Radiation therapy
|
WikiDoc Resources for Radiation therapy |
|
Articles |
|---|
|
Most recent articles on Radiation therapy Most cited articles on Radiation therapy |
|
Media |
|
Powerpoint slides on Radiation therapy |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Radiation therapy |
|
Clinical Trials |
|
Ongoing Trials on Radiation therapy at Clinical Trials.gov Trial results on Radiation therapy Clinical Trials on Radiation therapy at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Radiation therapy NICE Guidance on Radiation therapy
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Radiation therapy Discussion groups on Radiation therapy Patient Handouts on Radiation therapy Directions to Hospitals Treating Radiation therapy Risk calculators and risk factors for Radiation therapy
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Radiation therapy |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]; Assistant Editor-In-Chief: Anand Patel, MD [4]
Overview
Radiation therapy (or radiotherapy) is the medical use of ionizing radiation as part of cancer treatment to control malignant cells (not to be confused with radiology, the use of radiation in medical imaging and diagnosis). Radiotherapy may be used for curative or adjuvant cancer treatment. It is used as palliative treatment (where cure is not possible and the aim is for local disease control or symptomatic relief) or as therapeutic treatment (where the therapy has survival benefit but is not curative) Total body irradiation (TBI) is a radiotherapy technique used to prepare the body to receive a bone marrow transplant. Radiotherapy has a few applications in non-malignant conditions, such as the treatment of trigeminal neuralgia, severe thyroid eye disease, pterygium, prevention of keloid scar growth, and prevention of heterotopic ossification. The use of radiotherapy in non-malignant conditions is limited partly by worries about the risk of radiation-induced cancers.
Radiotherapy is commonly used for the treatment of malignant tumors (cancer), and may be used as the primary therapy. It is also common to combine radiotherapy with surgery, chemotherapy, hormone therapy or some mixture of the three. Most common cancer types can be treated with radiotherapy in some way. The precise treatment intent (curative, adjuvant, neoadjuvant, therapeutic, or palliative) will depend on the tumour type, location, and stage, as well as the general health of the patient.
Radiation therapy is commonly applied to the tumour. The radiation fields may also include the draining lymph nodes if they are clinically or radiologically involved with tumour, or if there is thought to be a risk of subclinical malignant spread. It is necessary to include a margin of normal tissue around the tumour to allow for uncertainties in daily set-up and internal tumor motion. These uncertainties can be caused by internal movement (for example, respiration and bladder filling) and movement of external skin marks relative to the tumour position.
To spare normal tissues (such as skin or organs which radiation must pass through in order to treat the tumour), shaped radiation beams are aimed from several angles of exposure to intersect at the tumour, providing a much larger absorbed dose there than in the surrounding, healthy tissue.
Side effects
Radiation Therapy is in itself painless. Many low-dose palliative treatments (for example, radiotherapy to bony metastases) cause minimal or no side effects. Treatment to higher doses causes varying side effects during treatment (acute side effects), in the months or years following treatment (long-term side effects), or after re-treatment (cumulative side effects). The nature, severity, and longevity of side effects depends on the organs that receive the radiation, the treatment itself (type of radiation, dose, fractionation, concurrent chemotherapy), and the patient.
Most side effects are predictable and expected. One of the aims of modern radiotherapy is to reduce side effects to a minimum, and to help the patient to understand and to deal with those side effects which are unavoidable.
Acute side effects
- Damage, possibly severe, to epithelial surfaces (skin, oral, pharyngeal and bowel mucosa, urothelium)
- The rates of onset and of recovery depend on the rate of turnover of the epithelial cells. Typically the skin starts to become pink and sore several weeks into treatment. The reaction may become more severe during the treatment and for up to about one week following the end of radiotherapy, and the skin may break down. Although this moist desquamation is uncomfortable, recovery is usually quick. Skin reactions tend to be worse in areas where there are natural folds in the skin, such as underneath the female breast, behind the ear, and in the groin.
- Similarly, the lining of the mouth, throat, esophagus, and bowel may be damaged by radiation. If the head and neck area is treated, temporary soreness and ulceration commonly occur in the mouth and throat. If severe, this can affect swallowing, and the patient may need painkillers and nutritional support. The esophagus can also become sore if it is treated directly, or if, as commonly occurs, it receives a dose of collateral radiation during treatment of lung cancer.
- The lower bowel may be treated directly with radiation (treatment of rectal or anal cancer) or be exposed by radiotherapy to other pelvic structures (prostate, bladder, female genital tract). Typical symptoms are soreness, diarrhoea, and nausea.
- Swelling (edema or Oedema)
- As part of the general inflammation that occurs, swelling of soft tissues may cause problems during radiotherapy. This is a concern during treatment of brain tumours and brain metastases, especially where there is pre-existing raised intracranial pressure or where the tumour is causing near-total obstruction of a lumen (e.g., trachea or main bronchus). Surgical intervention may be considered prior to treatment with radiation. If surgery is deemed unnecessary or inappropriate, the patient may receive steroids during radiotherapy to reduce swelling.
- Infertility
- The gonads (ovaries and testicles) are very sensitive to radiation. They may be unable to produce gametes following direct exposure to most normal treatment doses of radiation. Treatment planning for all body sites is designed to minimize, if not completely exclude dose to the gonads if they are not the primary area of treatment.
- Generalized fatigue
Medium and long-term side effects
These depend on the tissue that received the treatment; they may be minimal.
- Fibrosis
- Tissues which have been irradiated tend to become less elastic over time due to a diffuse scarring process.
- Hair loss
- This may be most pronounced in patients who have received radiotherapy to the brain. Unlike the hair loss seen with chemotherapy, radiation-induced hair loss is more likely to be permanent, but is also more likely to be limited to the area treated by the radiation.
- Dryness
- The salivary glands and tear glands have a radiation tolerance of about 30 Gy in 2 Gy fractions, a dose which is exceeded by most radical head and neck cancer treatments. Dry mouth (xerostomia) and dry eyes (xerophthalmia) can become irritating long-term problems and severely reduce the patient's quality of life. Similarly, sweat glands in treated skin (such as the armpit) tend to stop working, and the naturally moist vaginal mucosa is often dry following pelvic irradiation.
- Cancer
- Radiation is a potential cause of cancer, and secondary malignancies are seen in a very small minority of patients, generally many years after they have received a course of radiation treatment. In the vast majority of cases, this risk is greatly outweighed by the reduction in risk conferred by treating the primary cancer.
Cumulative side effects
Cumulative effects from reirradiation should not be confused with long-term effects—when short-term effects have disappeared and long-term effects are subclinical, reirradiation can still be problematic [1].
Dose
The amount of radiation used in radiation therapy is measured in gray (Gy), and varies depending on the type and stage of cancer being treated. For curative (radical) cases, the typical dose for a solid epithelial tumor ranges from 60 to 80 Gy, while lymphoma tumors are treated with 20 to 40 Gy. Preventative (adjuvant) doses are typically around 45 - 60 Gy in 1.8 - 2 Gy fractions (for Breast, Head and Neck cancers respectively.) Many other factors are considered by radiation oncologists when selecting a dose, including whether the patient is receiving chemotherapy, whether radiation therapy is being administered before or after surgery, and the degree of success of surgery.
Fractionation
The total dose is fractionated (spread out over time) in order to give normal cells time to recover. In the USA and Europe, the typical fractionation schedule for adults is 1.8 to 2 Gy per day, five days a week. In the northern United Kingdom, fractions are more commonly 2.67 to 2.75 Gy per day, which eases the burden on thinly spread resources in the National Health Service. For children, a typical fraction is 1.5 to 1.7 Gy per day, reducing the chance and severity of late-onset side effects.
In some cases, two fractions per day are used near the end of a course of treatment. This schedule, known as a concomitant boost regimen and/or hyperfractionation, is used on tumors that regenerate more quickly when they are smaller. In particular, tumors in the head and neck demonstrate this behavior.
One of the best-known alternative fractionation schedules is Continuous Hyperfractionated Accelerated Radiotherapy (CHART). CHART, used to treat lung cancer, consists of three smaller fractions per day. Although reasonably successful, CHART can be a strain on radiation therapy departments.
Implants can be fractionated over minutes or hours, or they can be permanent seeds which slowly deliver radiation until they become inactive.
Mechanism of action
Radiation therapy works by damaging the DNA of cells. The damage is caused by a photon, electron, proton, neutron, or ion beam directly or indirectly ionizing the atoms which make up the DNA chain. Indirect ionization happens as a result of the ionization of water, forming free radicals, notably hydroxyl radicals, which then damage the DNA. In the most common forms of radiation therapy, most of the radiation effect is through free radicals. Because cells have mechanisms for repairing DNA damage, breaking the DNA on both strands proves to be the most significant technique in modifying cell characteristics. Because cancer cells generally are undifferentiated and stem cell-like, they reproduce more, and have a diminished ability to repair sub-lethal damage compared to most healthy differentiated cells. The DNA damage is inherited through cell division, accumulating damage to the cancer cells, causing them to die or reproduce more slowly. Proton radiotherapy works by sending protons with varying kinetic energy to precisely stop at the tumor.
One of the major limitations of radiotherapy is that the cells of solid tumors become deficient in oxygen. This is because solid tumours usually outgrow their blood supply, causing a low-oxygen state known as hypoxia. The more hypoxic the tumours are the more resistant they are to the effects of radiation because oxygen makes the radiation damage to DNA permanent. Much research has been devoted to overcoming this problem including the use of high pressure oxygen tanks, blood substitutes that carry increased oxygen, hypoxic cell radiosensitizers such as misonidazole and metronidazole, and hypoxic cytotoxins, such as tirapazamine. There is also interest in the fact that high LET particles such as carbon or neon ions may have an antitumour effect which is independent of tumour hypoxia.
History of radiation therapy
Radiation therapy has been in use as a cancer treatment for more than 100 years, with its earliest roots traced from the discovery of x-rays in 1895.[2] The concept of therapeutic radiation was invented by German physicist Wilhelm Conrad Rontgen when he discovered that the x-ray was a powerful and effective tool with which to treat cancer.
The field of radiation therapy began to grow in the early 1900s largely due to the groundbreaking work of Nobel Prize-winning scientist Marie Curie, who discovered the radioactive elements polonium and radium. This began a new era in medical treatment and research.[2]. Radium was used in various forms until the mid-1900s when cobalt and caesium units came into use. Medical linear accelerators have been developed since the late 1940s.
With Godfrey Hounsfield’s discovery of computed tomography (CT), three-dimensional planning became a possibility and created a shift from 2-D to 3-D radiation delivery; physicians and physics were no longer limited because CT-based planning allowed physicians to directly measure the dose delivered to the patient's anatomy based on axial tomographical images. Orthovoltage and cobalt units have largely been replaced by megavoltage linear accelerators, useful for their penetrating energies and lack of physical radiation source.
In the last few decades, the advent of new imaging technologies, e.g., magnetic resonance imaging (MRI) in the 1970s and positron emission tomography (PET) in the 1980s, as well as new radiation delivery and visualization products, e.g., digital linear accelerator, image fusion has moved radiation therapy from 3-D conformal to IMRT and eventually to IGRT (4-D) in the near future. These advances have resulted in better treatment outcomes and less side effects. Now 70% of cancer patients receive radiation therapy as part of their cancer treatment.
Types of radiation therapy
Three main divisions of radiotherapy are external beam radiotherapy (EBRT or XBRT) or teletherapy, brachytherapy or sealed source radiotherapy and unsealed source radiotherapy. The differences relate to the position of the radiation source; external is outside the body, while sealed and unsealed source radiotherapy has radioactive material delivered internally. Brachytherapy sealed sources are usually extracted later, while unsealed sources may be administered by injection or ingestion. Proton therapy is a special case of external beam radiotherapy where the particles are protons.
Roughly half of the 2500 worldwide radiotherapy clinics are in the US (as of 2001).
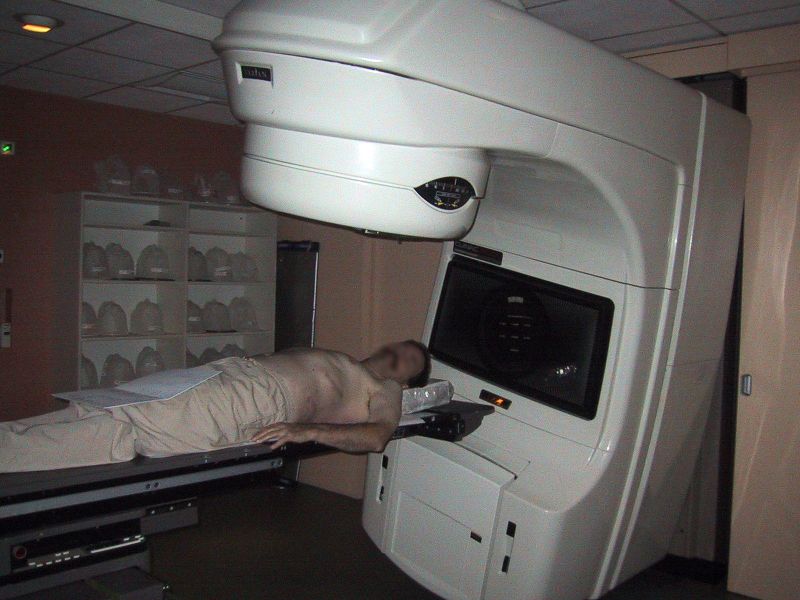
Conventional external beam radiotherapy
Conventional external beam radiotherapy (2DXRT) is delivered via two-dimensional beams using linear accelerator machines. 2DXRT mainly consists of a single beam of radiation delivered to the patient from several directions: often front or back, and both sides. Conventional refers to the way the treatment is planned or simulated on a specially calibrated diagnostic x-ray machine known as a simulator because it recreates the linear accelerator actions (or sometimes by eye), and to the usually well established arrangements of the radiation beams to achieve a desired plan. The aim of simulation is to accurately target or localize the volume which is to be treated. This technique is well established and is generally quick and reliable. The worry is that some high-dose treatments may be limited by the radiation toxicity capacity of healthy tissues which lay close to the target tumor volume. An example of this problem is seen in radiation of the prostate gland, where the sensitivity of the adjacent rectum limits the dose which can be safely prescribed to such an extent that tumor control may not be easily achievable. Previous to the invention of the CT, physicians and physicists had limited knowledge about the true radiation dosage delivered to both cancerous and healthy tissue. For this reason, 3-dimensional conformal radiotherapy is becoming the standard treatment for a number of tumor sites.
Virtual simulation, 3-dimensional conformal radiotherapy, and intensity-modulated radiotherapy
The planning of radiotherapy treatment has been revolutionized by the ability to delineate tumors and adjacent normal structures in three dimensions using specialized CT and/or MRI scanners and planning software.[3] Virtual simulation, the most basic form of planning, allows more accurate placement of radiation beams than is possible using conventional X-rays, where soft-tissue structures are often difficult to assess and normal tissues difficult to protect.
An enhancement of virtual simulation is 3-Dimensional Conformal Radiotherapy (3DCRT), in which the profile of each radiation beam is shaped to fit the profile of the target from a beam's eye view (BEV) using a multileaf collimator (MLC) and a variable number of beams. When the treatment volume conforms to the shape of the tumour, the relative toxicity of radiation to the surrounding normal tissues is reduced, allowing a higher dose of radiation to be delivered to the tumor than conventional techniques would allow.
Intensity-Modulated Radiation Therapy (IMRT) is an advanced type of high-precision radiation that is the next generation of 3DCRT.(Galvin et al 2004) Computer-controlled x-ray accelerators distribute precise radiation doses to malignant tumors or specific areas within the tumor. The pattern of radiation delivery is determined using highly-tailored computing applications to perform optimization and treatment simulation (Treatment Planning). The radiation dose is consistent with the 3-D shape of the tumor by controlling, or modulating, the radiation beam’s intensity. IMRT also improves the ability to conform the treatment volume to concave tumor shapes, for example when the tumor is wrapped around a vulnerable structure such as the spinal cord or a major organ or blood vessel. The radiation dose intensity is elevated near the gross tumor volume while radiation among the neighboring normal tissue is decreased or avoided completely. The customized radiation dose is intended to maximize tumor dose while simultaneously protecting the surrounding normal tissue. Because of this, IMRT allows for higher radiation doses to be delivered to the tumor while sparing healthy tissue as compared with conventional radiation therapy techniques (2DXRT and 3DCRT). This in turn results in better tumor targeting, lessened side effects, and improved treatment outcomes than even 3DCRT.
3DCRT is still used extensively for many body sites but the use of IMRT is growing in more complicated body sites such as CNS, head and neck, prostate, breast and lung. Unfortunately, IMRT is limited by its need for additional time from experienced medical personnel. This is because physicians must manually delineate the tumors one CT image at a time through the entire disease site which can take much longer than 3DCRT preparation. Then, medical physicists and dosimetrists must be engaged to create a viable treatment plan. Also, the IMRT technology has only been used commercially since the late 1990s even at the most advanced cancer centers, so radiation oncologists who did not learn it as part of their residency program must to find additional sources of education before implementing IMRT.
Proof of improved survival benefit from either of these two techniques over conventional radiotherapy (2DXRT) is growing for many tumor sites, but the ability to reduce toxicity is generally accepted. Both techniques enable dose escalation, potentially increasing usefulness. There has been some concern, particularly with 3DCRT, about increased exposure of normal tissue to radiation and the consequent potential for secondary malignancy. Overconfidence in the accuracy of imaging may increase the chance of missing lesions that are invisible on the planning scans (and therefore not included in the treatment plan) or that move between or during a treatment (for example, due to respiration or inadequate patient immobilization). New techniques are being developed to better control this uncertainty—for example, real-time imaging combined with real-time adjustment of the therapeutic beams. This new technology is called image-guided radiation therapy (IGRT) or four-dimensional radiotherapy.
Radioisotope Therapy (RIT)
Radiotherapy can also be delivered through infusion (into the bloodstream) or ingestion. Examples are the infusion of metaiodobenzylguanidine (MIBG) to treat neuroblastoma, of oral iodine-131 to treat thyroid cancer or thyrotoxicosis, and of hormone-bound lutetium-177 and yttrium-90 to treat neuroendocrine tumors (peptide receptor radionuclide therapy). Another example is the injection of radioactive glass or resin microspheres into the hepatic artery to radioembolize liver tumors or liver metastases.
In 2002, the United States Food and Drug Administration (FDA) approved Ibritumomab tiuxetan (Zevalin), which is a monoclonal antibody anti-CD20 conjugated to a molecule of Yttrium-90. [4] In 2003, the FDA approved Tositumomab Iodine-131 (Bexxar), which conjugates a molecule of Iodine-131 to the monoclonal antibody anti-CD20. [5] These medications were the first agents of what is known as radioimmunotherapy, and they were approved for the treatment of refractory non-Hodgkins lymphoma.Uranium-235 is also used in radiotherapy recently to treat some diseases.
References
- Galvin, JM; Ezzel, G; Eisbrauch, A; Yu, C; Butler, B; Xiao, Y; Rosen, I; Rosenman, J; Sharpe, M; Xing, L; Xia, P; Lomax, T; Low, DA; Palta, J contribution = (2004), "Implementing IMRT in clinical practice: a joint document of the American Society for Therapeutic Radiology and Oncology and the American Association of Physicists in Medicine.", Int J Radiat Oncol Biol Phys., 58 (5), p. 1616-34 Unknown parameter
|month=ignored (help)
General references
- Practical Radiotherapy Planning, Dobbs J, Barrett A, Ash D (1999) Arnold ISBN 0-340-70631-7
- ↑ Nieder C, Milas L, Ang KK (2000). "Tissue tolerance to reirradiation". Semin Radiat Oncol. 10 (3): 200–9. PMID 11034631.
- ↑ 2.0 2.1 "University of Alabama at Birmingham Comprehensive Cancer Center, History of Radiation Oncology".
- ↑ Bucci M, Bevan A, Roach M (2005). "Advances in radiation therapy: conventional to 3D, to IMRT, to 4D, and beyond". CA Cancer J Clin. 55 (2): 117–34. PMID 15761080.Full text
- ↑ [1]
- ↑ [2]
ar:علاج إشعاعي cs:Radioterapie da:Strålebehandling de:Strahlentherapie eu:Erradioterapia fa:پرتودرمانی ko:방사선종양학과 is:Geislalækningar it:Radioterapia he:רדיותרפיה nl:Radiotherapie no:Strålebehandling nn:Radioterapi sl:Radioterapija wa:Radioterapeye fi:Sädehoito sv:Strålbehandling wa:Radioterapeye