Uveitis pathophysiology
|
Uveitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Uveitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Uveitis pathophysiology |
|
Risk calculators and risk factors for Uveitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Tarek Nafee, M.D. [2]
Overview
The exact pathogenesis of uveitis is not fully understood. It is thought that uveitis is mediated by a genetic predisposition and an acquired cross immunity to infectious agents, or cross immunity to self-antigens due to underlying autoimmune diseases. It is estimated that 35% to 50% of cases of uveitis are idiopathic.[1][2] Development of uveitis is hypothesized to be the result of a genetic predisposition for acquiring the disease; contributions of several human leukocyte antigen (HLA) alleles are most commonly implicated.[2][3]
Pathogenesis
The exact pathogenesis of uveitis is not fully understood. It is thought that uveitis is mediated by a genetic predisposition combined with cross immunity to infectious agents, or cross immunity to self-antigens due to underlying autoimmune diseases. It is estimated that 35-50% of cases of uveitis are idiopathic.[1][2] Uveitis, in the setting of underlying infectious diseases, is hypothesized to be secondary to a T-cell mediated hypersensitivity reaction resulting in immunoactivating cytokine production by proliferating Tн17 and Tн1 cells.[3][4] A similar mechanism is hypothesized for autoimmune etiologies of uveitis with the exception of an unknown source of the triggering antigen.[5][6][7][8]
Genetics
Development of uveitis is hypothesized to be the result of a genetic predisposition for acquiring the disease. Contributions of several human leukocyte antigen (HLA) alleles are most commonly implicated. This includes HLA-B27 in seronegative spondyloarthropathies, HLA-A29 in birdshot chorioretinopathy, HLA-B51 in Behcet syndrome and multiple sclerosis, HLA-B8, HLA-DR15, and HLA-DR2.[2][3]
Associated Conditions
The following conditions are associated with uveitis:[1][2][9]
- Seronegative spondyloarthropathy
- Sarcoidosis
- Multiple sclerosis
- Inflammatory bowel disease
- Systemic lupus erythematosus (SLE)
- Behçet's syndrome
- Birdshot retinochoroidopathy
- Juvenile idiopathic arthritis (JIA)
- Vogt-Koyanagi-Harada syndrome
- Fuch's heterochromic iridocyclitis
- Lymphoma
- Lyme Disease
- Acquired immunodeficiency syndrome (AIDS)
- Herpes simplex
- Varicella Zoster
- Cytomegalovirus
- Syphilis
- Toxoplasmosis
- Toxocariasis
- Tuberculosis
- Rubella
- Cat scratch disease (Bartonella spp.)
Gross Pathology
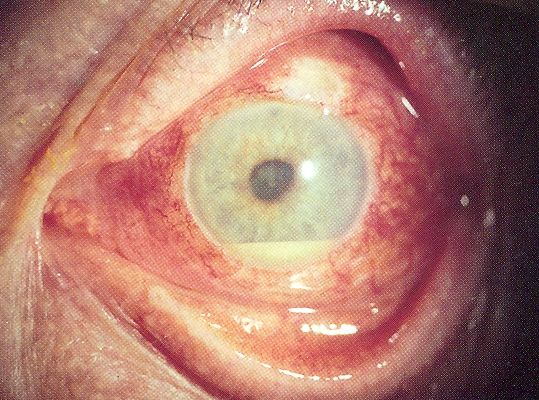
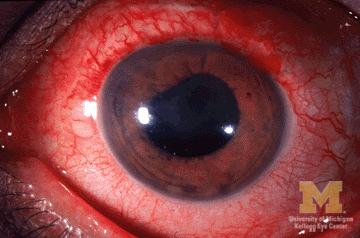
On gross pathology, redness of the eye and dilated cilliary vessels are common yet non-specific findings in uveitis. The following are images of the gross pathology of uveitis:[10][11]
-
Uveitis with pus in the anterior chamber
-
Anterior Uveitis
Microscopic Pathology
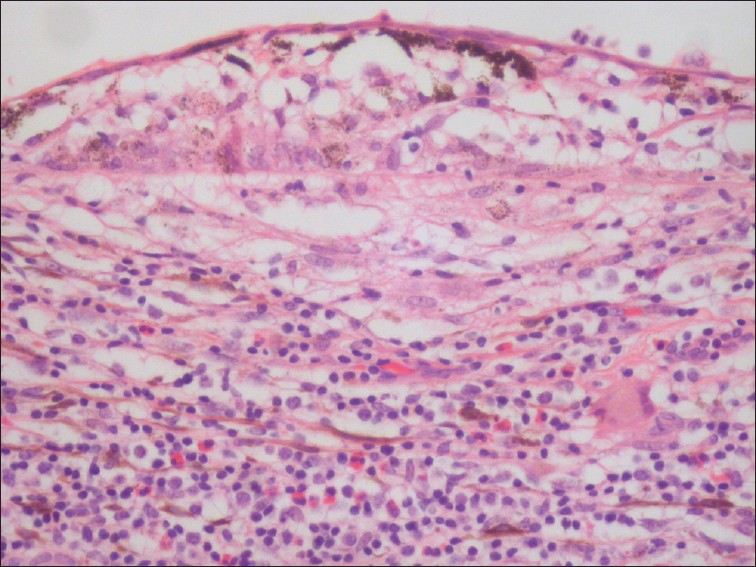
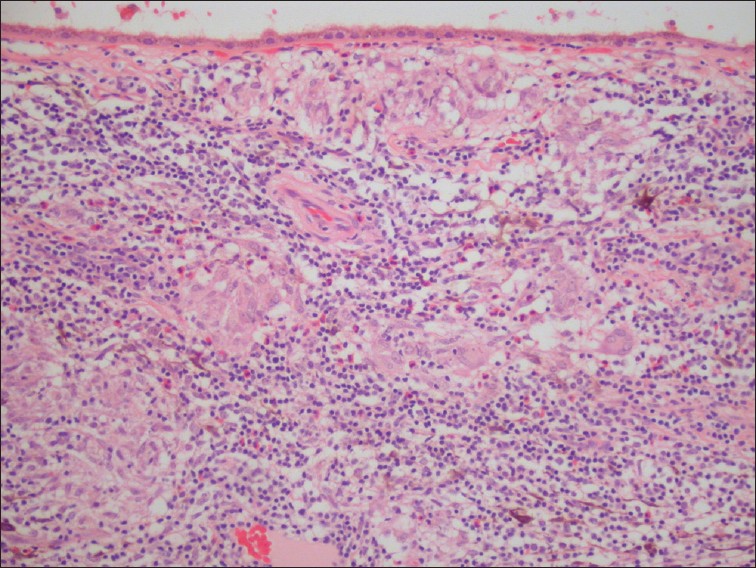
On microscopic histopathological analysis, lymphocytic infiltration, monocytic infiltration, epitheloid cells, and granulomatous inflammation of the uveal structures are characteristic findings of uveitis. The following are images of the microscopic pathology of uveitis:[12]
-
Uveitis with infiltration of lymphocytes
-
Uveitis with granulomatous inflammation and infiltration of the choroid by lymphocytes and macrophages
References
- ↑ Jump up to: 1.0 1.1 1.2 Rodriguez A, Calonge M, Pedroza-Seres M, Akova YA, Messmer EM, D'Amico DJ; et al. (1996). "Referral patterns of uveitis in a tertiary eye care center". Arch Ophthalmol. 114 (5): 593–9. PMID 8619771.
- ↑ Jump up to: 2.0 2.1 2.2 2.3 2.4 Guly CM, Forrester JV (2010). "Investigation and management of uveitis". BMJ. 341: c4976. doi:10.1136/bmj.c4976. PMID 20943722.
- ↑ Jump up to: 3.0 3.1 3.2 Przeździecka-Dołyk J, Węgrzyn A, Turno-Kręcicka A, Misiuk-Hojło M (2016). "Immunopathogenic Background of Pars Planitis". Arch Immunol Ther Exp (Warsz). 64 (2): 127–37. doi:10.1007/s00005-015-0361-y. PMC 4805694. PMID 26438050.
- ↑ Urban B, Bakunowicz-Łazarczyk A, Michalczuk M (2014). "Immune recovery uveitis: pathogenesis, clinical symptoms, and treatment". Mediators Inflamm. 2014: 971417. doi:10.1155/2014/971417. PMC 4096001. PMID 25089078.
- ↑ Sun D, Liang D, Kaplan HJ, Shao H (2015). "The role of Th17-associated cytokines in the pathogenesis of experimental autoimmune uveitis (EAU)". Cytokine. 74 (1): 76–80. doi:10.1016/j.cyto.2014.12.017. PMC 4457592. PMID 25742774.
- ↑ Bi HS, Liu ZF, Cui Y (2015). "Pathogenesis of innate immunity and adaptive immunity in the mouse model of experimental autoimmune uveitis". J Chin Med Assoc. 78 (5): 276–82. doi:10.1016/j.jcma.2015.01.002. PMID 25769932.
- ↑ Horai R, Caspi RR (2011). "Cytokines in autoimmune uveitis". J Interferon Cytokine Res. 31 (10): 733–44. doi:10.1089/jir.2011.0042. PMC 3189550. PMID 21787221.
- ↑ Ke Y, Liu K, Huang GQ, Cui Y, Kaplan HJ, Shao H; et al. (2009). "Anti-inflammatory role of IL-17 in experimental autoimmune uveitis". J Immunol. 182 (5): 3183–90. doi:10.4049/jimmunol.0802487. PMC 3275433. PMID 19234216.
- ↑ American Academy of Ophthalmology EyeWiki(2015)http://eyewiki.aao.org/Category:Uveitis
- ↑ Wikipedia Uveitis(2006)https://en.wikipedia.org/wiki/Uveitis#/media/File:Hypopyon.jpg
- ↑ University of Michigan Eyes Have It(2009)http://kellogg.umich.edu/theeyeshaveit/red-eye/anterior-uveitis.html
- ↑ Arevalo JF, Garcia RA, Al-Dhibi HA, Sanchez JG, Suarez-Tata L (2012). "Update on sympathetic ophthalmia". Middle East Afr J Ophthalmol. 19 (1): 13–21. doi:10.4103/0974-9233.92111. PMC 3277011. PMID 22346110.