T helper cell
|
WikiDoc Resources for T helper cell |
|
Articles |
|---|
|
Most recent articles on T helper cell Most cited articles on T helper cell |
|
Media |
|
Powerpoint slides on T helper cell |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on T helper cell at Clinical Trials.gov Trial results on T helper cell Clinical Trials on T helper cell at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on T helper cell NICE Guidance on T helper cell
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on T helper cell Discussion groups on T helper cell Patient Handouts on T helper cell Directions to Hospitals Treating T helper cell Risk calculators and risk factors for T helper cell
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for T helper cell |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
T helper cells (also known as effector T cells or Th cells) are a sub-group of lymphocytes (a type of white blood cell or leukocyte) that plays an important role in establishing and maximizing the capabilities of the immune system. These cells are unusual in that they have no cytotoxic or phagocytic activity; they cannot kill infected host (also known as somatic) cells or pathogens, and without other immune cells they would usually be considered useless against an infection. Th cells are involved in activating and directing other immune cells, and are particularly important in the immune system. They are essential in determining B cell antibody class switching, in the activation and growth of cytotoxic T cells, and in maximizing bactericidal activity of phagocytes such as macrophages. It is this diversity in function and their role in influencing other cells that gives T helper cells their name.
Mature Th cells are believed to always express the surface protein CD4. T cells expressing CD4 are also known as CD4+ T cells. CD4+ T cells are generally treated as having a pre-defined role as helper T cells within the immune system, although there are known rare exceptions. For example, there are sub-groups of suppressor T cells, natural killer T cells, and cytotoxic T cells that are known to express CD4 (although cytotoxic examples have been observed in extremely low numbers in specific disease states, they are usually considered non-existent). All of the latter CD4+ T cell groups are not considered T helper cells, and are beyond the scope of this article.

The importance of helper T cells can be seen from HIV, a virus that infects cells that are CD4+ (including helper T cells). Towards the end of a HIV infection the number of functional CD4+ T cells falls, which leads to the symptomatic stage of infection known as the acquired immune deficiency syndrome (AIDS). There are also rare disorders, probably genetic in etiology, that result in the absence or dysfunction of CD4+ T cells. These disorders produce similar symptoms, and many of these are fatal (see T-Lymphocytopenia).
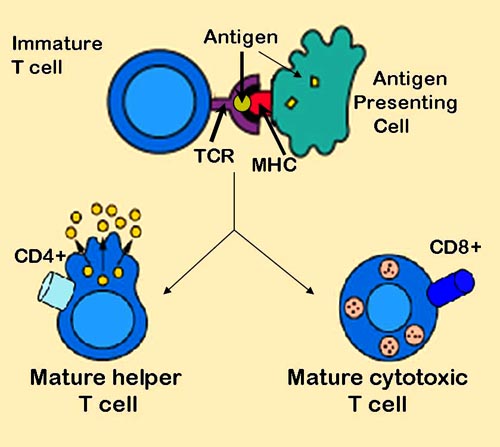
Activation of naïve helper T cells
Following T cell development, matured, naïve (meaning they have never been exposed to the antigen to which they can respond) T cells leave the thymus and begin to spread throughout the body, including the lymph nodes. Like all T cells, they express the T cell receptor/CD3 complex. The T cell receptor (TcR) consists of both constant and variable regions, the latter of which determines what antigen the T cell can respond to. CD4+ T cells have TcRs with an affinity for Class II MHC, and it is believed that CD4 is involved in determining MHC affinity during maturation in the thymus. Class II MHC proteins are generally only found on the surface of professional antigen-presenting cells (APCs). Professional antigen presenting cells are primarily dendritic cells, macrophages and B cells, although dendritic cells are the only cell group that expresses MHC Class II constitutively (at all times). Some APCs also bind native (or unprocessed) antigens to their surface, such as follicular dendritic cells, but unprocessed antigens do not interact with T cells and are not involved in their activation. The antigens that bind to MHC proteins are always short peptides, 8-10 amino acids long for MHC Class I, and up to 25 or so for MHC Class II.
Recognition (Signal 1)
During an immune response, professional antigen-presenting cells (APCs) endocytose (absorb) foreign material (typically bacteria or viruses), which undergoes processing, then travel from the infection site to the lymph nodes. Once at the lymph nodes, the APC begins to present antigen peptides that are bound to Class II MHC, allowing CD4+ T cells that express specific TcR's against the peptide/MHC complex to activate.
When a Th cell encounters and recognises the antigen on an APC, the TcR-CD3 complex binds strongly to the peptide-MHC complex present on the surface of professional APC's. CD4, a co-receptor of the TCR complex, also binds to a different section of the MHC molecule. These interactions bring these proteins closer together, allowing the intracellular kinases present on the TcR, CD3 and CD4 proteins to activate each other via phosphorylation. With the assistance of a phosphatase present on the intracellular section of CD45 (common leukocyte antigen), these molecules activate the major biochemical pathways in the cytosol of the Th cell. These active pathways are known as Signal 1 of T cell activation, as it is the first and primary pro-activation signal in a Th cell. Upon subsequent encounters with a given antigen, memory T cells are re-activated using the same TCR pathways.
The binding of the antigen-MHC to the TCR complex and CD4 may also help the APC and the Th cell adhere during Th cell activation, but the integrin protein LFA-1 on the T cell and ICAM on the APC are the primary molecules of adhesion in this cell interaction.
It is unknown what role the relatively bulky extracellular region of CD45 plays during cell interactions, but CD45 has various isoforms that change in size depending on the Th cell's activation and maturation status. For example, CD45 shortens in length following Th activation (CD45RA+ to CD45RO+), but whether this change in length influences activation is unknown. It has been proposed that the larger CD45RA+ may decrease the accessibility of the T cell receptor for the antigen-MHC molecule, thereby necessitating an increase in the affinity (and specificity) of the T cell for activation. Once the activation has occurred however, CD45 shortens, allowing easier interactions and activation as an effector T helper cell.
Verification (Signal 2)
Having received the first TcR/CD3 signal, the naïve T cell must activate a second independent biochemical pathway, known as Signal 2. This verification step is a protective measure to ensure that a T cell is responding to a foreign antigen. If this second signal is not present during initial antigen exposure, the T cell presumes that it is auto-reactive. This results in the cell becoming anergic (anergy is generated from the unprotected biochemical changes of Signal 1). Anergic cells will not respond to any antigen in the future, even if both signals are present later on. These cells are generally believed to circulate throughout the body with no value until they apoptose at the end of their lifespan.
The second signal involves an interaction between CD28 on the CD4+ T cell and the proteins CD80 (B7.1) or CD86 (B7.2) on the professional APCs. Both CD80 and CD86 activate the CD28 receptor. These proteins are also known as co-stimulatory molecules.
Although the verification stage is necessary for the activation of naïve helper T cells, the importance of this stage is best demonstrated during the similar activation mechanism of CD8+ cytotoxic T cells. As naïve CD8+ T cells have no true bias towards foreign sources, these T cells must rely on the activation of CD28 for confirmation that they recognise a foreign antigen (as CD80/CD86 is only expressed by active APC's). CD28 plays an important role in decreasing the risk of T cell auto-immunity against host antigens.
Once the naïve T cell has both pathways activated, the biochemical changes induced by Signal 1 are altered, allowing the cell to activate instead of anergise. The second signal is then obsolete; only the first signal is necessary for future activation. This is also true for memory T cells, which is one example of learned immunity. Faster responses occur upon reinfection because memory T cells have already undergone confirmation and can produce effector cells much sooner.
Proliferation
Once both stimulatory signals are active within the helper T cell, the cell then allows itself to proliferate. It achieves this by releasing a potent T cell growth factor called interleukin-2 (IL-2). Activated T cells also produce the alpha sub-unit of the IL-2 receptor (CD25 or IL-2R), enabling a fully functional receptor that can bind with IL-2, which in turn activates the T cell's proliferation pathways.
In this case, the released IL-2 binds to same T cell's IL-2 receptors to allow itself to proliferate. The phenomenon of cells releasing cytokines to alter their own behaviour is known as auto-regulation (or autocrine stimulation). It should be noted that this is not the only function of IL-2 release, and that IL-2 can also bind to other T cells in the area (paracrine stimulation).
Maturation
After many cell generations, the Th cell's progenitors differentiate into effector Th cells, memory Th cells, and suppressor Th cells.
- Effector Th cells secrete cytokines, proteins or peptides that stimulate or interact with other leukocytes, including Th cells.
- Memory Th cells retain the antigen affinity of the originally activated T cell, and are used to act as later effector cells during a second immune response (e.g. if there is re-infection of the host at a later stage).
- Suppressor T cells do not promote immune function, but act to decrease it instead. Despite their low numbers during an infection, these cells are believed to play an important role in the self-limitation of the immune system; they have been shown to prevent the development of various auto-immune diseases.
The production of IL-2 by helper T cells is also necessary for the proliferation of activated CD8+ T cells. Without helper T cell interactions, CD8+ T cells do not proliferate and eventually become anergic. This cross-reliance on helper T cells is another way the immune system tries to prevent T cell-mediated auto-immune disease.
Determination of the effector T cell response
Helper T cells are capable of influencing a variety of immune cells, and the T cell response generated (including the extracellular signals such as cytokines) can be essential for a successful outcome from infection. In order to be effective, helper T cells must determine which cytokines will allow the immune system to be most useful or beneficial for the host. Understanding exactly how helper T cells respond to immune challenges is currently of major interest in immunology, because such knowledge may be very useful in the treatment of disease and in increasing the effectiveness of vaccination.
Th1/Th2 Model for helper T cells
Proliferating helper T cells that develop into effector T cells differentiate into two major subtypes of cells known as Th1 and Th2 cells (also known as Type 1 and Type 2 helper T cells, respectively).
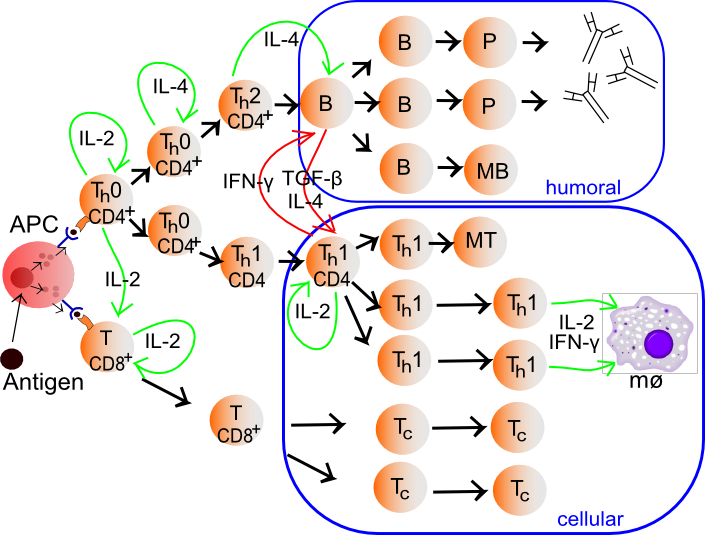
| Type 1/ Th1 | Type 2/ Th2 | |
| Cytokines produced | interferon-gamma and tumor necrosis factor-beta. (Interleukin-2 was classically associated with Th1 cells, but this association may be misleading; IL-2 is produced by all helper T cells early in their activation.) | interleukin-4, interleukin-5, interleukin-6, interleukin-10, interleukin-13 |
| Immune stimulation promoted | Cellular immune system. Maximises the killing efficacy of the macrophages and in the proliferation of cytotoxic CD8+ T cells. | Humoral immune system. Stimulates B-cells into proliferation, to induce B-cell antibody class switching, and to increase antibody production. |
| Other functions | The Type 1 cytokine interferon-gamma increases the production of interleukin-12 by dendritic cells and macrophages, and via positive feedback, IL-12 stimulates the production of IFN-gamma in helper T cells, thereby promoting the Th1 profile. IFN-gamma also inhibits the production of cytokines such as interleukin-4, an important cytokine associated the Type 2 response, and thus it also acts to preserve its own response. | The Type 2 response promotes its own profile using two different cytokines. Interleukin-4 acts on helper T cells to promote the production of Th2 cytokines (including itself; it is auto-regulatory), while interleukin-10 (IL-10) inhibits a variety of cytokines including interleukin-2 and interferon-gamma in helper T cells and IL-12 in dendritic cells and macrophages. The combined action of these two cytokines suggests that once the T cell has decided to produce these cytokines, that decision is preserved (and also encourages other T cells to do the same). |
While we know about the types of cytokine patterns helper T cells tend to produce, we understand less about how the patterns themselves are decided. Various evidence suggests that the type of APC presenting the antigen to the T cell has a major influence on its profile. Other evidence suggests that the concentration of antigen presented to the T cell during primary activation influences its choice. The presence of some cytokines (such as the ones mentioned above) will also influence the response that will eventually be generated, but our understanding is nowhere near complete.
Limitations to the Th1/Th2 model
The interactions between cytokines from the Th1/Th2 model can be more complicated in some animals. For example, the Th2 cytokine IL-10 inhibits cytokine production of both Th subsets in humans. Human IL-10 (hIL-10) suppresses the proliferation and cytokine production of all T cells and the activity of macrophages, but continues to stimulate plasma cells, ensuring that antibody production still occurs. As such, hIL-10 is not believed to truly promote the Th2 response in humans, but acts to prevent over-stimulation of helper T cells while still maximising the production of antibodies.
There are also other types of T cells that can influence the expression and activation of helper T cells, such as natural regulatory T cells, along with less common cytokine profiles such as the Th3 subset of helper T cells. Terms such as "regulatory" and "suppression" have become ambiguous after the discovery that helper CD4+ T cells are also capable of regulating (and suppressing) their own responses outside of dedicated suppressor T cells.
One major difference with "suppressor" (or "natural regulatory") T cells is that they always suppress the immune system, while effector T cell groups usually begin with immune-promoting cytokines and then switch to inhibitory cytokines later in their repertoire. The latter is a feature of Th3 cells, which transform into a suppressor subset after its initial activation and cytokine production.
Both regulatory T cells and Th3 cells produce the cytokine transforming growth factor-beta (TGF-β) and IL-10. Both cytokines are inhibitory to helper T cells; TGF-β suppresses the activity of most of the immune system. There is evidence to suggest that TGF-β may not suppress activated Th2 cells as effectively as it might suppress naive cells, but it is not typically considered a Th2 cytokine.
The characterisation of another novel T helper subtype, T helper 17 cells (Th17)[2] has cast further doubt on the basic Th1/Th2 model. These IL-17 producing cells were initially described as a pathogenic population implicated in autoimmunity but are now thought to have their own distinct effector and regulatory functions.
Many of the cytokines in this article are also expressed by other immune cells (see individual cytokines for details), and it is becoming clear that while the original Th1/Th2 model is enlightening and gives insight into the functions of helper T cells, it is far too simple to define its entire role or actions. Some immunologists question the model completely, as some in vivo studies suggest that individual helper T cells usually do not match the specific cytokine profiles of the Th model, and many cells express cytokines from both profiles. That said, the Th model has still played an important part in developing our understanding of the roles and behaviour of helper T cells and the cytokines they produce during an immune response.
Role of helper T cells in disease
Considering the diverse and important role helper T cells play in the immune system, it is not surprising that these cells often influence the immune response against disease. They also appear to make occasional mistakes, or generate responses that would be politely considered non-beneficial. In the worst case scenario, the helper T cell response could lead to a disaster and the fatality of the host. Fortunately this is a very rare occurrence.
Helper T cells and hypersensitivity
The immune system must achieve a balance of sensitivity in order to respond to foreign antigens without responding to the antigens of the host itself. When the immune system responds to very low levels of antigen that it usually shouldn't respond to, a hypersensitivity response occurs. Hypersensitivity is believed to be the cause of allergy and some auto-immune disease.
Hypersensitivity reactions can be divided into four types:
- Type 1 hypersensitivity includes common immune disorders such as asthma, allergic rhinitis (hay fever), eczema, urticaria (hives) and anaphylaxis. These reactions all involve IgE antibodies, which require a Th2 response during helper T cell development. Preventative treatments, such as corticosteroids and montelukast, focus on suppressing mast cells or other allergic cells; T cells do not play a primary role during the actual inflammatory response. It's important to note that the numeral allocation of hypersensitivity "types" does not correlate (and is completely unrelated) to the "response" in the Th model.
- Type 2 and Type 3 hypersensitivity both involve complications from auto-immune or low affinity antibodies. In both of these reactions, T cells may play an accomplice role in generating these auto-specific antibodies, although some of these reactions under Type 2 hypersensitivity would be considered normal in a healthy immune system (for example, Rhesus factor reactions during child-birth is a normal immune response against child antigens). The understanding of the role of helper T cells in these responses is limited but it is generally thought that Th2 cytokines would promote such disorders. For example, studies have suggested that lupus (SLE) and other auto-immune diseases of similar nature can be linked to the production of Th2 cytokines.
- Type 4 hypersensitivity, also known as delayed type hypersensitivity, are caused via the over-stimulation of immune cells, commonly lymphocytes and macrophages, resulting in chronic inflammation and cytokine release. Antibodies do not play a direct role in this allergy type. T cells play an important role in this hypersensitivity, as they activate against the stimulus itself and promote the activation of other cells; particularly macrophages via Th1 cytokines.
Other cellular hypersensitivities include cytotoxic T cell mediated auto-immune disease, and a similar phenomenon; transplant rejection. Helper T cells are required to fuel the development of these diseases. In order to create sufficient auto-reactive killer T cells, interleukin-2 must be produced, and this is supplied by CD4+ T cells. CD4+ T cells can also stimulate cells such as natural killer cells and macrophages via cytokines such as interferon-gamma, encouraging these cytotoxic cells to kill host cells in certain circumstances.
The mechanism that killer T cells use during auto-immunity is almost identical to their response against viruses, and some viruses have been accused of causing auto-immune diseases such as Type 1 Diabetes mellitus. Cellular auto-immune disease occurs because the host antigen recognition systems fail, and the immune system believes, by mistake, that a host antigen is foreign. As a result, the CD8+ T cells treat the host cell presenting that antigen as infected, and go on to destroy all host cells (or in the case of transplant rejection, transplant organ) that express that antigen.
It should be noted that some of this section is a simplification, and that many auto-immune diseases are more complex; a well known example is rheumatoid arthritis, where both antibodies and immune cells are known to play a role in the pathology. Generally the immunology of most auto-immune diseases is not well understood.
HIV infection
Perhaps the best example of the importance of CD4+ T cells is demonstrated with human immunodeficiency virus (HIV) infection. HIV targets cells that express CD4, and can infect macrophages, dendritic cells (both groups express CD4 at low levels) and CD4+ T cells.
It has been proposed that during the non-symptomatic phase of HIV infection, the virus has a relatively low affinity towards T cells (and has a higher affinity for macrophages), resulting in a slow kill rate of CD4+ T cells by the immune system. This is initially compensated for via the production of new helper T cells from the thymus (originally from the bone marrow). Once the virus becomes lymphotropic (or T-tropic) however, it begins to infect CD4+ T cells far more efficiently (likely due to a change in the co-receptors it binds to during infection), and the immune system is overwhelmed.
At this point, functional CD4+ T cell levels begin to decrease, eventually to a point where the CD4+ T cell population is too small to recognize the full range of antigens that could potentially be detected. The lack of full antigen cover results in the core symptoms of acquired immune deficiency syndrome (AIDS). CD4 T cell depletion during AIDS allows various pathogens to escape T cell recognition, thus allowing opportunistic infections that would normally elicit a helper T cell response to bypass the immune system. While these complete bypass situations only occur when the helper T cell response is absolutely necessary for infection clearance, most infections increase in severity and/or duration because the immune system's helper T cells provide a weaker contribution to a less efficient immune response.
Two components of the immune system are particularly affected in AIDS, due to its CD4+ T cell dependency:
- CD8+ T cells are not stimulated as effectively during the AIDS period of HIV infection, making AIDS patients very susceptible to most viruses, including HIV itself. This decline in killing of CD4+ T cells results in the virus being produced for a longer period (the infected CD4+ T cells are not killed as quickly), increasing the proliferation of the virus, and accelerating the development of the disease.
- Antibody class switching declines significantly once helper T cell function fails. The immune system loses its ability to improve the affinity of their antibodies, and are unable to generate B cells that can produce antibody groups such as IgG and IgA. These effects are primarily due to the loss of any helper T cell that can interact with the B lymphocyte correctly. Another symptom of AIDS is the reduction in antibody levels due to a decrease in Th2 cytokines (and less interactions by helper T cells). All of these complications result in an increased susceptibility to aggressive bacterial infections, especially in areas of the body not accessible by IgM antibodies.
If the patient does not respond to (or does not receive) HIV treatment they will succumb usually to either cancers or infections; the immune system finally reaches a point where it is no longer coordinated or stimulated enough to deal with the disease.
References
- ↑ Rang, H. P. (2003). Pharmacology. Edinburgh: Churchill Livingstone. ISBN 0-443-07145-4. Page 223
- ↑ Template:Harvard reference
dv:ހެލްޕަރ ޓީ ސެލް id:Sel T pembantu nl:T-helpercel sv:T-hjälparcell