Ivosidenib
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Zach Leibowitz [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
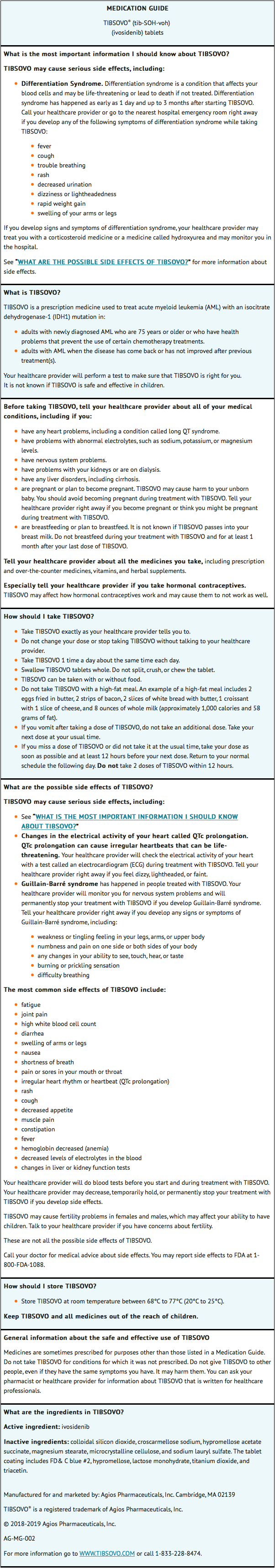
Black Box Warning
|
WARNING: DIFFERENTIATION SYNDROME
See full prescribing information for complete Boxed Warning.
*Patients treated with ivosidenib have experienced symptoms of differentiation syndrome, which can be fatal if not treated. Symptoms may include fever, dyspnea, hypoxia, pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain or peripheral edema, hypotension, and hepatic, renal, or multi-organ dysfunction. If differentiation syndrome is suspected, initiate corticosteroid therapy and hemodynamic monitoring until symptom resolution.
|
Overview
Ivosidenib is an isocitrate dehydrogenase-1 (IDH1) inhibitor that is FDA approved for the treatment of acute myeloid leukemia (AML) with a susceptible IDH1 mutation as detected by an FDA-approved test in adult patients with newly-diagnosed AML who are ≥ 75 years old or who have comorbidities that preclude use of intensive induction chemotherapy and adult patients with relapsed or refractory AML. There is a Black Box Warning for this drug as shown here. Common adverse reactions include fatigue, arthralgia, leukocytosis, diarrhea, edema, nausea, dyspnea, mucositis, electrocardiogram QT prolonged, rash, cough, decreased appetite, myalgia, constipation, and pyrexia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indication
- Ivosidenib is indicated for the treatment of newly-diagnosed acute myeloid leukemia (AML) with a susceptible isocitrate dehydrogenase-1 (IDH1) mutation as detected by an FDA-approved test in adult patients who are ≥ 75 years old or who have comorbidities that preclude use of intensive induction chemotherapy.
- Ivosidenib is indicated for the treatment of adult patients with relapsed or refractory acute myeloid leukemia (AML) with a susceptible isocitrate dehydrogenase-1 (IDH1) mutation as detected by an FDA-approved test.
Dosage
- The recommended dose of ivosidenib is 500 mg taken orally once daily until disease progression or unacceptable toxicity. For patients without disease progression or unacceptable toxicity, treat for a minimum of 6 months to allow time for clinical response.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding ivosidenib Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding ivosidenib Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
The safety and effectiveness of ivosidenib in pediatric patients have not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding ivosidenib Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding ivosidenib Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
None.
Warnings
|
WARNING: DIFFERENTIATION SYNDROME
See full prescribing information for complete Boxed Warning.
*Patients treated with ivosidenib have experienced symptoms of differentiation syndrome, which can be fatal if not treated. Symptoms may include fever, dyspnea, hypoxia, pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain or peripheral edema, hypotension, and hepatic, renal, or multi-organ dysfunction. If differentiation syndrome is suspected, initiate corticosteroid therapy and hemodynamic monitoring until symptom resolution.
|
Differentiation Syndrome
- In the clinical trial, 25% (7/28) of patients with newly diagnosed AML and 19% (34/179) of patients with relapsed or refractory AML treated with ivosidenib experienced differentiation syndrome. Differentiation syndrome is associated with rapid proliferation and differentiation of myeloid cells and may be life-threatening or fatal if not treated. Symptoms of differentiation syndrome in patients treated with ivosidenib included noninfectious leukocytosis, peripheral edema, pyrexia, dyspnea, pleural effusion, hypotension, hypoxia, pulmonary edema, pneumonitis, pericardial effusion, rash, fluid overload, tumor lysis syndrome and creatinine increased. Of the 7 patients with newly diagnosed AML who experienced differentiation syndrome, 6 (86%) patients recovered. Of the 34 patients with relapsed or refractory AML who experienced differentiation syndrome, 27 (79%) patients recovered after treatment or after dose interruption of ivosidenib. Differentiation syndrome occurred as early as 1 day and up to 3 months after ivosidenib initiation and has been observed with or without concomitant leukocytosis.
- If differentiation syndrome is suspected, initiate dexamethasone 10 mg IV every 12 hours (or an equivalent dose of an alternative oral or IV corticosteroid) and hemodynamic monitoring until improvement. If concomitant noninfectious leukocytosis is observed, initiate treatment with hydroxyurea or leukapheresis, as clinically indicated. Taper corticosteroids and hydroxyurea after resolution of symptoms and administer corticosteroids for a minimum of 3 days. Symptoms of differentiation syndrome may recur with premature discontinuation of corticosteroid and/or hydroxyurea treatment. If severe signs and/or symptoms persist for more than 48 hours after initiation of corticosteroids, interrupt ivosidenib until signs and symptoms are no longer severe.
QTc Interval Prolongation
- Patients treated with ivosidenib can develop QT (QTc) prolongation and ventricular arrhythmias. Of the 258 patients with hematological malignancies treated with ivosidenib in the clinical trial, 9% were found to have a QTc interval greater than 500 msec and 14% of patients had an increase from baseline QTc greater than 60 msec. One patient developed ventricular fibrillation attributed to ivosidenib. The clinical trial excluded patients with baseline QTc of ≥ 450 msec (unless the QTc ≥ 450 msec was due to a pre-existing bundle branch block) or with a history of long QT syndrome or uncontrolled or significant cardiovascular disease.
- Concomitant use of ivosidenib with drugs known to prolong the QTc interval (e.g., anti-arrhythmic medicines, fluoroquinolones, triazole anti-fungals, 5-HT3 receptor antagonists) and CYP3A4 inhibitors may increase the risk of QTc interval prolongation. Conduct monitoring of electrocardiograms (ECGs) and electrolytes.
- In patients with congenital long QTc syndrome, congestive heart failure, electrolyte abnormalities, or those who are taking medications known to prolong the QTc interval, more frequent monitoring may be necessary.
- Interrupt ivosidenib if QTc increases to greater than 480 msec and less than 500 msec. Interrupt and reduce ivosidenib if QTc increases to greater than 500 msec. Permanently discontinue ivosidenib in patients who develop QTc interval prolongation with signs or symptoms of life-threatening arrhythmia.
Guillain-Barré Syndrome
- Guillain-Barré syndrome occurred in < 1% (2/258) of patients treated with ivosidenib in the clinical study. Monitor patients taking ivosidenib for onset of new signs or symptoms of motor and/or sensory neuropathy such as unilateral or bilateral weakness, sensory alterations, paresthesias, or difficulty breathing. Permanently discontinue ivosidenib in patients who are diagnosed with Guillain-Barré syndrome.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The safety of ivosidenib as a single agent at 500 mg daily was evaluated in 213 patients with AML in Study AG120-C-001. The median age of ivosidenib treated patients was 68 (range 18-87) with 68% ≥ 65 years, 51% male, 66% White, 6% Black or African American, 3% Asian, 0.5% Native Hawaiian or other Pacific Islander, 0.5% American Indian or Alaska Native, and 24% other/not provided. Among the 213 patients who received ivosidenib, 37% were exposed for 6 months or longer and 14% were exposed for 12 months or longer. The most common adverse reactions including laboratory abnormalities in ≥ 20% of 213 patients who received ivosidenib were hemoglobin decreased, fatigue, arthralgia, calcium decreased, sodium decreased, leukocytosis, diarrhea, magnesium decreased, edema, nausea, dyspnea, uric acid increased, potassium decreased, alkaline phosphatase increased, mucositis, aspartate aminotransferase increased, phosphatase decreased, electrocardiogram QT prolonged, rash, creatinine increased, cough, decreased appetite, myalgia, constipation, and pyrexia.
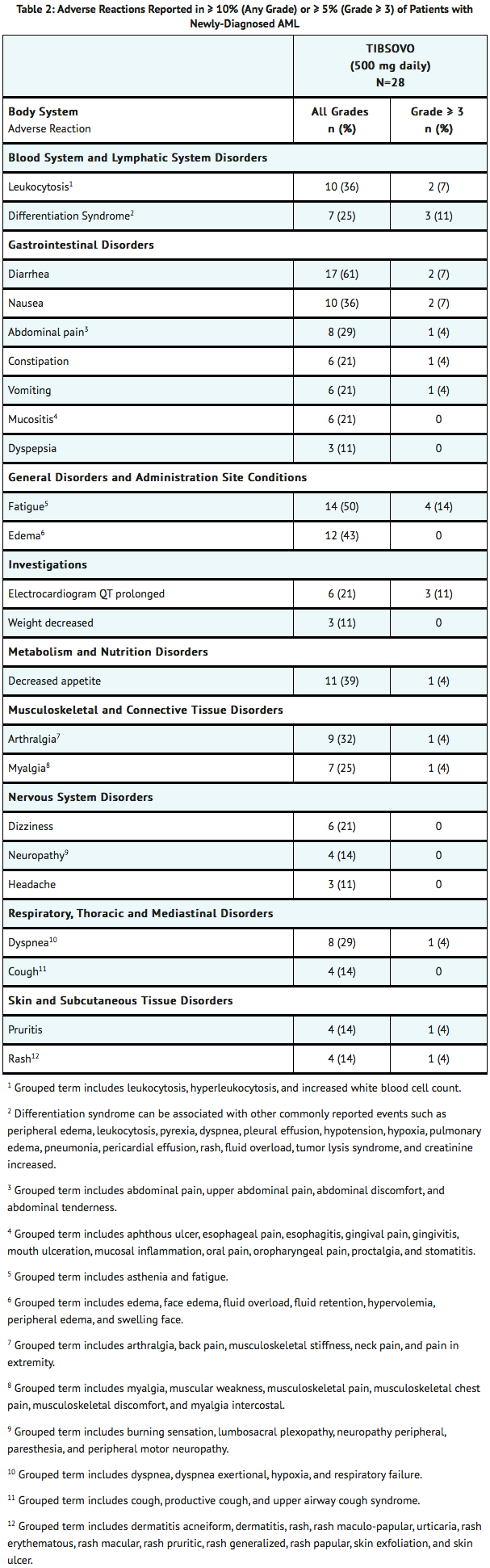
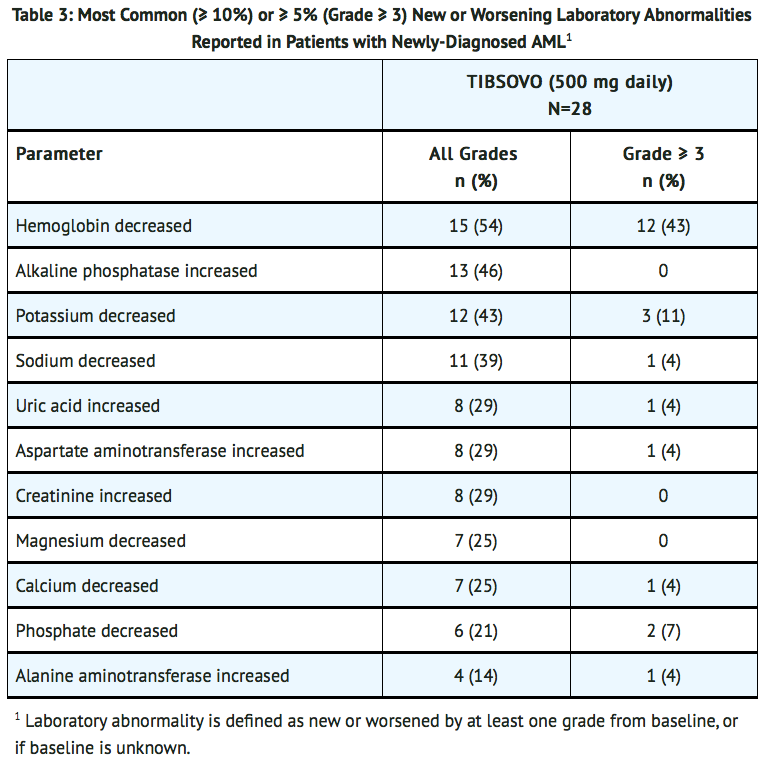
Newly-Diagnosed AML
- The safety profile of single-agent ivosidenib was studied in 28 adults with newly-diagnosed AML treated with 500 mg daily. The median duration of exposure to ivosidenib was 4.3 months (range 0.3 to 40.9 months). Ten patients (36%) were exposed to ivosidenib for at least 6 months and 6 patients (21%) were exposed for at least 1 year.
- Common (≥ 5%) serious adverse reactions included differentiation syndrome (18%), electrocardiogram QT prolonged (7%), and fatigue (7%). There was one case of posterior reversible encephalopathy syndrome (PRES).
- Common (≥ 10%) adverse reactions leading to dose interruption included electrocardiogram QT prolonged (14%) and differentiation syndrome (11%). Two (7%) patients required a dose reduction due to electrocardiogram QT prolonged. One patient each required permanent discontinuation due to diarrhea and PRES.
- The most common adverse reactions reported in the trial are shown in TABLE 2.
- Changes in selected post-baseline laboratory values that were observed in patients with newly diagnosed AML are shown in TABLE 3.
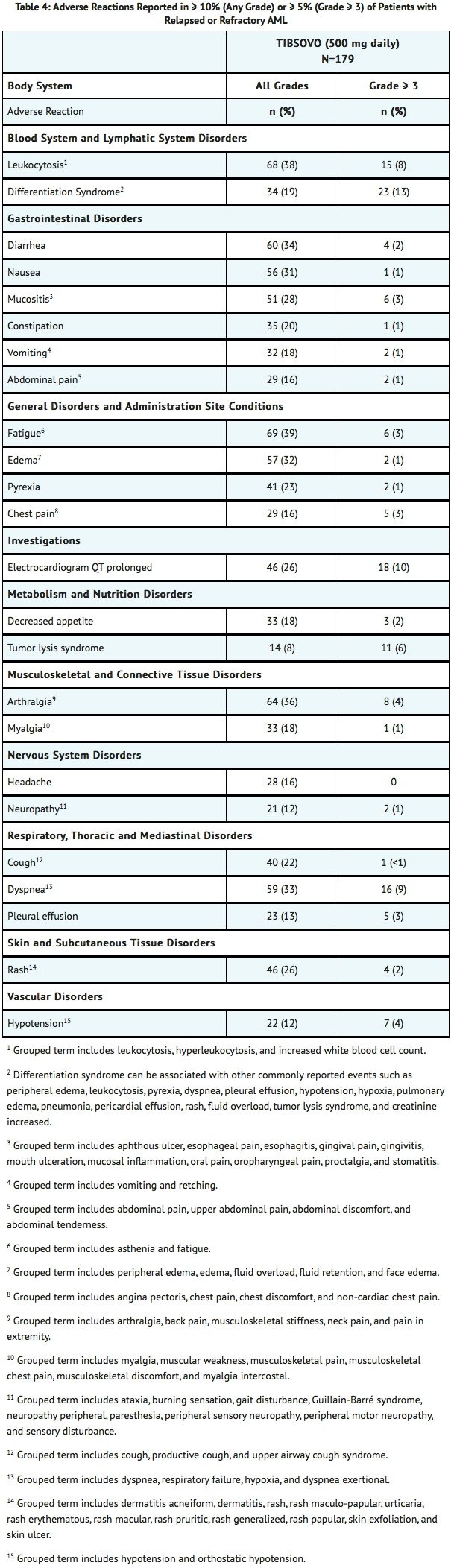
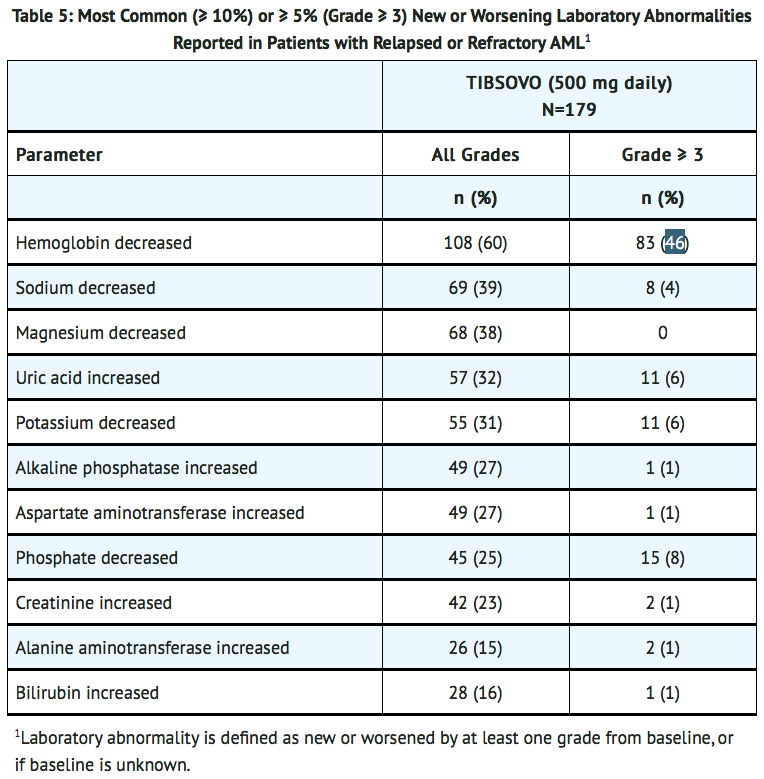
Relapsed or Refractory AML
- The safety profile of single-agent ivosidenib was studied in 179 adults with relapsed or refractory AML treated with 500 mg daily.
- The median duration of exposure to ivosidenib was 3.9 months (range 0.1 to 39.5 months). Sixty-five patients (36%) were exposed to ivosidenib for at least 6 months and 16 patients (9%) were exposed for at least 1 year.
- Serious adverse reactions (≥ 5%) were differentiation syndrome (10%), leukocytosis (10%), and electrocardiogram QT prolonged (7%). There was one case of progressive multifocal leukoencephalopathy (PML).
- The most common adverse reactions leading to dose interruption were electrocardiogram QT prolonged (7%), differentiation syndrome (3%), leukocytosis (3%) and dyspnea (3%). Five out of 179 patients (3%) required a dose reduction due to an adverse reaction. Adverse reactions leading to a dose reduction included electrocardiogram QT prolonged (1%), diarrhea (1%), nausea (1%), decreased hemoglobin (1%), and increased transaminases (1%). Adverse reactions leading to permanent discontinuation included Guillain-Barré syndrome (1%), rash (1%), stomatitis (1%), and creatinine increased (1%).
- The most common adverse reactions reported in the trial are shown in TABLE 4.
- Changes in selected post-baseline laboratory values that were observed in patients with relapsed or refractory AML are shown in TABLE 5.
Postmarketing Experience
There is limited information regarding Ivosidenib Postmarketing Experience in the drug label.
Drug Interactions
Effect of Other Drugs on Ivosidenib
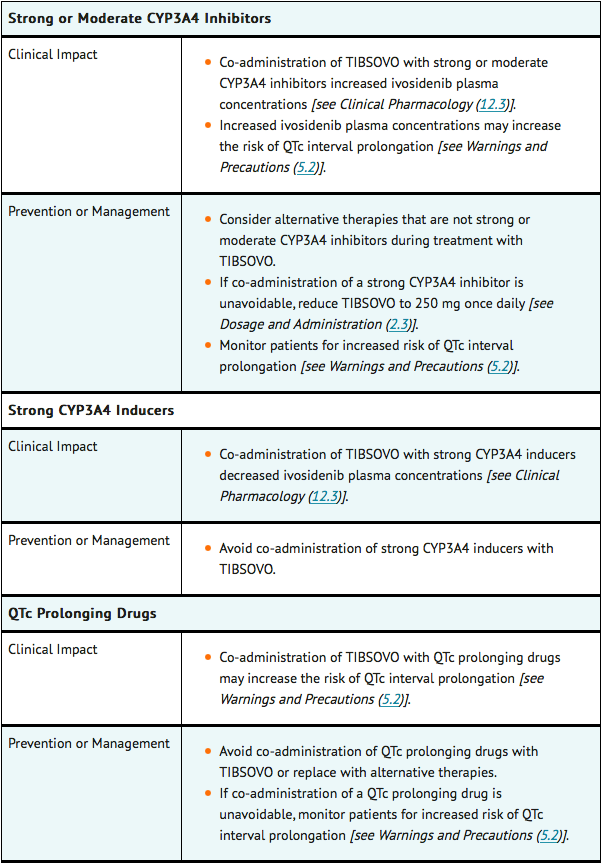
Effect of Ivosidenib on Other Drugs
- Ivosidenib induces CYP3A4 and may induce CYP2C9. Co-administration will decrease concentrations of drugs that are sensitive CYP3A4 substrates and may decrease concentrations of drugs that are sensitive CYP2C9 substrates. Use alternative therapies that are not sensitive substrates of CYP3A4 and CYP2C9 during ivosidenib treatment. Do not administer ivosidenib with itraconazole or ketoconazole (CYP3A4 substrates) due to expected loss of antifungal efficacy. Co-administration of ivosidenib may decrease the concentrations of hormonal contraceptives, consider alternative methods of contraception in patients receiving ivosidenib. If co-administration of ivosidenib with sensitive CYP3A4 substrates or CYP2C9 substrates is unavoidable, monitor patients for loss of therapeutic effect of these drugs.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Risk Summary
- Based on animal embryo-fetal toxicity studies, ivosidenib may cause fetal harm when administered to a pregnant woman. There are no available data on ivosidenib use in pregnant women to inform a drug-associated risk of major birth defects and miscarriage. In animal embryo-fetal toxicity studies, oral administration of ivosidenib to pregnant rats and rabbits during organogenesis was associated with embryo-fetal mortality and alterations to growth starting at 2 times the steady state clinical exposure based on the AUC at the recommended human dose. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, advise the patient of the potential risk to a fetus.
- The background risk of major birth defects and miscarriage for the indicated population is unknown. Adverse outcomes in pregnancy occur regardless of the health of the mother or the use of medications. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2%-4% and 15%-20%, respectively.
Animal Data
- Ivosidenib administered to pregnant rats at a dose of 500 mg/kg/day during organogenesis (gestation days 6-17) was associated with adverse embryo-fetal effects including lower fetal weights, and skeletal variations. These effects occurred in rats at approximately 2 times the human exposure at the recommended dose of 500 mg daily.
- In pregnant rabbits treated during organogenesis (gestation days 7-20), ivosidenib was maternally toxic at doses of 180 mg/kg/day (exposure approximately 3.9 times the human exposure at the recommended dose of 500 mg daily) and caused spontaneous abortions as well as decreased fetal weights, skeletal variations, and visceral variations.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Ivosidenib in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Ivosidenib during labor and delivery.
Nursing Mothers
Risk Summary
- There are no data on the presence of ivosidenib or its metabolites in human milk, the effects on the breastfed child, or the effects on milk production. Because many drugs are excreted in human milk and because of the potential for adverse reactions in breastfed children, advise women not to breastfeed during treatment with ivosidenib and for at least 1 month after the last dose.
Pediatric Use
- The safety and effectiveness of ivosidenib in pediatric patients have not been established.
Geriatic Use
- Thirty-three (97%) of the 34 patients with newly diagnosed AML in the clinical study were 65 years of age or older, and 19 patients (56%) were 75 years or older. One hundred and twelve (63%) of the 179 patients with relapsed or refractory AML in the clinical study were 65 years of age or older and 40 patients (22%) were 75 years or older. No overall differences in effectiveness or safety were observed between patients with relapsed or refractory AML who were 65 years and older and younger patients.
Gender
There is no FDA guidance on the use of Ivosidenib with respect to specific gender populations.
Race
There is no FDA guidance on the use of Ivosidenib with respect to specific racial populations.
Renal Impairment
- No modification of the starting dose is recommended for patients with mild or moderate renal impairment (eGFR ≥ 30 mL/min/1.73m2, MDRD). The pharmacokinetics and safety of ivosidenib in patients with severe renal impairment (eGFR < 30 mL/min/1.73m2, MDRD) or renal impairment requiring dialysis are unknown. For patients with pre-existing severe renal impairment or who are requiring dialysis, consider the risks and potential benefits before initiating treatment with ivosidenib.
Hepatic Impairment
- No modification of the starting dose is recommended for patients with mild or moderate (Child-Pugh A or B) hepatic impairment. The pharmacokinetics and safety of ivosidenib in patients with severe hepatic impairment (Child-Pugh C) are unknown. For patients with pre-existing severe hepatic impairment, consider the risks and potential benefits before initiating treatment with ivosidenib.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Ivosidenib in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Ivosidenib in patients who are immunocompromised.
Administration and Monitoring
Administration
Patient Selection
- Select patients for the treatment of AML with ivosidenib based on the presence of IDH1 mutations in the blood or bone marrow. Patients without IDH1 mutations at diagnosis should be retested at relapse because a mutation in IDH1 may emerge during treatment and at relapse. Information on FDA-approved tests for the detection of IDH1 mutations in AML is available at HTTP://WWW.FDA.GOV/COMPANIONDIAGNOSTICS.
Recommended Dosage
- The recommended dose of ivosidenib is 500 mg taken orally once daily until disease progression or unacceptable toxicity. For patients without disease progression or unacceptable toxicity, treat for a minimum of 6 months to allow time for clinical response.
- Administer ivosidenib with or without food. Do not administer ivosidenib with a high-fat meal because of an increase in ivosidenib concentration. Do not split or crush ivosidenib tablets. Administer ivosidenib tablets orally about the same time each day. If a dose of ivosidenib is vomited, do not administer a replacement dose; wait until the next scheduled dose is due. If a dose of ivosidenib is missed or not taken at the usual time, administer the dose as soon as possible and at least 12 hours prior to the next scheduled dose. Return to the normal schedule the following day. Do not administer 2 doses within 12 hours.
Patients with the Comorbidities of Severe Renal or Severe Hepatic Impairment
- Treatment with ivosidenib has not been studied in patients with pre-existing severe renal or hepatic impairment. For patients with pre-existing severe renal or hepatic impairment, consider the risks and potential benefits before initiating treatment with ivosidenib.
Dose Modification for Use with Strong CYP3A4 Inhibitors
- If a strong CYP3A4 inhibitor must be coadministered, reduce the ivosidenib dose to 250 mg once daily. If the strong inhibitor is discontinued, increase the ivosidenib dose (after at least 5 half-lives of the strong CYP3A4 inhibitor) to the recommended dose of 500 mg once daily.
Monitoring
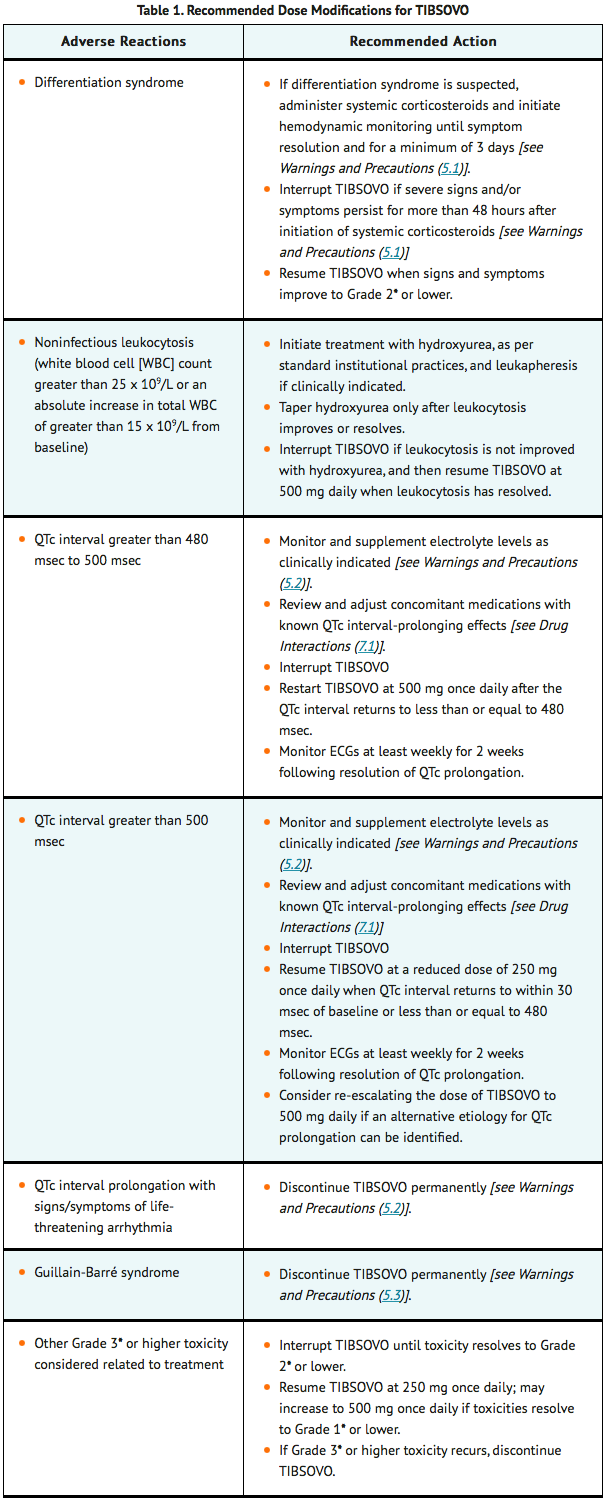
Monitoring and Dose Modifications for Toxicities
- Assess blood counts and blood chemistries prior to the initiation of ivosidenib, at least once weekly for the first month, once every other week for the second month, and once monthly for the duration of therapy. Monitor blood creatine phosphokinase weekly for the first month of therapy. Monitor electrocardiograms (ECGs) at least once weekly for the first 3 weeks of therapy and then at least once monthly for the duration of therapy. Manage any abnormalities promptly.
- Interrupt dosing or reduce dose for toxicities. See TABLE 1 for dose modification guidelines.
IV Compatibility
There is limited information regarding the compatibility of Ivosidenib and IV administrations.
Overdosage
There is limited information regarding Ivosidenib overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
| |
Ivosidenib
| |
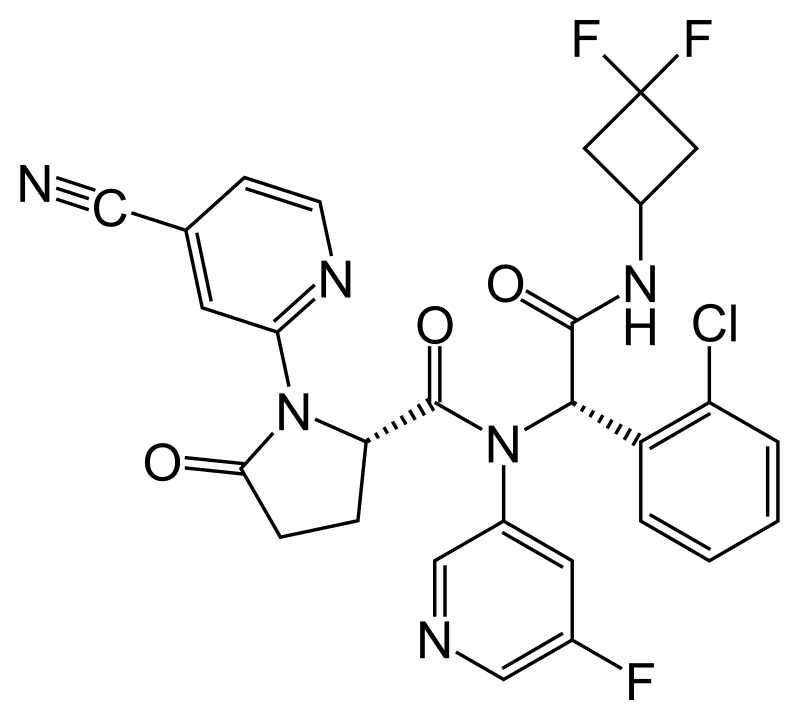
| Systematic (IUPAC) name | |
| (2S)-N-{(1S)-1-(2-chlorophenyl)-2-[(3,3- difluorocyclobutyl)amino]-2-oxoethyl}-1-(4-cyanopyridin2-yl)-N-(5-fluoropyridin-3-yl)-5-oxopyrrolidine2-carboxamide | |
| Identifiers | |
| CAS number | |
| ATC code | L01 |
| PubChem | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | ? |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status |
Investigational |
| Routes | Oral |
Mechanism of Action
- Ivosidenib is a small molecule inhibitor that targets the mutant isocitrate dehydrogenase 1 (IDH1) enzyme. Susceptible IDH1 mutations are defined as those leading to increased levels of 2-hydroxyglutarate (2-HG) in the leukemia cells and where efficacy is predicted by 1) clinically meaningful remissions with the recommended dose of ivosidenib and/or 2) inhibition of mutant IDH1 enzymatic activity at concentrations of ivosidenib sustainable at the recommended dosage according to validated methods. The most common of such mutations are R132H and R132C substitutions.
- Ivosidenib was shown to inhibit selected IDH1 R132 mutants at much lower concentrations than wild-type IDH1 in vitro. Inhibition of the mutant IDH1 enzyme by ivosidenib led to decreased 2-HG levels and induced myeloid differentiation in vitro and in vivo in mouse xenograft models of IDH1-mutated AML. In blood samples from patients with AML with mutated IDH1, ivosidenib decreased 2-HG levels ex-vivo, reduced blast counts, and increased percentages of mature myeloid cells.
Structure
- The molecular formula is C28H22C1F3N6O3 and the molecular weight is 583.0 g/mol. Ivosidenib is practically insoluble in aqueous solutions between pH 1.2 and 7.4. The chemical structure is:
Pharmacodynamics
- Multiple doses of ivosidenib 500 mg daily were observed to decrease plasma 2-HG concentrations in patients with hematological malignancies to levels similar to those observed at baseline in healthy subjects. In bone marrow, 2-HG concentrations were reduced by >90%.
Cardiac Electrophysiology
- A concentration-dependent QTc interval prolongation of approximately 17.2 msec (90% CI: 14.7, 19.7) was observed at the steady-state Cmax following a 500 mg daily dose based on an analysis of 171 patients with advanced hematologic malignances and an IDH1 mutation, including 26 patients with newly diagnosed AML and 136 patients with relapsed or refractory AML, who received ivosidenib 500 mg daily. Co-administration with moderate or strong CYP3A inhibitors is expected to further increase QTc interval prolongation from baseline.
Pharmacokinetics
- The following ivosidenib pharmacokinetic parameters were observed following administration of ivosidenib 500 mg as a single dose or daily dose (for steady-state), unless otherwise specified. The steady-state pharmacokinetics of ivosidenib 500 mg were comparable between patients with newly diagnosed AML and patients with relapsed or refractory AML.
- The mean peak plasma concentration (Cmax) is 4,503 ng/mL [% coefficient of variation (%CV: 38)] after a single dose, and 6,551 ng/mL (%CV: 44) at steady-state. The steady-state area under the concentration time curve (AUC) is 117,348 ng·hr/mL (%CV: 50).
- The AUC and Cmax of ivosidenib increase in a less than dose-proportional manner from 200 mg to 1,200 mg daily (0.4 to 2.4 times the approved recommended dosage). Accumulation ratios were approximately 1.9 for AUC and 1.5 for Cmax over one month. Steady-state plasma levels are reached within 14 days.
Absorption
- The median time to Cmax is approximately 3 hours.
Effect of Food
- Following administration of a single dose in healthy subjects, a high-fat meal (approximately 900 to 1,000 calories, 500 to 600 fat calories, 250 carbohydrate calories and 150 protein calories) increased ivosidenib Cmax by 98% (90% CI: 79%, 119%) and AUCinf by approximately 25%.
Distribution
- The mean apparent volume of distribution of ivosidenib at steady-state is 234 L (%CV: 47). Protein binding of ivosidenib ranges from 92 to 96% in vitro.
Elimination
- Ivosidenib has a terminal half-life of 93 hours (%CV: 67) and an apparent clearance (CL/F) of 4.3 L/hour (%CV: 50).
Metabolism
- Ivosidenib is the predominant component (>92%) of total radioactivity in plasma. Ivosidenib is primarily metabolized by CYP3A4 with minor contributions by N-dealkylation and hydrolytic pathways.
Excretion
- After a single oral administration of radiolabeled ivosidenib to healthy subjects, 77% of ivosidenib was eliminated in the feces (67% as unchanged) and 17% in the urine (10% as unchanged).
Specific Populations
- No clinically meaningful effects on the pharmacokinetics of ivosidenib were observed based on age (18 years to 89 years), sex, race (White, Asian, Black or African American), body weight (38 to 150 kg), ECOG performance status, or mild or moderate renal impairment (eGFR ≥30 mL/min/1.73m2, MDRD). The pharmacokinetics of ivosidenib in patients with severe renal impairment (eGFR <30 mL/min/1.73m2, MDRD) or renal impairment requiring dialysis is unknown.
Patients with Hepatic Impairment
- Following a single dose of ivosidenib 500 mg, the geometric mean ratio (90% confidence interval) of ivosidenib systemic exposure (AUC0-INF) in subjects with mild hepatic impairment (Child-Pugh A) was 0.85 (0.62, 1.15) and moderate hepatic impairment (Child-Pugh B) was 0.71 (0.48, 1.05) as compared to that in subjects with normal hepatic function. The pharmacokinetics of ivosidenib in patients with severe hepatic impairment (Child-Pugh C) is unknown.
Drug Interaction Studies
Clinical Studies and Model-Based Approaches
Effect of Strong or Moderate CYP3A4 Inhibitors on Ivosidenib
- Itraconazole was used as a strong CYP3A4 index inhibitor to evaluate the effect of CYP3A4 inhibition on the pharmacokinetics of ivosidenib single-dose in a drug-drug interaction study in healthy subjects. Co-administration of 250 mg ivosidenib with itraconazole (200 mg itraconazole once daily for 18 days) increased ivosidenib single-dose AUC to 269% of control (90% CI: 245%, 295%) with no change in Cmax. In regards to multiple-dosing, note that because ivosidenib induces the metabolism of CYP3A4 substrates following ivosidenib multiple dosing, itraconazole (a CYP3A4 substrate) is not recommended to be used concomitantly with ivosidenib in patients.
- Based on physiologically-based pharmacokinetic modeling, co-administration of 500 mg ivosidenib with the moderate CYP3A4 inhibitor fluconazole (dosed to steady-state) is predicted to increase ivosidenib single-dose AUC to 173% of control with no change in Cmax. In regards to multiple-dosing, co-administration with ivosidenib and fluconazole is predicted to increase ivosidenib steady-state Cmax to 152% of control and AUC to 190% of control.
Effect of Strong CYP3A4 Inducers on Ivosidenib
- Co-administration of ivosidenib with a strong CYP3A4 inducer (600 mg rifampin once daily for 15 days) is predicted to decrease ivosidenib steady-state AUC by 33%.
Effect of Ivosidenib on CYP3A4 Substrates
- Ivosidenib induces CYP3A4, including its own metabolism. Co-administration of ivosidenib with CYP3A4 substrates such as itraconazole is expected to decrease itraconazole steady-state AUC to a clinically relevant extent.
Effect of Gastric Acid Reducing Agents on Ivosidenib
- Gastric acid reducing agents (e.g., proton pump inhibitors, H2-receptor antagonists, antacids) do not affect ivosidenib concentrations.
In vitro Studies
Metabolic Pathways
- Ivosidenib may induce CYP2B6, CYP2C8, and CYP2C9 and therefore may affect the pharmacokinetics of sensitive substrates of these enzymes.
Drug Transporter Systems
- Ivosidenib is a substrate for P-glycoprotein (P-gp). Ivosidenib is not a substrate for BCRP or hepatic transporters OATP1B1 and OATP1B3.
- Ivosidenib does not inhibit BCRP, OATP1B1, OATP1B3, OAT1, and OCT2 at clinically relevant concentrations. Ivosidenib is an inhibitor of OAT3 and P-gp.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Carcinogenicity studies have not been conducted with ivosidenib. Ivosidenib was not mutagenic in an in vitro bacterial reverse mutation (Ames) assay. Ivosidenib was not clastogenic in an in vitro human lymphocyte micronucleus assay, or in an in vivo rat bone marrow micronucleus assay. Fertility studies in animals have not been conducted with ivosidenib. In repeat-dose toxicity studies up to 90 days in duration with twice daily oral administration of ivosidenib in rats, uterine atrophy was reported in females at non-tolerated dose levels.
Clinical Studies
Newly-Diagnosed AML
- The efficacy of ivosidenib was evaluated in an open-label, single-arm, multicenter clinical trial (Study AG120-C-001, NCT02074839) that included 28 adult patients with newly-diagnosed AML with an IDH1 mutation. IDH1 mutations were identified by a local or central diagnostic test and confirmed retrospectively using the Abbott RealTime™ IDH1 Assay. The cohort included patients who were age 75 years or older or who had comorbidities that precluded the use of intensive induction chemotherapy based on at least one of the following criteria: baseline Eastern Cooperative Oncology Group (ECOG) performance status of ≥ 2, severe cardiac or pulmonary disease, hepatic impairment with bilirubin > 1.5 times the upper limit of normal, or creatinine clearance < 45 mL/min. Ivosidenib was given orally at a starting dose of 500 mg daily until disease progression, development of unacceptable toxicity, or undergoing hematopoietic stem cell transplantation. Two (7%) of the 28 patients went on to stem cell transplantation following ivosidenib treatment.
- The baseline demographic and disease characteristics are shown in TABLE 6.
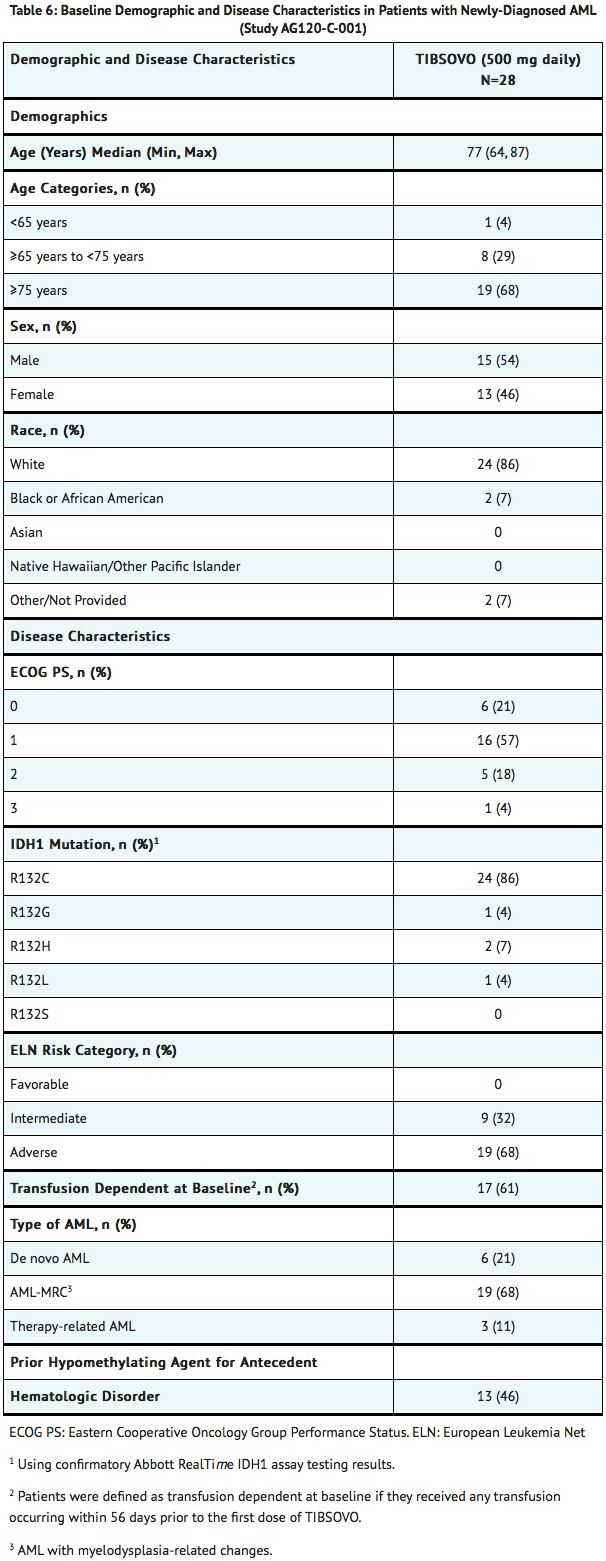
- Efficacy was established on the basis of the rate of complete remission (CR) or complete remission with partial hematologic recovery (CRh), the duration of CR+CRh, and the rate of conversion from transfusion dependence to transfusion independence. The efficacy results are shown in TABLE 7. The median follow-up was 8.1 months (range, 0.6 to 40.9 months) and median treatment duration was 4.3 months (range, 0.3 to 40.9 months).
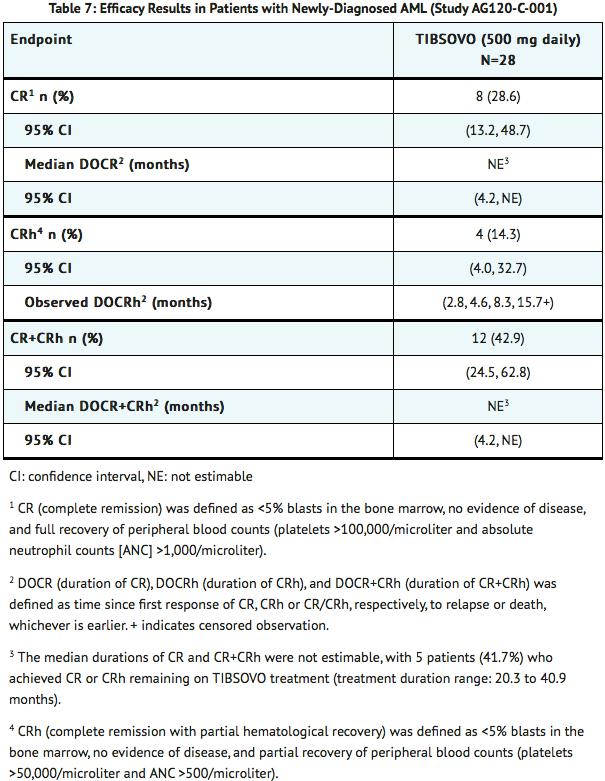
- For patients who achieved a CR or CRh, the median time to CR or CRh was 2.8 months (range, 1.9 to 12.9 months). Of the 12 patients who achieved a best response of CR or CRh, 11 (92%) achieved a first response of CR or CRh within 6 months of initiating ivosidenib.
- Among the 17 patients who were dependent on red blood cell (RBC) and/or platelet transfusions at baseline, 7 (41.2%) became independent of RBC and platelet transfusions during any 56-day post-baseline period. Of the 11 patients who were independent of both RBC and platelet transfusions at baseline, 6 (54.5%) remained transfusion independent during any 56-day post-baseline period.
Relapsed or Refractory AML
- The efficacy of ivosidenib was evaluated in an open-label, single-arm, multicenter clinical trial (Study AG120-C-001, NCT02074839) of 174 adult patients with relapsed or refractory AML with an IDH1 mutation. IDH1 mutations were identified by a local or central diagnostic test and confirmed retrospectively using the Abbott RealTime™ IDH1 Assay. Ivosidenib was given orally at a starting dose of 500 mg daily until disease progression, development of unacceptable toxicity, or undergoing hematopoietic stem cell transplantation. Twenty-one (12%) of the 174 patients went on to stem cell transplantation following ivosidenib treatment.
- The baseline demographic and disease characteristics are shown in TABLE 8.
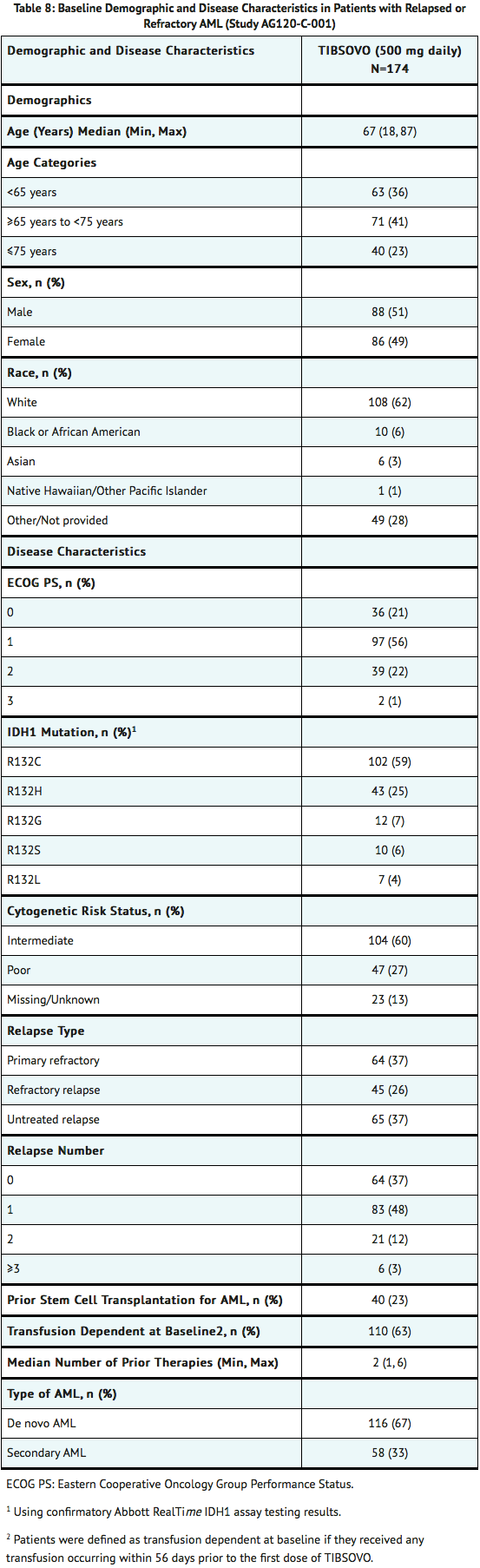
- Efficacy was established on the basis of the rate of complete remission (CR) plus complete remission with partial hematologic recovery (CRh), the duration of CR+CRh, and the rate of conversion from transfusion dependence to transfusion independence. The efficacy results are shown in TABLE 9. The median follow-up was 8.3 months (range, 0.2 to 39.5 months) and median treatment duration was 4.1 months (range, 0.1 to 39.5 months).
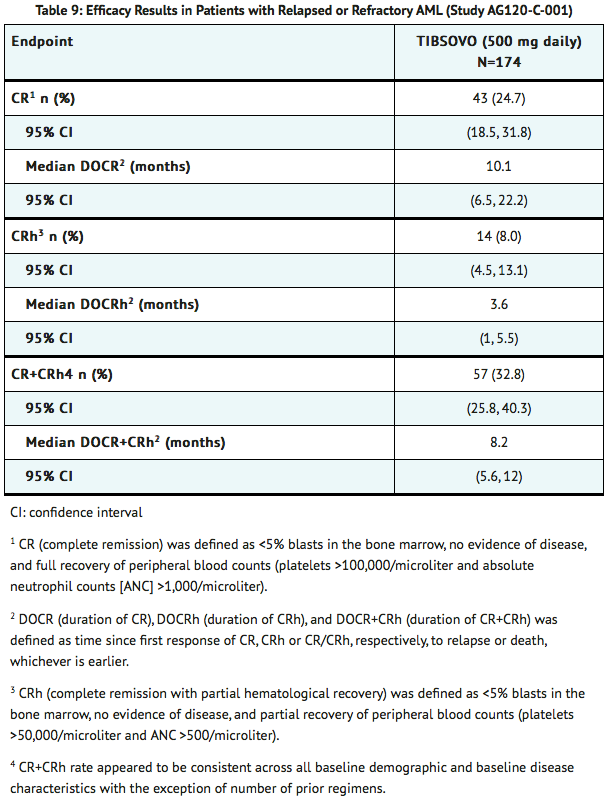
- For patients who achieved a CR or CRh, the median time to CR or CRh was 2 months (range, 0.9 to 5.6 months). Of the 57 patients who achieved a best response of CR or CRh, all achieved a first response of CR or CRh within 6 months of initiating ivosidenib.
- Among the 110 patients who were dependent on red blood cell (RBC) and/or platelet transfusions at baseline, 41 (37.3%) became independent of RBC and platelet transfusions during any 56-day post-baseline period. Of the 64 patients who were independent of both RBC and platelet transfusions at baseline, 38 (59.4%) remained transfusion independent during any 56-day post-baseline period.
How Supplied
- 250 mg tablet: Blue oval-shaped film-coated tablet debossed “IVO” on one side and “250” on the other side.
- 60-count bottles of 250 mg tablets with a desiccant canister.
Storage
- Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C to 30°C (59°F to 86°F).
Images
Drug Images
{{#ask: Page Name::Ivosidenib |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

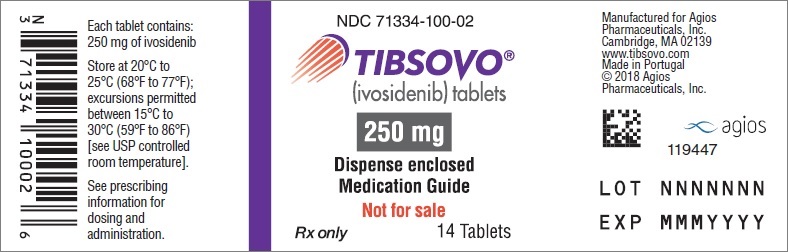
{{#ask: Label Page::Ivosidenib |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise the patient to read the FDA-approved patient labeling (MEDICATION GUIDE).
Differentiation Syndrome
- Advise patients of the risks of developing differentiation syndrome as early as 1 day after start of therapy and during the first 3 months on treatment. Ask patients to immediately report any symptoms suggestive of differentiation syndrome, such as fever, cough or difficulty breathing, rash, decreased urinary output, low blood pressure, rapid weight gain, or swelling of their arms or legs, to their healthcare provider for further evaluation.
QTc Interval Prolongation
- Inform patients of symptoms that may be indicative of significant QTc interval prolongation including dizziness, lightheadedness, and fainting. Advise patients to report these symptoms and the use of all medications to their healthcare provider.
Drug Interactions
- Advise patients to inform their healthcare providers of all concomitant medications, including over-the-counter medications, vitamins, and herbal products.
Guillain-Barré Syndrome
- Inform patients of symptoms that may be indicative of Guillain-Barré syndrome, including new signs or symptoms of motor and/or sensory neuropathy, such as weakness or tingling sensation in the legs, arms, or upper body, numbness and pain on one side or both sides of the body, changes to any sensory function, or burning or prickling sensation, or difficulty breathing. Advise patients to report these symptoms to their healthcare provider.
Tumor Lysis Syndrome
- Advise patients on the risks of developing tumor lysis syndrome. Advise patients on the importance of maintaining high fluid intake, and the need for frequent monitoring of blood chemistry values.
Gastrointestinal Adverse Reactions
- Advise patients on the risks of experiencing gastrointestinal reactions such as diarrhea, nausea, mucositis, constipation, vomiting, decreased appetite and abdominal pain. Ask patients to report these events to their healthcare provider, and advise patients how to manage them.
Lactation
- Advise women not to breastfeed during treatment with ivosidenib and for at least 1 month after the final dose
Dosing and Storage Instructions
- Advise patients to swallow tablets whole and to not split, crush, or chew ivosidenib tablets.
- Advise patients to avoid taking ivosidenib with a high-fat meal.
- Instruct patients that if a dose of ivosidenib is vomited, not to take an additional dose, and wait until the next scheduled dose is due. If a dose of ivosidenib is missed or not taken at the usual time, instruct patients to take the dose as soon as possible unless the next dose is due within 12 hours. Patients can return to the normal schedule the following day.
- Store ivosidenib at room temperature from 20°C to 25°C (68°F to 77°F).
Medication Guide
Precautions with Alcohol
Alcohol-Ivosidenib interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
Look-Alike Drug Names
There is limited information regarding Ivosidenib Look-Alike Drug Names in the drug label.
Price
References
The contents of this FDA label are provided by the National Library of Medicine.