Hypertrophic cardiomyopathy electrocardiogram
|
Hypertrophic Cardiomyopathy Microchapters |
|
Differentiating Hypertrophic Cardiomyopathy from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Hypertrophic cardiomyopathy electrocardiogram On the Web |
|
Directions to Hospitals Treating Hypertrophic cardiomyopathy |
|
Risk calculators and risk factors for Hypertrophic cardiomyopathy electrocardiogram |
Editors-In-Chief: C. Michael Gibson, M.S., M.D. [1], Martin S. Maron, M.D., and Barry J. Maron, M.D. Soroush Seifirad, M.D.[2]
Overview
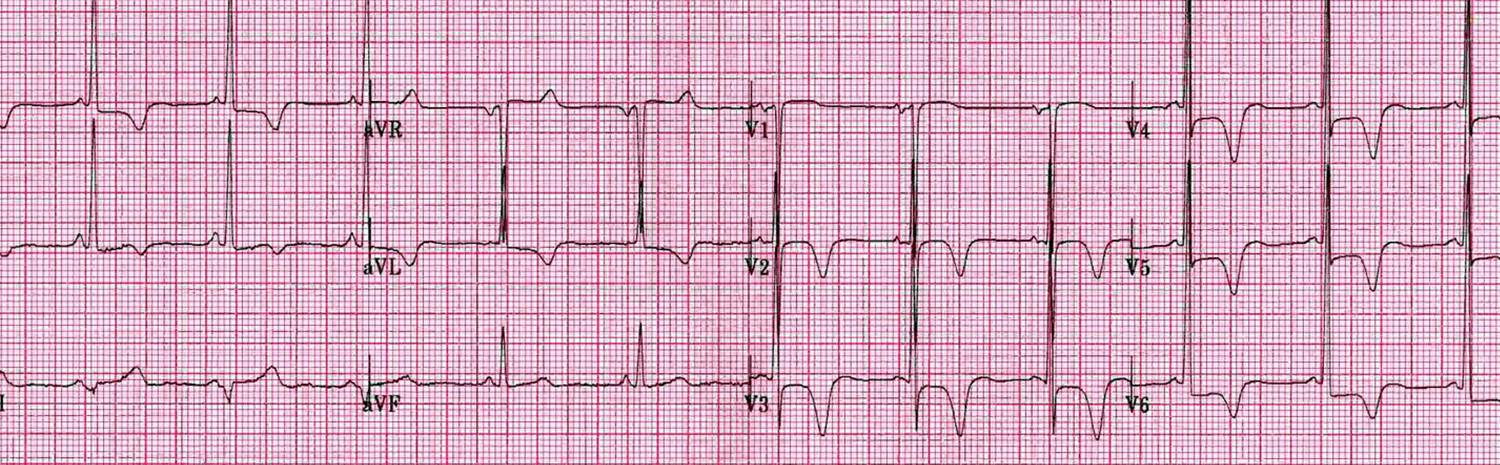
A 12 lead EKG is strongly recommended at the time of the initial diagnosis of hypertrophic cardiomyopathy. Common findings on an EKG in these patients include tall R waves, deep Q waves, inverted T waves, ST segment abnormalities and 'strain pattern' in the chest leads. The deep Q waves indicate septal hypertrophy and similarly deeply inverted T waves indicate apical hypertrophy.
Electrocardiogram
Large septal Q waves may be present reflective of the septal hypertrophy. In the Yamaguchi variant of apical hypertrophic cardiomyopathy, there may be deeply inverted T waves in precordial leads V2-V6 and II, III, aVL (see example).
Shown below is an example of a variant of apical hypertrophic cardiomyopathy with deeply inverted T waves in precordial leads V2-V6 and II, III, aVL.

Shown below is an example of hypertrophic cardiomyopathy with abnormal ST segments, deeply flipped T waves, tall R apical waves, deep Q waves. "Strain pattern" can be observed in the precordial leads.

Shown below is an example of hypertrophic cardiomyopathy with ST depression in the lateral leads, deeper S waves in the right precordial leads and tall R waves in the left precordial leads with T wave inversions indicating "strain pattern".
Yamagouchi
Yamaguchi syndrome or apical hypertrophy pseudoacute coronary syndrome might be observed on ECG. ECG findings might show left ventricular hypertrophy as well as diffuse T-wave inversions over the inferior and anterolateral leads
2020 AHA/ACC Guideline for the Diagnosis and Treatment of Patients With Hypertrophic Cardiomyopathy A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines[1]
Recommendations for Heart Rhythm Assessment Referenced studies that support the recommendations are summarized in Online Data Supplement
| Class I |
| 1. In patients with HCM, a 12-lead ECG is recommended in the initial evaluation and as part of periodic follow-up (every 1 to 2 years)(Level of Evidence: B-NR)
2. In patients with HCM, 24- to 48-hour ambulatory electrocardiographic monitoring is recommended in the initial evaluation and as part of periodic follow-up (every 1 to 2 years) to identify patients who are at risk for SCD and guide management of arrhythmias(Level of Evidence: B-NR) 3. In patients with HCM who develop palpitations or lightheadedness, extended (>24 hours) electrocardiographic monitoring or event recording is recommended, which should not be considered diagnostic unless patients have had symptoms while being monitored(Level of Evidence: B-NR) 4. In first-degree relatives of patients with HCM, a 12-lead ECG is recommended as a component of the screening algorithm(Level of Evidence: B-NR) |
| Class IIa |
| 5. In patients with HCM who have additional risk factors for AF, such as left atrial dilatation, advanced age, and New York Heart Association (NYHA) class III to class IV HF, and who are eligible for anticoagulation, extended ambulatory monitoring is reasonable to screen for AF as part of initial evaluation and periodic follow-up (every 1 to 2 years)(Level of Evidence: B-NR) |
| Class IIb |
| 6. In adult patients with HCM without risk fac-tors for AF and who are eligible for anticoagulation, extended ambulatory monitoring may be considered to assess for asymptomatic paroxysmal AF as part of initial evaluation and periodic follow-up (every 1 to 2 years)(Level of Evidence: B-NR) |
2011 ACCF/AHA Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy (DO NOT EDIT)[2]
Genotype-Positive/Phenotype-Negative Patients (DO NOT EDIT)[2]
| Class I |
| "1. In individuals with pathogenic mutations who do not express the HCM phenotype, it is recommended to perform serial electrocardiogram (ECG), transthoracic echocardiogram (TTE), and clinical assessment at periodic intervals (12 to 18 months in children and adolescents and about every 5 years in adults), based on the patient’s age and change in clinical status.[3][4][5][6] (Level of Evidence: B)" |
Electrocardiography (DO NOT EDIT)[2]
| Class I |
| "1. A 12-lead ECG is recommended in the initial evaluation of patients with HCM. (Level of Evidence: C)" |
| "2. Twenty-four–hour ambulatory (Holter) electrocardiographic monitoring is recommended in the initial evaluation of patients with HCM to detect ventricular tachycardia (VT) and identify patients who may be candidates for ICD therapy.[5][7][8][9] (Level of Evidence: B)" |
| "3. Twenty-four–hour ambulatory (Holter) electrocardiographic monitoring or event recording is recommended in patients with HCM who develop palpitations or lightheadedness.[5][7][8] (Level of Evidence: B)" |
| "4. A repeat ECG is recommended for patients with HCM when there is worsening of symptoms. (Level of Evidence: C)" |
| "5. A 12-lead ECG is recommended every 12 to 18 months as a component of the screening algorithm for adolescent first-degree relatives of patients with HCM who have no evidence of hypertrophy on echocardiography. (Level of Evidence: C)" |
| "6. A 12-lead ECG is recommended as a component of the screening algorithm for first-degree relatives of patients with HCM. (Level of Evidence: C)" |
| Class IIa |
| "1. Twenty-four–hour ambulatory (Holter) electrocardiographic monitoring, repeated every 1 to 2 years, is reasonable in patients with HCM who have no previous evidence of VT to identify patients who may be candidates for ICD therapy.[9] (Level of Evidence: C)" |
| "2. Annual 12-lead ECGs are reasonable in patients with known HCM who are clinically stable to evaluate for asymptomatic changes in conduction or rhythm (i.e., atrial fibrillation (AF)). (Level of Evidence: C)" |
| Class IIb |
| "1. Twenty-four–hour ambulatory (Holter) electrocardiographic monitoring might be considered in adults with HCM to assess for asymptomatic paroxysmal AF/atrial flutter. (Level of Evidence: C)" |
References
- ↑ Ommen SR, Mital S, Burke MA, Day SM, Deswal A, Elliott P; et al. (2020). "2020 AHA/ACC Guideline for the Diagnosis and Treatment of Patients With Hypertrophic Cardiomyopathy: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines". Circulation. 142 (25): e558–e631. doi:10.1161/CIR.0000000000000937. PMID 33215931 Check
|pmid=value (help). - ↑ 2.0 2.1 2.2 Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, Naidu SS, Nishimura RA, Ommen SR, Rakowski H, Seidman CE, Towbin JA, Udelson JE, Yancy CW (2011). "2011 ACCF/AHA Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Developed in Collaboration With the American Association for Thoracic Surgery, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Journal of the American College of Cardiology. 58 (25): e212–60. doi:10.1016/j.jacc.2011.06.011. PMID 22075469. Retrieved 2011-12-19. Unknown parameter
|month=ignored (help) - ↑ Christiaans I, Lekanne dit Deprez RH, van Langen IM, Wilde AA (2009). "Ventricular fibrillation in MYH7-related hypertrophic cardiomyopathy before onset of ventricular hypertrophy". Heart Rhythm : the Official Journal of the Heart Rhythm Society. 6 (9): 1366–9. doi:10.1016/j.hrthm.2009.04.029. PMID 19539541. Retrieved 2011-12-22. Unknown parameter
|month=ignored (help) - ↑ Andersen PS, Havndrup O, Hougs L, Sørensen KM, Jensen M, Larsen LA, Hedley P, Thomsen AR, Moolman-Smook J, Christiansen M, Bundgaard H (2009). "Diagnostic yield, interpretation, and clinical utility of mutation screening of sarcomere encoding genes in Danish hypertrophic cardiomyopathy patients and relatives". Human Mutation. 30 (3): 363–70. doi:10.1002/humu.20862. PMID 19035361. Retrieved 2011-12-22. Unknown parameter
|month=ignored (help) - ↑ 5.0 5.1 5.2 Christiaans I, Birnie E, van Langen IM, van Spaendonck-Zwarts KY, van Tintelen JP, van den Berg MP, Atsma DE, Helderman-van den Enden AT, Pinto YM, Hermans-van Ast JF, Bonsel GJ, Wilde AA (2010). "The yield of risk stratification for sudden cardiac death in hypertrophic cardiomyopathy myosin-binding protein C gene mutation carriers: focus on predictive screening". European Heart Journal. 31 (7): 842–8. doi:10.1093/eurheartj/ehp539. PMID 20019025. Retrieved 2011-12-22. Unknown parameter
|month=ignored (help) - ↑ Michels M, Soliman OI, Phefferkorn J, Hoedemaekers YM, Kofflard MJ, Dooijes D, Majoor-Krakauer D, Ten Cate FJ (2009). "Disease penetrance and risk stratification for sudden cardiac death in asymptomatic hypertrophic cardiomyopathy mutation carriers". European Heart Journal. 30 (21): 2593–8. doi:10.1093/eurheartj/ehp306. PMID 19666645. Retrieved 2011-12-22. Unknown parameter
|month=ignored (help) - ↑ 7.0 7.1 Elliott PM, Gimeno JR, Tomé MT, Shah J, Ward D, Thaman R, Mogensen J, McKenna WJ (2006). "Left ventricular outflow tract obstruction and sudden death risk in patients with hypertrophic cardiomyopathy". European Heart Journal. 27 (16): 1933–41. doi:10.1093/eurheartj/ehl041. PMID 16754630. Retrieved 2011-12-22. Unknown parameter
|month=ignored (help) - ↑ 8.0 8.1 Maron BJ, Savage DD, Wolfson JK, Epstein SE (1981). "Prognostic significance of 24 hour ambulatory electrocardiographic monitoring in patients with hypertrophic cardiomyopathy: a prospective study". The American Journal of Cardiology. 48 (2): 252–7. PMID 7196685. Retrieved 2011-12-22. Unknown parameter
|month=ignored (help) - ↑ 9.0 9.1 Monserrat L, Elliott PM, Gimeno JR, Sharma S, Penas-Lado M, McKenna WJ (2003). "Non-sustained ventricular tachycardia in hypertrophic cardiomyopathy: an independent marker of sudden death risk in young patients". Journal of the American College of Cardiology. 42 (5): 873–9. PMID 12957435. Retrieved 2011-12-22. Unknown parameter
|month=ignored (help)