Pterygium
Template:DiseaseDisorder infobox
|
WikiDoc Resources for Pterygium |
|
Articles |
|---|
|
Most recent articles on Pterygium |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Pterygium at Clinical Trials.gov Clinical Trials on Pterygium at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Pterygium
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Pterygium Discussion groups on Pterygium Directions to Hospitals Treating Pterygium Risk calculators and risk factors for Pterygium
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Pterygium |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Roukoz A. Karam, M.D.[2]
Synonyms and keywords: pterygia
Overview
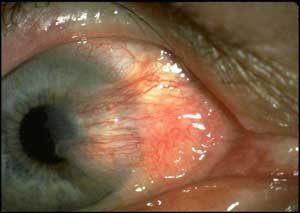
Pterygium usually refers to a benign growth of the conjunctiva. Alternately, it refers to any winglike triangular membrane occurring in the neck, eyelids, knees, elbows, ankles or digits. An example is popliteal pterygium syndrome, which affects the legs. The term comes from the Greek word pterygion meaning "wing". When associated with the conjunctiva, a pterygium commonly grows from the nasal side of the sclera. It is associated with, and thought to be caused by ultraviolet-light exposure (e.g. sunlight), low humidity, and dust. The predominance of pterygia on the nasal side is possibly a result of the sun's rays passing laterally through the cornea where it undergoes refraction and becomes focused on the limbic area. Sunlight passes unobstructed from the lateral side of the eye, focusing on the medial limbus after passing through the cornea. On the contralateral side, however, the shadow of the nose medially reduces the intensity of sunlight focused on the lateral/temporal limbus.
Historical Perspective
It is not clear when pterygium first became known. However,
Classification
Pterygium can be classified into 3 main groups:[1]
| Grade | Description |
|---|---|
| Mild Pterygium | Clearly visible episcleral blood vessels under the body of the pterygium |
| Moderate Pterygium | Partially visible episcleral blood vessels under the body of the pterygium |
| Severe Pterygium | Totally obscured episcleral blood vessels under the body of the pterygium |
Pathophysiology
- Pterygium in the conjunctiva is characterized by elastic degeneration of collagen and fibrovascular proliferation.
- It has an advancing portion called the head of the pterygium, which is connected to the main body of the pterygium by the neck.
- Sometimes a line of iron deposition can be seen adjacent to the head of the pterygium called Stocker's line.
- The location of the line can give an indication of the pattern of growth.
- As it is a benign growth, it requires no treatment unless it grows to such an extent that it covers the pupil, obstructing vision.
Causes
The exact cause is unknown, but it is associated with excessive exposure to wind, sun, or sand.
Differentiating Pterygium From Other Diseases
- Pinguecula is a degenerative eye condition that is often confused with pterygium.
- A pinguecula is a yellowish, slightly raised conjunctival lesion arising at the limbal conjunctiva.
- Unlike a pterygium that arises from the limbus and progresses onto the cornea, a pinguecula arises from the limbus and remains confined to the conjunctiva without corneal involvement.
- Pseudopterygium
- Neoplasia
- Carcinoma in situ
- Squamous cell carcinoma
- Other neoplastic diseases
Epidemiology and Demographics
Age
Several population-based studies have found higher rates of pterygium to be associated with older age.
It is uncommon for patients to present with pterygium prior to age 20 years. Patients older than 40 years have the highest prevalence of pterygia, while patients aged 20-40 years are reported to have the highest incidence of pterygium.
Gender
Pterygium is reported to occur in males twice as frequently as in females.
Race
Risk Factors
Several risk factors may lead to the formation of pterygium, these include:[2]
- Ultraviolet (UV) light[3]
- UV radiation may trigger events that produce damage to cellular DNA, RNA, and extracellular matrix composition
- Abnormal conjunctival expression of tumor suppressor gene p53
- Angiogenesis-related factors
- Human papillomavirus (HPV) infection
- Abnormal human leukocyte antigen (HLA)expression
- Family history
Screening
There is insufficient evidence to recommend routine screening for pterygium.
Natural History, Complications, and Prognosis
Natural History
- The natural history of pterygium is poorly understood.
- Pterygium, when active, can grow over a period of several months to years.
- Activity is marked clinically by redness and localized thickening, which probably represent active inflammation. When inactive (white and flat), pterygium may remain static for decades with no measurable increase in size or clinical significance. It is unclear how pterygium converts from active to inactive, or if it can be reactivated.
Complications
Complications of pterygium include the following:
- Distortion and/or reduction of central vision
- Redness
- Irritation
- Chronic scarring of the conjunctiva and the cornea
Prognosis
- Recurrence rates for simple surgical excision to bare sclera are high, varying between 30 to 80 percent of cases, and reported as high as 90 percent in certain subpopulations.
- The high recurrence rate, even when adjunctive measures are used with excision, is the main reason that surgery is not recommended for a small pterygium, for irritation, or for cosmetic reasons alone.
- The visual and cosmetic prognosis following pterygium excision is good. The procedures are well tolerated by patients, and, aside from some discomfort in the first few postoperative days, most patients are able to resume full activity within 48 hours of their surgery.[4]
- Those patients who develop recurrent pterygia can be retreated with repeat surgical excision and grafting, with conjunctival/limbal autografts or amniotic membrane transplants in selected patients.[5]
Diagnosis
Diagnostic Study of Choice
- The diagnosis of pterygium is made by the classic clinical appearance of a wedge-shaped growth extending onto the cornea.
- However, pterygium does not always manifest in its classic form, and other conditions may have a similar appearance.
- It is important to distinguish pterygium from these other conditions, particularly neoplastic lesions.
History and Symptoms
- The most common symptoms caused by pterygium are redness and irritation.
- Visual impairment is less common. In the absence of symptoms, patients may also report a change in the appearance of their eye, or pterygium may be noted incidentally on physical examination.
Physical Examination
Laboratory Findings
Electrocardiogram
There are no ECG findings associated with pteryigum.
X-ray
There are no x-ray findings associated with pteryigum.
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with pteryigum.
CT scan
There are no CT scan findings associated with pteryigum.
MRI
There are no MRI findings associated with pteryigum.
Other Imaging Findings
Corneal topography can be very useful in determining the degree of irregular astigmatism induced by an advanced pterygium.
Other Diagnostic Studies
Treatment
Medical Therapy
Medical treatments are for symptomatic relief and have not been shown to stop progression or cause regression of a pterygium.
- Patients with pterygium that do not affect vision or eye movement may be treated symptomatically with topical lubricants including drops, ointments, and gels, all of which are available over-the-counter.[6]
- Artificial tears are the most frequently utilized topical lubricant for pterygium and may help to reduce symptoms.
- They can be given 1 to 2 drops to affected area three to four times daily.
- Preservative-free preparations should be used in patients who have irritative symptoms with preservatives or who need to use lubrication more than four times per day.
- Preservative-free preparations are more expensive.
- Treatment with topical decongestants, NSAIDs, and glucocorticoids may also be effective for symptomatic relief of pterygium.[7][8]
- These are associated with adverse effects which limit their use.
- Topical decongestants can be used to treat redness and irritation not relieved by artificial tears.
Surgery
Definitive treatment is achieved only by surgical removal. Long term follow up is required as pterygium may recur even after complete surgical correction.
Indications for surgical removal of pterygium include:
- Astigmatism leading to visual impairment
- Opacity in the visual axis
- Documented growth that is threatening to affect the visual axis via astigmatism or opacity
- Restriction of eye movement
- Significant cosmetic impact or intractable irritation
Primary Prevention
- Theoretically, minimizing exposure to ultraviolet radiation should reduce the risk of development of pterygium in susceptible individuals.
- Patients are advised to use a hat or a cap with a brim, in addition to ultraviolet-blocking coatings on the lenses of glasses/sunglasses to be used in areas of sun exposure.
Secondary Prevention
See also
External links
- Facts About the Cornea and Corneal Disease The National Eye Institute (NEI)
References
- ↑ Tan DT, Chee SP, Dear KB, Lim AS (1997). "Effect of pterygium morphology on pterygium recurrence in a controlled trial comparing conjunctival autografting with bare sclera excision". Arch Ophthalmol. 115 (10): 1235–40. doi:10.1001/archopht.1997.01100160405001. PMID 9338666.
- ↑ Bradley JC, Yang W, Bradley RH, Reid TW, Schwab IR (2010). "The science of pterygia". Br J Ophthalmol. 94 (7): 815–20. doi:10.1136/bjo.2008.151852. PMID 19515643.
- ↑ Threlfall TJ, English DR (1999). "Sun exposure and pterygium of the eye: a dose-response curve". Am J Ophthalmol. 128 (3): 280–7. doi:10.1016/s0002-9394(99)00161-0. PMID 10511020.
- ↑ Fernandes M, Sangwan VS, Bansal AK, Gangopadhyay N, Sridhar MS, Garg P; et al. (2005). "Outcome of pterygium surgery: analysis over 14 years". Eye (Lond). 19 (11): 1182–90. doi:10.1038/sj.eye.6701728. PMID 15543190.
- ↑ Starck T, Kenyon KR, Serrano F (1991). "Conjunctival autograft for primary and recurrent pterygia: surgical technique and problem management". Cornea. 10 (3): 196–202. PMID 2055023.
- ↑ Hoffman RS, Power WJ (1999). "Current options in pterygium management". Int Ophthalmol Clin. 39 (1): 15–26. PMID 10083903.
- ↑ Frucht-Pery J, Siganos CS, Solomon A, Shvartzenberg T, Richard C, Trinquand C (1999). "Topical indomethacin solution versus dexamethasone solution for treatment of inflamed pterygium and pinguecula: a prospective randomized clinical study". Am J Ophthalmol. 127 (2): 148–52. doi:10.1016/s0002-9394(98)00327-4. PMID 10030555.
- ↑ Frucht-Pery J, Solomon A, Siganos CS, Shvartzenberg T, Richard C, Trinquand C (1997). "Treatment of inflamed pterygium and pinguecula with topical indomethacin 0.1% solution". Cornea. 16 (1): 42–7. PMID 8985633.