaxis for Dental Procedures|Dental procedures]] | |||
:❑ [[Endocarditis antibiotic prophylaxis#Antibiotic Prophylaxis For Respiratory Tract Procedures|Respiratory tract procedures]] | |||
:❑ [[Endocarditis antibiotic prophylaxis#Antibiotic Prophylaxis for Gastrointestinal (GI) and Genitourinary (GU) Procedures|GI and GU procedures]] | |||
</div>|A02=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Initiate anticoagulation therapy:'''<br> | |||
❑ Indications: | |||
:❑ History of systemic [[embolism]] | |||
:❑ Left atrial thrombus | |||
:❑ Paroxysmal or chronic [[atrial fibrillation]] | |||
❑ [[Warfarin]]: | |||
:❑ Target INR 2.5 (range 2.0 to 3.0) | |||
❑ [[Aspirin]]: <br> | |||
:❑ 75 to 100 mg/day | |||
:❑ For patients with recurrent [[embolism]] despite adequate [[anticoagulation]] | |||
---- | |||
'''Educate the patient about [[Endocarditis antibiotic prophylaxis|IE prophylaxis]]:'''<br> | |||
❑ Only if they undergo [[mitral valve replacement]]<br> | |||
</div>| A03=<div style="float: left; text-align: left; width: 20em; padding:1em;">'''Initiate anticoagulation therapy:'''<br> | |||
❑ Indications: | |||
:❑ History of systemic [[embolism]] | |||
:❑ Left atrial thrombus | |||
:❑ Paroxysmal or chronic [[atrial fibrillation]] | |||
❑ [[Warfarin]]: | |||
:❑ Target INR 2.5 (range 2.0 to 3.0) | |||
❑ [[Aspirin]]: <br> | |||
:❑ 75 to 100 mg/day | |||
:❑ For patients with recurrent [[embolism]] despite adequate [[anticoagulation]] | |||
---- | |||
'''Educate the patient about [[Endocarditis antibiotic prophylaxis|IE prophylaxis]]:'''<br> | |||
❑ Only if they undergo [[mitral valve replacement]]<br> | |||
</div>}} | |||
{{familytree/end}} | |||
== | ==Do's== | ||
* | * Always consult a multidisciplinary heart valve team for patients with acute [[MR]], severe chronic [[MR]] and with multiple comorbidities. | ||
* | * Consider vasodilator therapy in patients with chronic MR based upon the presence or absence of symptoms and the functional state of the [[left ventricle]]. | ||
* | * Always consider patients with chronic [[MR]] who become symptomatic to be candidates for corrective mitral surgery. | ||
* Perform [[mitral valve repair]] for patients with chronic severe primary [[MR]] limited to the posterior leaflet. | |||
* | ==Don'ts== | ||
* Don't initiate [[vasodilator]] therapy for normotensive asymptomatic patients with chronic primary [[MR]] (stages B and C1) and normal systolic LV function. | |||
* Don't recommend cardiovascular magnetic resonance (CMR) for routine diagnosis of [[MR]]. | |||
* Don't prefer [[mitral valve repair]] to replacement to chronic severe primary [[MR]] patients involving the anterior leaflet or both leaflets when a successful and durable repair cannot be accomplished. | |||
* Don't perform mitral valve replacement in patients with isolated severe primary MR limited to less than one half of the posterior leaflet unless mitral valve repair has been attempted and was unsuccessful. | |||
* Don't perform [[coronary angiography]] before valve surgery in patients who are hemodynamically unstable. | |||
* Avoid [[coronary angiography]] in patients of acute coronary syndrome complicated by severe acute [[mitral regurgitation]]. | |||
==References== | ==References== | ||
| Line 30: | Line 814: | ||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Resident survival guide]] | |||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Latest revision as of 13:57, 19 May 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mugilan Poongkunran M.B.B.S [2]
| Mitral Regurgitation Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| FIRE |
| Complete Diagnostic Approach |
| Treatment |
| Do's |
| Don'ts |
Overview
Mitral regurgitation (MR) is a disorder of the heart characterized by failure of the mitral valve to close properly during systole leading to blood leakage from the left ventricle to the left atrium during systole. Individuals with acute mitral regurgitation may present with significant hemodynamic instability due to the sudden drop in cardiac output, leading to acute pulmonary edema, hypotension and possible cardiogenic shock. Individuals with chronic compensated mitral regurgitation may be asymptomatic, with a normal exercise tolerance and no evidence of heart failure, or may present with fatigue, dyspnea on exertion, orthopnea, and paroxysmal nocturnal dyspnea.[1] The management of MR includes afterload reduction with careful monitoring of fluid status, management of the underlying disease (CAD, mitral valve prolapse, rheumatic heart disease), and early surgical intervention in severe cases. Ultimately, the management of MR depends on the anatomy of the mitral valve, the acuteness of the disease process, and the severity of presentation. [2]
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
Acute Mitral Regurgitation
- Papillary muscle rupture:
- Ruptured mitral chordae tendinae:
- Acute rheumatic fever[3]
- Chest trauma[4]
- Mitral valve prolapse[5]
- Infective endocarditis
- Spontaneous rupture
Chronic Primary Mitral Regurgitation
Chronic Secondary Mitral Regurgitation
Click here for the complete list of causes.
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.
Boxes in red color signify that an urgent management is needed.
Abbreviations: ARBs: Angiotensin II receptor antagonist; CABG: Coronary artery bypass surgery; HF: Heart failure; IE: Infective endocarditis; LVEF: Left ventricular ejection fraction; LV: Left ventricle; MR: Mitral regurgitation; S1: First heart sound; S2: Second heart sound
Identify cardinal findings that increase the pretest probability of mitral regurgitation: ❑ Murmur:
❑ Heart sounds: | |||||||||||||||||||||||||||||||||||||||
Does the patient have any of the following findings of acute mitral regurgitation with instability? ❑ Sudden onset and rapid progression of pulmonary edema:
| |||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||
| Continue with complete diagnostic approach below | |||||||||||||||||||||||||||||||||||||||
Initiate resuscitative measures: ❑ Secure airway Order imaging and blood tests (urgent): | |||||||||||||||||||||||||||||||||||||||
| Does the patient has any evidence of MR in TTE? | |||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||
Stabilize the patient:
❑ Establish intra-aortic balloon pump:
Initiate treatment for specific etiologies: | Consider other possible diagnosis: | ||||||||||||||||||||||||||||||||||||||
Does the patient have any findings on TTE that require mitral valve surgery? ❑ Flail mitral leaflet (papillary muscle or chordal rupture)
| |||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||
Perform mitral valve surgery:
| Perform reperfusion or revascularization: ❑ In patients with acute coronary syndrome, CABG or coronary angioplasty should be performed | ||||||||||||||||||||||||||||||||||||||
Perform reperfusion or revascularization: ❑ Perform CABG or coronary angioplasty at the time of mitral valve surgery in patients with myocardial infarction Consider cardiac transplantation: | |||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach to Mitral Regurgitation
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[2].
Abbreviations: AF: Atrial fibrillation; MR: Mitral regurgitation; EKG: Electrocardiogram; EF: Ejection fraction; S1: First heart sound; S2: Second heart sound; S3: Third heart sound; LV: Left ventricle; MVP: Mitral valve prolapse
Characterize the symptoms: Acute mitral regurgitation:
❑ Symptoms of shock and pulmonary edema:
❑ Symptoms suggestive of precipitating events:
Chronic mitral regurgitation: ❑ Asymptomatic
❑ Symptoms associated with decreased forward flow and increased backflow across mitral valve (left ventricular failure):
❑ Symptoms associated with complications:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Obtain a detailed history: ❑ Past medical history:
❑ Family history: ❑ Medications: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient: Vital signs:
Skin: Cardiovascular system:
❑ Thrill (in acute MR and severe chronic MR)
Auscultation:
❑ Murmur
Respiratory system: Abdominal system: Neurological system: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Order electrocardiogram (urgent):
❑ In acute MR
❑ In chronic MR
 Order chest X-ray (urgent):
 Order transthoracic echocardiography (TTE) (urgent): Order lab tests: Other tests:
❑ Exercise testing:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the patient has acute or chronic MR? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Acute MR (Cardinal findings suggestive of acute mitral regurgitation) ❑ Sudden onset and rapid progression of pulmonary edema
| Chronic MR (cardinal findings suggestive of chronic mitral regurgitation) ❑ Asymptomatic to chronic symptoms
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the mitral valve anatomy appear normal in TTE? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Chronic secondary mitral regurgitation | Chronic primary mitral regurgitation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment
Treatment of Acute Mitral Regurgitation
Shown below is an algorithm summarizing the approach to the management of acute mitral regurgitation.[1][2].
Abbreviations: IE: Infective endocarditis; LV: Left ventricle; LVEF: Left ventricular ejection fraction; MR: Mitral regurgitation
Does the patient has any signs of hemodynamic instability? ❑ Hypotension | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Initiate resuscitative measures: ❑ Secure airway Stabilize the patient:
❑ Establish intra-aortic balloon pump:
| Initiate resuscitative measures: ❑ Administer O2 Initiate medical therapy: | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| MR due to IE (organic MR) | Ischemic mitral regurgitation | MR due to heart failure exacerbation(functional MR) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Initiate IE medical therapy: ❑ Click here for infective endocarditis resident survival guide and antimicrobial treatment | Perform reperfusion or revascularization surgery: ❑ CABG or coronary angioplasty should be done to treat acute coronary syndrome | Initiate treatment for heart failure: ❑ Click here for acute heart failure resident survival guide
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the patient has any indications for mitral valve surgery? ❑ Hemodynamic instability | Does the patient has any indications for mitral valve surgery? ❑ Papillary muscle rupture | Does the patient show any hemodynamic improvement to medical therapy? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | Yes | No | Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Perform mitral valve surgery:
|
❑ Continue with medical management | Perform mitral valve surgery: ❑ Done at the time of reperfusion
❑ Mitral valve replacement: Preferred in the following groups | Consider medical therapy: Consider cardiac transplantation: | Continue with the heart failure management and have appropriate follow ups to assess the severity of MR | Consider mitral valve surgery:
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Initiate anticoagulation therapy: ❑ For patients undergoing mitral valve replacement Educate the patient about IE prophylaxis: | Initiate anticoagulation therapy: ❑ For patients undergoing mitral valve replacement Educate the patient about IE prophylaxis: | Initiate anticoagulation therapy: ❑ For patients undergoing mitral valve replacement Educate the patient about IE prophylaxis: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment of Chronic Mitral Regurgitation
Chronic Primary Mitral Regurgitation
Shown below is an algorithm summarizing the approach to the management of chronic primary mitral regurgitation.[2].
Abbreviations: AF: Atrial fibrillation; IE: Infective endocarditis; LVEF: Left ventricular ejection fraction; LVESD: Left ventricular end systolic dimension; MR: Mitral regurgitation; MVP: Mitral valve proplapse; PASP: Pulmonary artery systolic pressure; RHD: Rheumatic heart disease
| Determine the severity of MR on TTE | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Severe MR: ❑ Severe MVP with loss of coaptation | Progressive MR (Stage B): ❑ Severe MVP with normal coaptation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Symptomatic (Stage D) | Asymptomatic (Stage C) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Does the patient has any indications for mitral valve surgery? ❑ LVEF 30 to ≤60% OR LVESD ≥ 40mm (Stage C2)
❑ New onset AF OR PASP > 50mmHg (Stage C1)
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Initiate medical therapy:
❑ Beta blocker Perform mitral valve surgery:
Perform revascularisation: | Perform mitral valve surgery:
Perform revascularization: | Periodic monitoring:
❑ Clinical evaluation:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Initiate anticoagulation therapy: ❑ Indications:
❑ Warfarin:
❑ Aspirin:
Educate the patient about IE prophylaxis: | Initiate anticoagulation therapy: ❑ Indications:
❑ Warfarin:
❑ Aspirin:
Educate the patient about IE prophylaxis: | Initiate anticoagulation therapy: ❑ Indications:
❑ Warfarin:
❑ Aspirin:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Chronic Secondary Mitral Regurgitation
Shown below is an algorithm summarizing the approach to the management of chronic secondary mitral regurgitation.[2].
Abbreviations: AF: Atrial fibrillation; CAD: Coronary artery disease; HF: Heart failure; IE: Infective endocarditis; LV: Left ventricle; MR: Mitral regurgitation
| Determine the etiology and initiate specific treatment | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Heart failure: ❑ Click here for heart failure resident survival guide
| Coronary artery disease: ❑ Click here for coronary artery disease medical therapy ❑ Coronary angiography | Functional MR with ventricular dyssynchrony: ❑ Cardiac resynchronization therapy with biventricular pacing:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Assess the severity of MR on TTE | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Severe MR: ❑ Regional wall motion abnormalities with severe tethering of mitral leaflet | Progressive MR: ❑ Regional wall motion abnormalities with mild tethering of mitral leaflets | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the HF symptoms due to MR persist even after revascularization and medical therapy? | HF and coronary ischemia symptoms respond to revascularization and medical herapy | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes (Stage D) | No (Stage C) | Stage B | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Perform mitral valve surgery:
| Periodic monitoring: ❑ Clinical evaluation:
Consider mitral valve surgery: | Periodic monitoring: ❑ Clinical evaluation:
Consider mitral valve surgery: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Initiate anticoagulation therapy: ❑ Indications:
❑ Warfarin:
❑ Aspirin:
Educate the patient about IE prophylaxis: | Initiate anticoagulation therapy: ❑ Indications:
❑ Warfarin:
❑ Aspirin:
Educate the patient about IE prophylaxis: | Initiate anticoagulation therapy: ❑ Indications:
❑ Warfarin:
❑ Aspirin:
Educate the patient about IE prophylaxis: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Do's
- Always consult a multidisciplinary heart valve team for patients with acute MR, severe chronic MR and with multiple comorbidities.
- Consider vasodilator therapy in patients with chronic MR based upon the presence or absence of symptoms and the functional state of the left ventricle.
- Always consider patients with chronic MR who become symptomatic to be candidates for corrective mitral surgery.
- Perform mitral valve repair for patients with chronic severe primary MR limited to the posterior leaflet.
Don'ts
- Don't initiate vasodilator therapy for normotensive asymptomatic patients with chronic primary MR (stages B and C1) and normal systolic LV function.
- Don't recommend cardiovascular magnetic resonance (CMR) for routine diagnosis of MR.
- Don't prefer mitral valve repair to replacement to chronic severe primary MR patients involving the anterior leaflet or both leaflets when a successful and durable repair cannot be accomplished.
- Don't perform mitral valve replacement in patients with isolated severe primary MR limited to less than one half of the posterior leaflet unless mitral valve repair has been attempted and was unsuccessful.
- Don't perform coronary angiography before valve surgery in patients who are hemodynamically unstable.
- Avoid coronary angiography in patients of acute coronary syndrome complicated by severe acute mitral regurgitation.
References
- ↑ 1.0 1.1 Stout KK, Verrier ED (2009). "Acute valvular regurgitation". Circulation. 119 (25): 3232–41. doi:10.1161/CIRCULATIONAHA.108.782292. PMID 19564568.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. doi:10.1161/CIR.0000000000000029. PMID 24589852.
- ↑ Anderson Y, Wilson N, Nicholson R, Finucane K (2008). "Fulminant mitral regurgitation due to ruptured chordae tendinae in acute rheumatic fever". J Paediatr Child Health. 44 (3): 134–7. doi:10.1111/j.1440-1754.2007.01214.x. PMID 17854408.
- ↑ Grinberg AR, Finkielman JD, Piñeiro D, Festa H, Cazenave C (1998). "Rupture of mitral chorda tendinea following blunt chest trauma". Clin Cardiol. 21 (4): 300–1. PMID 9580528.
- ↑ Grenadier E, Alpan G, Keidar S, Palant A (1983). "The prevalence of ruptured chordae tendineae in the mitral valve prolapse syndrome". Am Heart J. 105 (4): 603–10. PMID 6837414.
- ↑ Otto CM (2001). "Clinical practice. Evaluation and management of chronic mitral regurgitation". N Engl J Med. 345 (10): 740–6. doi:10.1056/NEJMcp003331. PMID 11547744.