Hip fracture
|
WikiDoc Resources for Hip fracture |
|
Articles |
|---|
|
Most recent articles on Hip fracture Most cited articles on Hip fracture |
|
Media |
|
Powerpoint slides on Hip fracture |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Hip fracture at Clinical Trials.gov Clinical Trials on Hip fracture at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Hip fracture
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Hip fracture Discussion groups on Hip fracture Patient Handouts on Hip fracture Directions to Hospitals Treating Hip fracture Risk calculators and risk factors for Hip fracture
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Hip fracture |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohammadmain Rezazadehsaatlou[2].
The "hip" joint is known as a ball-and-socket joint. It allows the femur bone to bend and rotate at the pelvis. Comparing to the injuries to the knee, ankle, and shoulder which are well documented, injuries to the hip, pelvis, and thigh get little attentions due to their lower prevalence. A hip fracture is a known as a fracture of the upper quarter of the femur bone while any other types of injuries to the socket, or acetabulum, itself is not considered a "hip fracture." Management of fractures to the socket is a completely different consideration. The hip fracture count as a serious problems associated with serious and life-threatening complications. Hip fractures most commonly occur due to the:
- Fall to the side of the hip
- A direct blow to the side of the hip
- Other medical conditions such as osteoporosis, cancer, or stress injuries affecting the strength.
During fracture the most common site of fracture are:
- The head of the femur
- The neck of the femur
- Between or below the greater trochanter and the lesser trochanters
Historical Perspective
There are no reliable information regarding the historical perspective of the hip bone fracture.
The main etiology of the hip fracture is thought to be a loading may be placed on a leg during falling or from a direct blow to the side of the hip. The main cause of hip fracture is trauma. Such as the most fractures the hip fracture is caused by a falling or automobile accident. Meanwhile, the normal healthy bones are extremely tough and resilient and can withstand most powerful impacts. As a person age, two factors cause higher risk of fractures:
- Weaker bones
- Greater risk of falling
Stress fractures as a common causes of fractures can be found due to the repeated stresses and strains. Importantly children having more physically active lifestyles than adults, are also prone to fractures. People with any underlying diseases such as osteoporosis, infection, or a tumor affecting their bones having a higher risk of fractures. As mentioned in previous chapters, this type of fracture is known as a pathological fracture. Stress fractures, which result from repeated stresses and strains, commonly found among professional sports people, are also common causes of fractures.
Life-threatening Causes
- There are no life-threatening causes of hip fracture , however complications resulting from hip fracture is common.
Common Causes
Common causes of hip fracture may include:
Less Common Causes
Less common causes of hip fracture include conditions that predisposes to fracture:
Causes by Organ System
| Cardiovascular | No underlying causes |
| Chemical/Poisoning | No underlying causes |
| Dental | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | No underlying causes |
| Ear Nose Throat | No underlying causes |
| Endocrine | No underlying causes |
| Environmental | No underlying causes |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | No underlying causes |
| Iatrogenic | No underlying causes |
| Infectious Disease | No underlying causes |
| Musculoskeletal/Orthopedic | Osteoporosis and osteopenia. |
| Neurologic | No underlying causes |
| Nutritional/Metabolic | Osteoporosis and osteopenia. |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | No underlying causes |
| Ophthalmologic | No underlying causes |
| Overdose/Toxicity | No underlying causes |
| Psychiatric | No underlying causes |
| Pulmonary | No underlying causes |
| Renal/Electrolyte | No underlying causes |
| Rheumatology/Immunology/Allergy | No underlying causes |
| Sexual | No underlying causes |
| Trauma | Falling of car accident to on side of hip. |
| Urologic | No underlying causes |
| Miscellaneous | No underlying causes |
Causes in Alphabetical Order
List the causes of the disease in alphabetical order:
Mechanism [14]
The hip fracture is caused by a fall or from a direct blow to the side of the hip. The form and severity of this fracture depends on the position of the hip joint at the moment of hitting the ground. The width of this mentioned angle affects the localization of the fracture. Pronation, supination and abduction positions leads the direction of the force and the compression of carpus and different appearances of injury. Its known that the hip fracture in normal healthy adults can be caused due to the high-energy trauma (e.g., motor vehicle accidents), sport related injuries, falling from height. But it should be noted that the most important Risk factors for insufficiency fractures is chronic metabolic disease such as steoporosis, osteopenia, eating-disordered behavior, higher age, prolonged corticosteroid usage, female gender, lower BMI, history of a recent falling, and prior fracture. Its been said that If the elbow is flexed during the falling, the chance of a type II or III lesion is high.
The pattern of bone fracture and severity of injury depends on variety of factors such as:
- Patients age
- Patients Weight
- Patients past medical history specifically any bone diseases affecting the quality of bone (such as osteoporosis, malignancies)
- Energy of trauma
- Bone quality
- Position of the specific organ during the trauma
- The below-mentioned processes cause decreased bone mass density:
- Autophagy is the mechanism through which osteocytes evade oxidative stress.
- The capability of autophagy in cells decreases as they age, a major factor of aging.
- As osteocytes grow, viability of cells decrease thereby decreasing the bone mass density
Differentiating Hip fracture from other Diseases[16][14][13][12]
In the orthopedic medicine its important to know that the Hip fracture should be evaluated using radiography for both confirming diagnosis and also for evaluating the surrounding tissues. Other injuries such as possible femoral fracture-dislocation or collateral ligament injury, might be seen in Hip fracture. If the mechanism of injury suggests particularly low energy then the Osteoporosis should be considered. The pathological Fractures occurring in a bone with a tumor or Paget's disease) are rare but possible[3]. Also it should be noted that the both bone fractures can be complicated by acute compartment syndrome. Signs suggesting compartment syndrome are pain on extension of digits, and marked edema[3]. As another important fact in orthopedic fracture is if both-bone fractures were found in pediatric which is common after accidental trauma, but it may also be the due to the of child abuse; and in these cases a careful attention and evaluation should be considered if a child abuse is suspected.
- Hip Pointer
- Hip Tendonitis and Bursitis
- Acetabular fracture
- Snapping Hip Syndrome
- Slipped Capital Femoral Epiphysis
- Femoral Neck Stress Fracture
- Femoral head fracture
- Femoral Head Avascular Necrosis
- Femoral Neck Fracture
- Femoral Injuries and Fractures
- Femoral Neck Fracture
- Femoral shaft Fracture
- Iliopsoas Tendinitis
- Slipped Capital Femoral Epiphysis
- Pubic rami fracture
- Osteitis Pubis
- Septic hip
The Hip fracture is an important problem of all ages specially for the older people. It is most commonly occurs in women. The available epidemiological information differed between countries, but totally it's been globally estimated that hip fractures affect around 5%% of men and 20% of women worldwide. Also, the total number of hip fractures is predicted to increase from 1.26 million in 1990 to around 5 million by the year 2050. In the United States the hip fractures occurred in 280,000 Americans per year at a rate of over 5000 per week and it was estimated that its incidence will rise to over 500,000 annually over the next 40 years. And, this type of fracture cost the US approximately $7.2 billion annually and it is estimated that this cost will rise up to 16 billion USD annually by the year 2041. It should be noted that in the United States, the hip fracture and related mortality among persons older than 65 years of age is declining, while related comorbidities have increased.
The Pathophysiology of hip fractures is multifactorial, but the related risk factors for this condition can be divided into two main subgroups: risk factors decreasing bone mineral density (BMD) risk factors increasing the rate of falls
Meanwhile, there are different risk factors that presidpose patient for the Hip fracture that include::
- High-risk contact sports
- Higher age (elderly adults are higher prone to such fractures)
- Low body frame size
- Low BMI
- Reduced exposure to sunlight
- Direct trauma
- Road / traffic accidents
- Falling
- Gunshot wounds
- Domestic violence
- Falling
- Glucocorticoid use
- Anabolic steroid use
- Paget disease of the bone
- Female sex
- Alcohol and tobacco
- Medical problems
- Physical inactivity
- Homocysteine
- Osteoporosis
- osteomalacia
- osteopetrosis
- osteogenesis imperfecta
- Metastatic disorders affecting the bone system
- Infection in the bone which is a rare cause of hip bone fracture.
Hip fractures classified into:
Intracapsular fractures (known as femoral neck fractures):
45% of all acute hip fractures in the elderly
Usually due to a low-impact fall from a standing position or from twisting on a planted foot
Femoral neck fractures are susceptible to malunion and avascular necrosis of the femoral head
further Classification based on radiographic findings
- Type 1: undisplaced and incomplete fracture
- Type 2: undisplaced complete fracture
- Type 3: complete fracture but incompletely displaced
- Type 4: complete fracture and completely displaced
Extracapsular fractures
A: Intertrochanteric fracture:
- Between the greater and the lesser trochanter
- Common in the osteoporotic elderly population
- Due to a fall from a standing height with direct contact of the lateral thigh or torsion of the lower extremity.
- avascular necrosis or nonunion is rare.
B: Subtronchanteric fracture:
- Below the lesser trochanter, approximately 2.5 inches below
- 5% due to tumor, bone cysts, or Paget’s disease.
- 50% due to osteoporosis
- almost all of cases have osteopenia
The most common types of the hip fractures :
- Femoral neck fracture: common among older adults and related to osteoporosis. Complication: cuts off the blood supply to the head of the femur which forms the hip joint.
- Intertrochanteric hip fracture: An intertrochanteric hip fracture occurs three to four inches from the hip joint. Complication: Normally does not interrupt the blood supply to the hip joint.

| Area of invovlement | Classification | ||
|---|---|---|---|
| Femoral head | Pipkin classification |
| |
| Femoral neck | Subcapital | Garden classification |
|
| Transcervical | Pauwel's classification |
| |
| Basicervical | |||
| Trochanteric | Intertrochanteric (between the greater and lesser trochanter) | Ramadier's classification
Ramadier's classification (1956) Boyd and Griffin's classification (1949) Decoulx & Lavarde's classification (1969) Ender's classification (1970) Tronzo's classification (1973) Evans-Jensen classification (1975) Deburge's classification (1976) Briot's classification (1980) |
Evans-Jensen classification (1975)
B: 2-part displaced
|
| Pertrochanteric (through the trochanters) | |||
| Subtrochanteric | Seinsheimer classification |
C: 2-part spiral fracture with lesser trochanter attached to the distal fragment
| |
| American Academy of Orthopedic Surgeons (AAOS) classification |
|
Fractures are classified accordingly:
|
|
| Cooke and Newman (modified Bethea) classification |
|
||
| Johansson classification |
|
||
| Vancouver classification |
|
Osteoporosis is an important risk factor for human affecting human bone especially in men with the age of older than 50 years old and postmenopausal and women.
Based on the US Preventive Services Task Force (USPSTF) there are three groups of patients need to be screened for the osteoporosis:
- · Men with no history of osteoporosis
- · Women with the age of 65≤ year old, with no previous history of pathological fracture due to the osteoporosis
- · Women with the age of <65 years, with 10-year fracture risk of not less than a 65-year-old white woman (who has not any other risk factor)
Accordingly women older than age of 50 are the main target for the osteoporosis screening. There is no specific recommendation to screen men for the osteoporosis.
The USPSTF recommendations from 2002 included:
Meanwhile, there are two major modalities for the osteoporosis screening:
- · Dual energy x-ray absorptiometry (DXA) of the hip and lumbar spine bones
- · Quantitative ultrasonography of the calcaneus
*It should be noted of the two above mentioned modalities for screening the ultrasonograhy is preferred to the DXA due to its lower cost, lower ionizing radiation, more availability.
After the primary evaluation of the osteoporosis, the further evaluation are required in some cases such as:
· Women with normal bone density or mild osteopenia: T-score of greater than −1.50 – should have screening for 15 years.
· Women with moderate osteopenia: T-score of −1.50 to −1.99 – should have screening for 5 years.
· Women with advanced osteopenia: T-score of −2.00 to −2.49 - should have screening for 1 year.
Natural History
- In cases with untreated hip fractures the malunion and deformity of HIP joint can be occurred.
Complication
The type and frequency of complications of the hip fractures varies. The main complication of the hip fractures is the high risk of re-fracture due to their instability. In general the following are the most common complications of the hip fractures :
- Infection of the bone
- Infection of soft tissue
- Compartment syndrome
- Non-union of the fracture
- Mal-union
- Arm shortening
- Nerve Damage
- Vascular injury
- Vascular bleeding
- Re-fracture
- Decreased Motion
- Painful movement
Prognosis
Generally, the hip fractures carry an approximately 30% risk of mortality at 1 year also around 25% to 75% of adults may not reach their pre-fracture functional level. Most of the hip fractures heal well with no functional or gross problems in the appearance of the injured bone. But, proper immobilized and proper orthopedic follow-up are required due to the higher risk of re-fracture, complete fracture and displacement of the fracture. The followoing mentioned factores affect the patients mortality rate: comorbid disease, low pre-injury cognitive function, abnormal preoperative ECG, age >85 years, and decreased pre-fracture mobility.
History and Symptoms
The diagnosis of a hip fracture is based on: patient history, physical examination, and radiography.
The related signs and symptoms include:
- Deformity
- Skin lacerations
- Weak pulse
- Open fractures
- Bruising
- Swelling
- Stiffness
- Inability to move
- Pain in touch
- Loss of function of the leg
- Difficulties in detection of pulses
- An antalgic gait pattern
In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the leg. In MULTI-trauma patients or a tense compartment with neurological signs or stretch pain should be considered as the compartment syndrome, and the compartment pressures should be measured and monitored.
Physical Examination[35]
The related signs and symptoms include:
- Inability to move
- Pain in hip or groin
- Inability to put weight on the involved leg
- Stiffness in and around injured hip area
- bruising in and around injured hip area
- swelling in and around injured hip area
- Shorter leg on the side of injured hip
- Edema around injured hip area
- Most of the time the edema will be a non-pitting edema
- Depends on the edema extent, it may even lead to compartment syndrome in the anterior and internal compartment of leg
- Bruising
- As a manifestation of internal injury to the local vessels by trauma or fractures bone
- Decrease in range of motion
- Movement of the fractures limb will be painful if possible at all
- Tenderness
- Deformity
- Fractured bone deformity may be touchable in the internal side of the leg if the fracture is displaced
Physical examination of patients with hip fractures is usually remarkable for swelling, tenderness, bruises, ecchymosis, deformity and restricted range of motion of the leg.
Appearance of the Patient
- Patients with hip fractures usually appears normal unless the patients had a high energy trauma causing the open wound fracture.
Vital Signs
- Weak pulse may be seen when associated with polytrauma.
- Low blood pressure with normal pulse pressure may be present due to compound fracture with blood loss.
Skin
- Skin examination of patients with hip fractures includes:
HEENT
- HEENT examination of patients withhip fractures is usually normal.
Neck
- Neck examination of patients with hip fractures is normal.
Lungs
- Pulmonary examination of patients with hip fractures is usually normal.
Heart
- Cardiovascular examination of patients with hip fractures is usually normal.
Abdomen
- Abdominal examination of patients with hip fractures is usually normal.
Back
- Back examination of patients with hip fractures is usually normal.
Genitourinary
- Genitourinary examination of patients with hip fractures is usually normal.
Neuromuscular
- Neuromuscular examination of patients with hip fractures is usually normal.
- However, some patients may develop neuropraxia of the branch of the Ulnar nerve resulting in decreased sensation of fingers.
Laboratory Findings[36]
There is a limited laboratory tests useful in the diagnosis of bone fractures such as hip fractures Meanwhile, aged men and women may have some abnormalities in their laboratory findings suggestive of osteoporosis.
- Laboratory tests for the diagnosis of osteoporosis are:
- Complete blood count (CBC)
- Serum total calcium level
- Serum Ionized calcium level
- Serum phosphate level
- Serum alkaline phosphatase level
- Serum 25-(OH)-vitamin D level
The orthopedic surgeon should consider to have at least two radiographic projections (ie, anteroposterior [AP] and lateral) of the hip. These show the fracture, the extent of displacement, and the extent of comminution. The orthopedic surgeon should pay serious attention toward finding any foreign bodies in open fractures and gunshot injuries. Also imperative is to include the hip joint in the radiographs of hip fractures to ensure that the distal radioulnar joint injuries are not missed
A tuberosity view is helpfull ascertain the rotational displacement of the fracture. Also, it would be helpful for the orthopedic surgeon in planning how much supination or pronation is needed to achieve accurate anatomic reduction. The ulna is laid flat on the cassette with its subcutaneous border in contact with the cassette; the x-ray tube is tilted toward the olecranon by 20°. This radiograph is then compared with a standard set of diagrams that show the prominence of the radial tuberosity in various degrees of pronation and supination in order to determine the scope of the rotational deformity
-
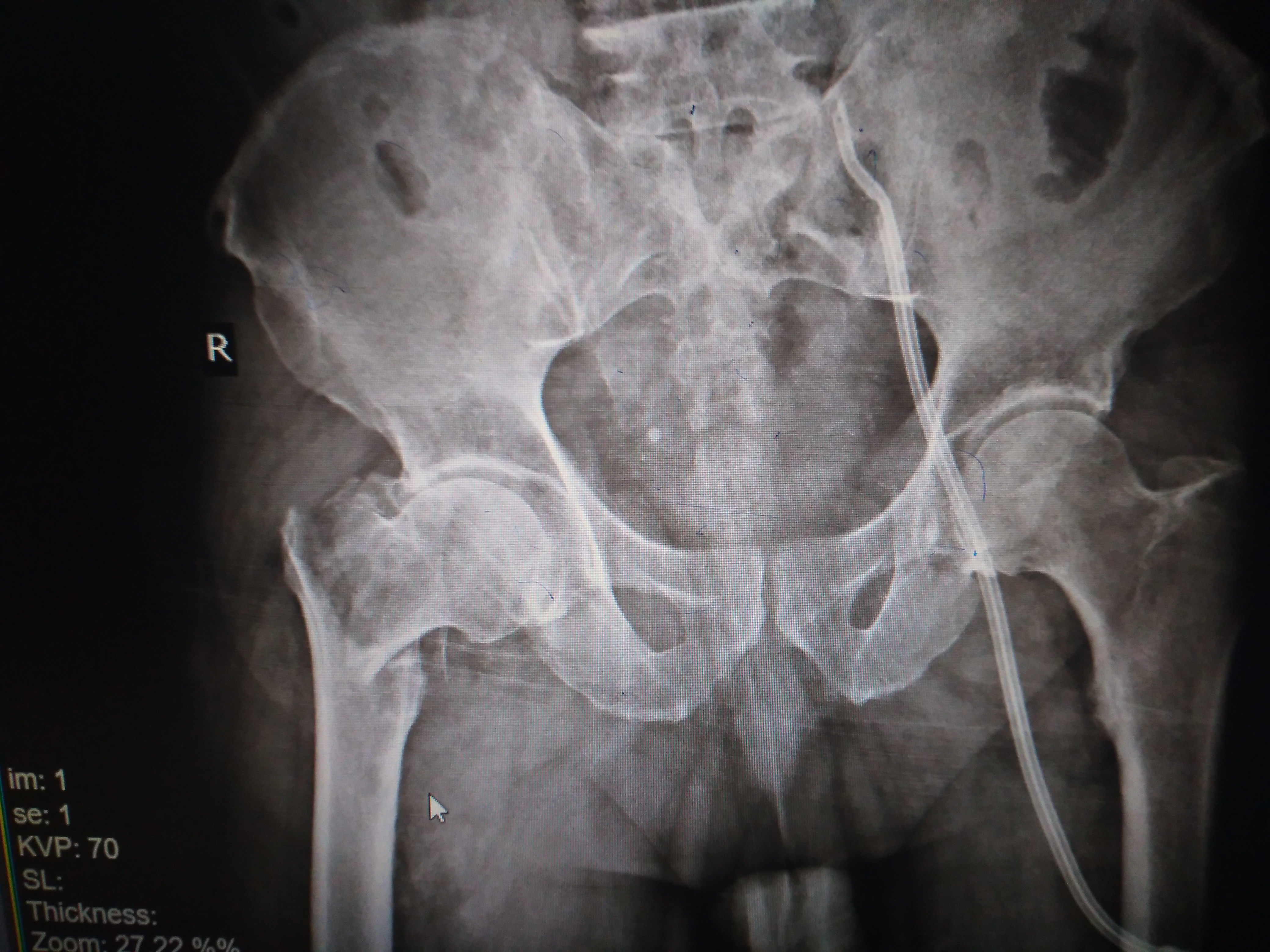
Fracture at the base of the right femoral neck.
-
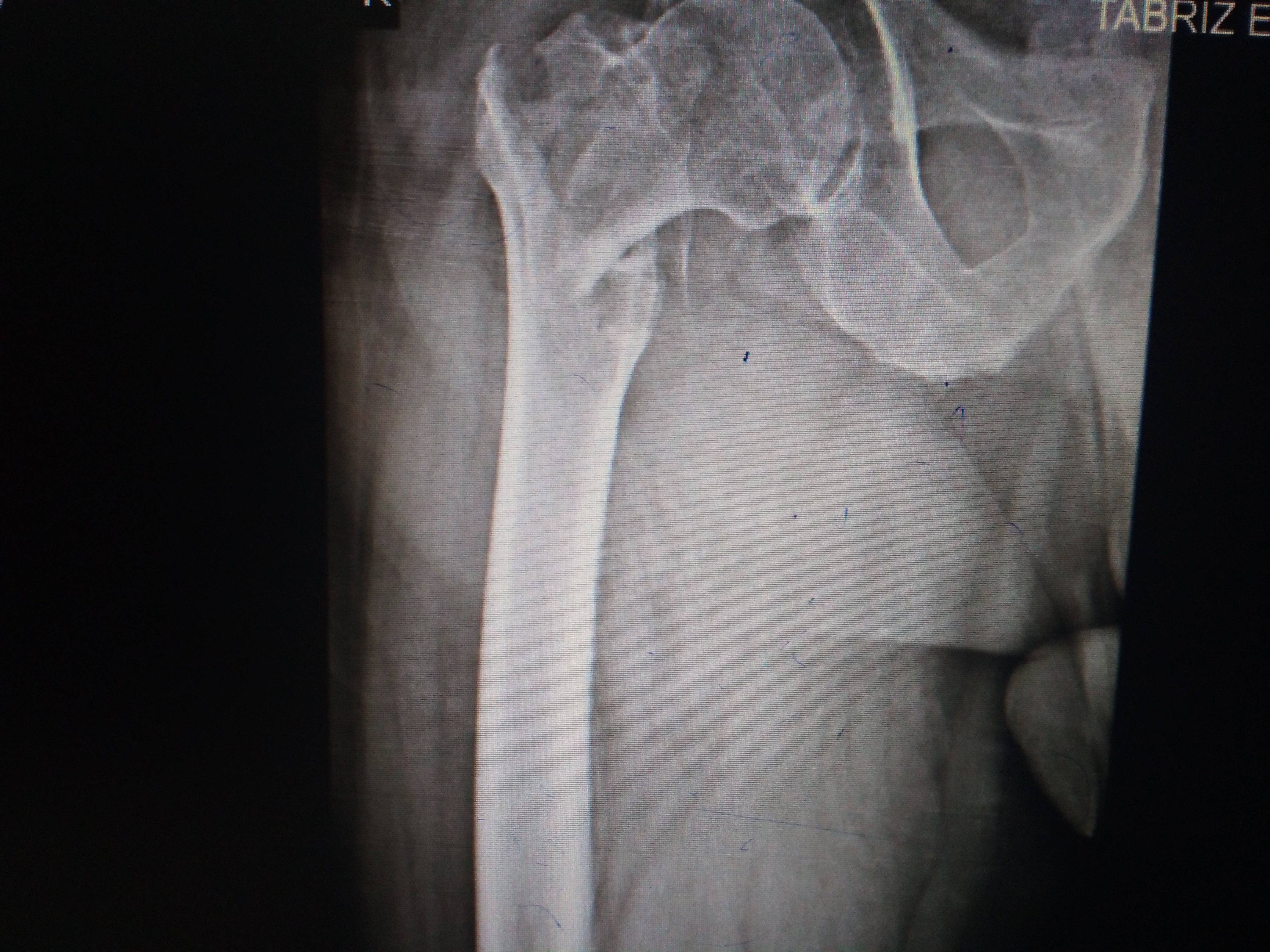
Fracture at the base of the right femoral neck.
-
Fracture at the base of the right femoral neck.
- CT-scan in the case of Hip fracture is the best modality if you can not have an exclusive diagnosis by X-ray itself can not be made.
- Its been reported that the articular fractures of the distal radius were statistically more likely to occur at the intervals between the ligament attachments than at the ligament attachments.
- The most common fracture sites were the center of the sigmoid notch, between the short and long radiolunate ligaments, and the central and ulnar aspects of the scaphoid fossa dorsally. These results suggest that CT may be used to identify the subsequent propagation of the fracture and the likely site of the impaction of the carpus on the distal radius articular surface.
-
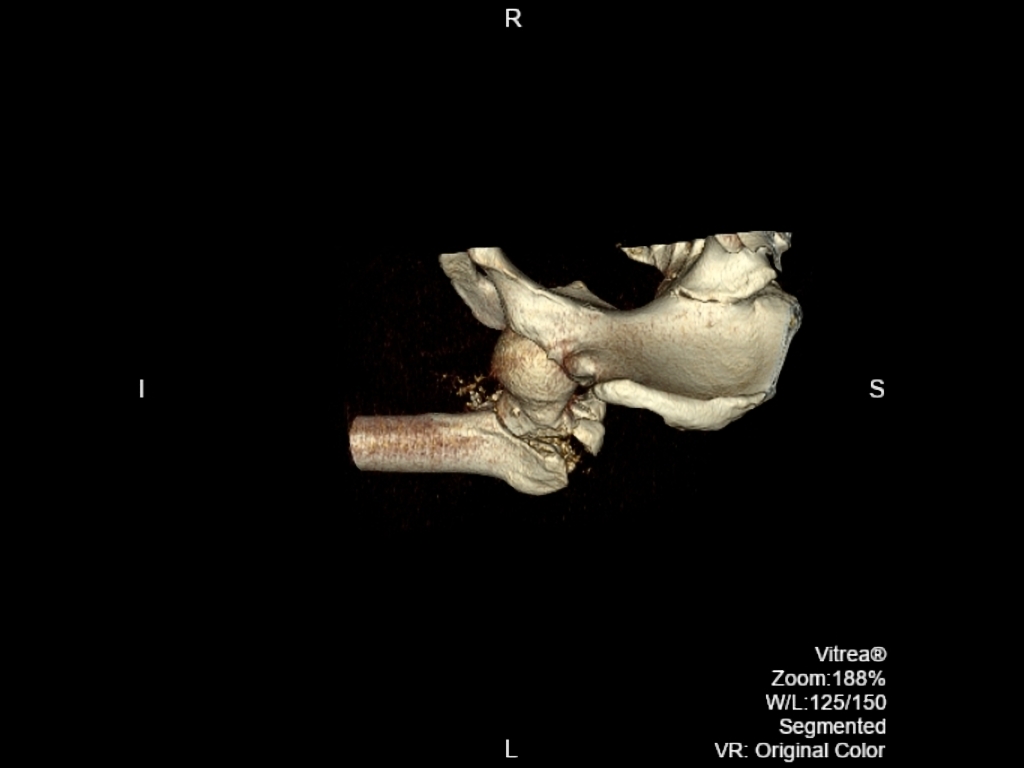
Fracture-dislocation of hip. CT scan shows posterior dislocation of femoral head associated with fracture of both anterior and posterior columns of acetabulum.
-
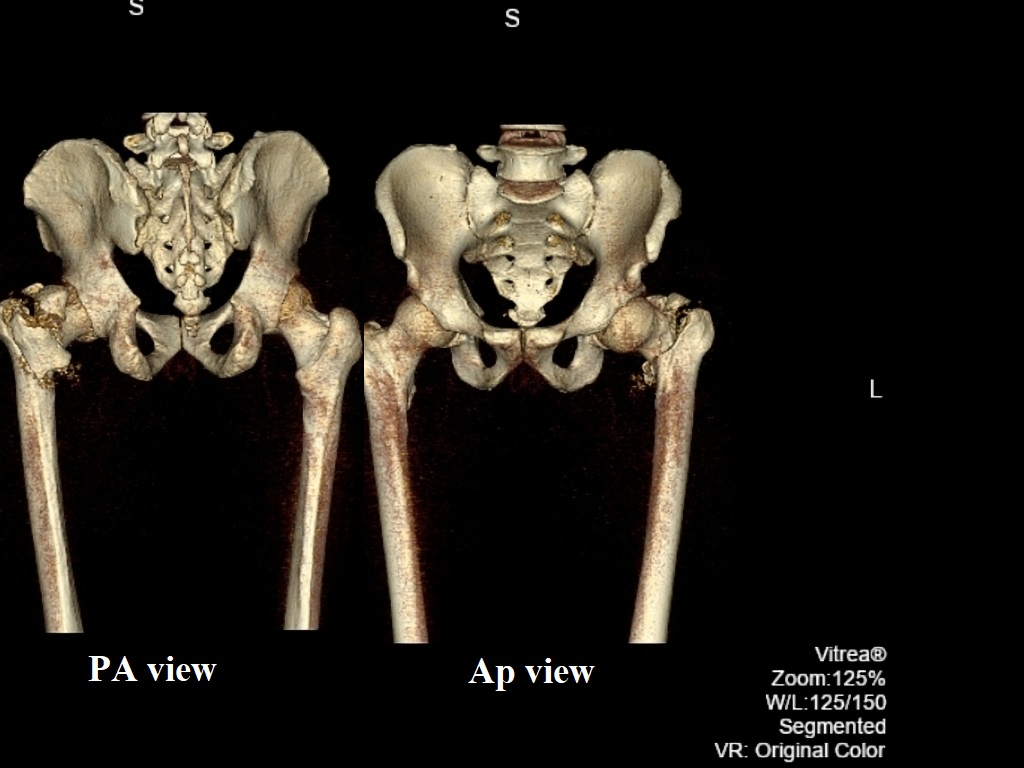
Coronal non-contrast. Comminuted intertrochanteric fracture involving the left proximal femur with internal rotation the femur following a road traffic accident.
-
Axial non-contrast. Comminuted intertrochanteric fracture involving the left proximal femur with internal rotation the femur following a road traffic accident.
-
Sagittal non-contrast. Comminuted intertrochanteric fracture involving the left proximal femur with internal rotation the femur following a road traffic accident.
-
3D. Comminuted intertrochanteric fracture involving the left proximal femur with internal rotation the femur following a road traffic accident.
-
Coronal non-contrast. Comminuted intertrochanteric fracture involving the left proximal femur with internal rotation the femur following a road traffic accident.
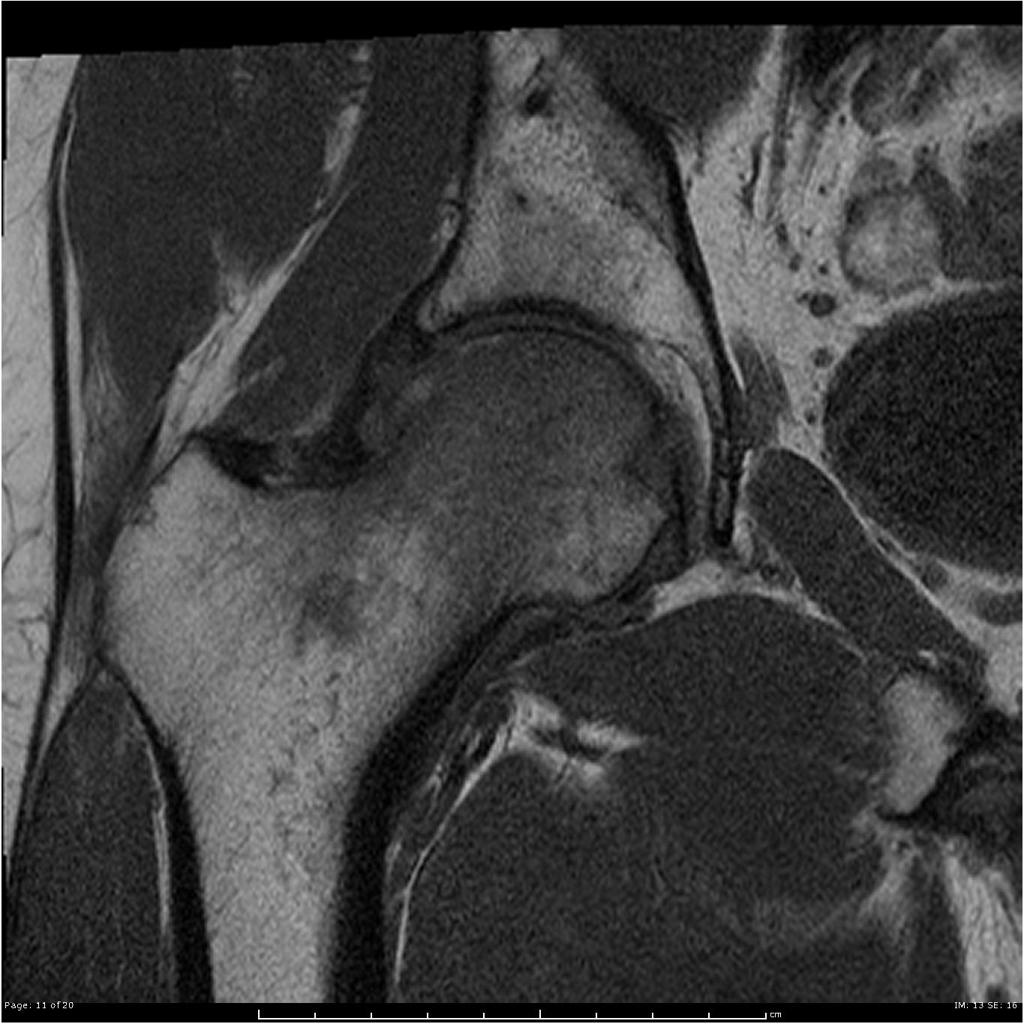
Magnetic resonance imaging (MRI) is an expensive technique that should not be used routinely. MRI is a powerful diagnostic tool to assess the abnormalities of the bone, ligaments and soft tissues associated with the Hip fractures, but it is known as a limited utility in radioulnar injuries and is not indicated in uncomplicated hip fractures. Meanwhile, the MRI can be useful in in following mentioned evaluations: Evaluation of occult fractures Evaluation of the post-traumatic or avascular necrosis of bones Evaluation of tendons Evaluation of nerve Evaluation of carpal tunnel syndrome
-
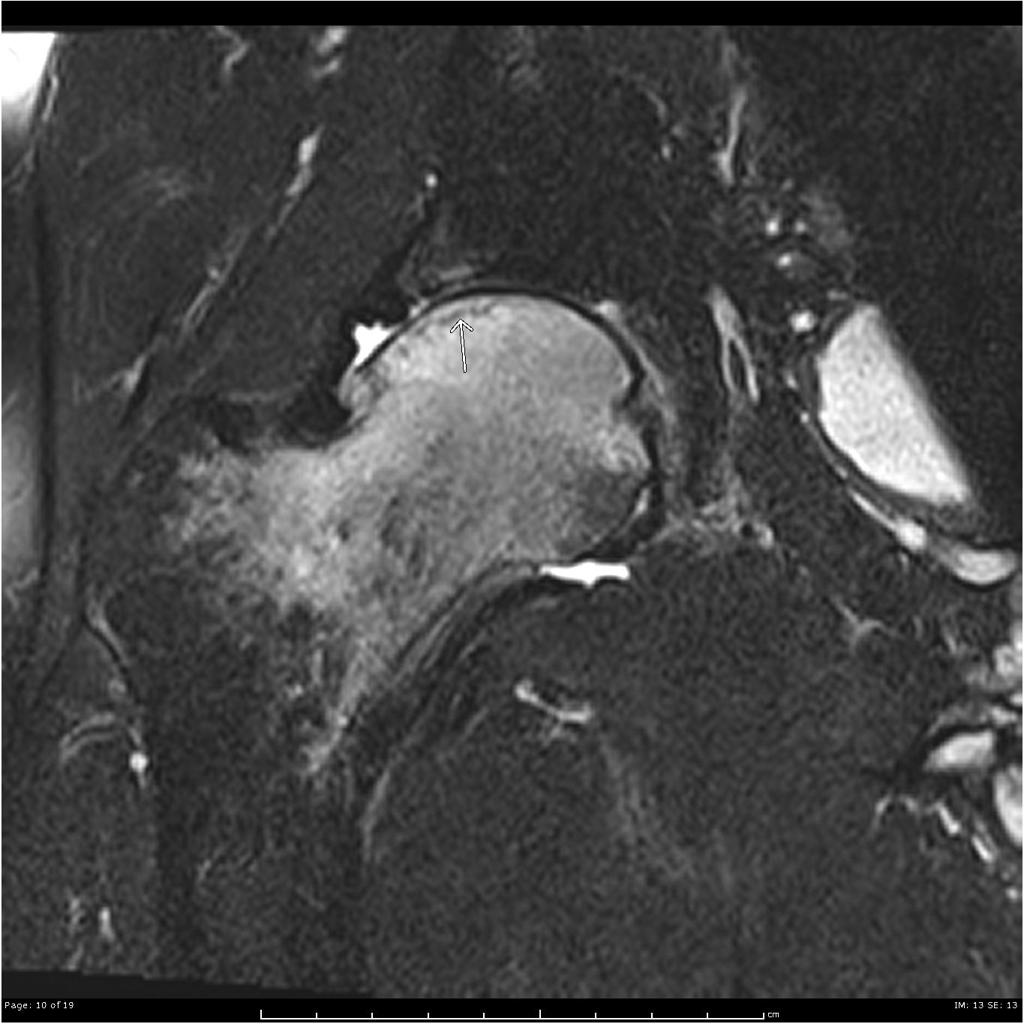
Coronal T1 Extensive marrow edema within the femoral head and neck. There is a subchondral fracture within the femoral head.
-
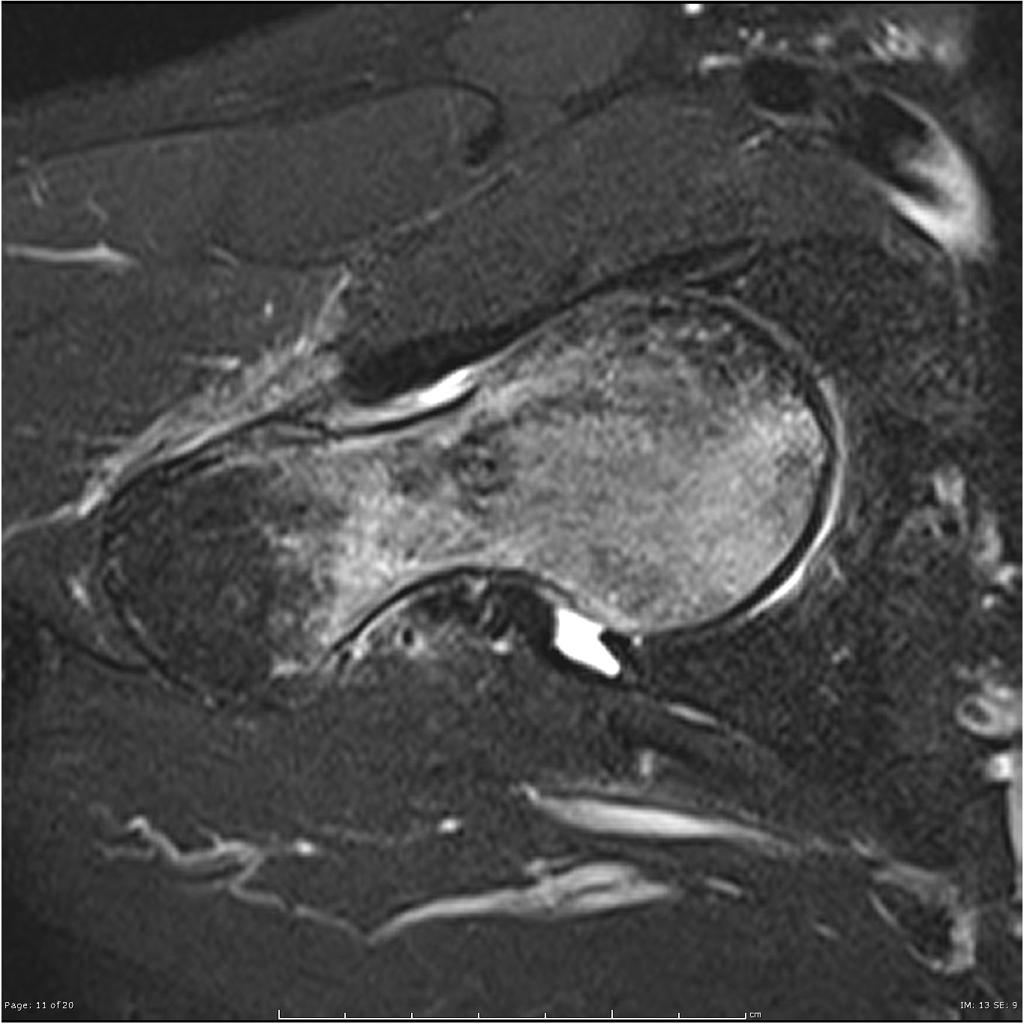
Coronal T2 fat sat Extensive marrow edema within the femoral head and neck. There is a subchondral fracture within the femoral head.
-
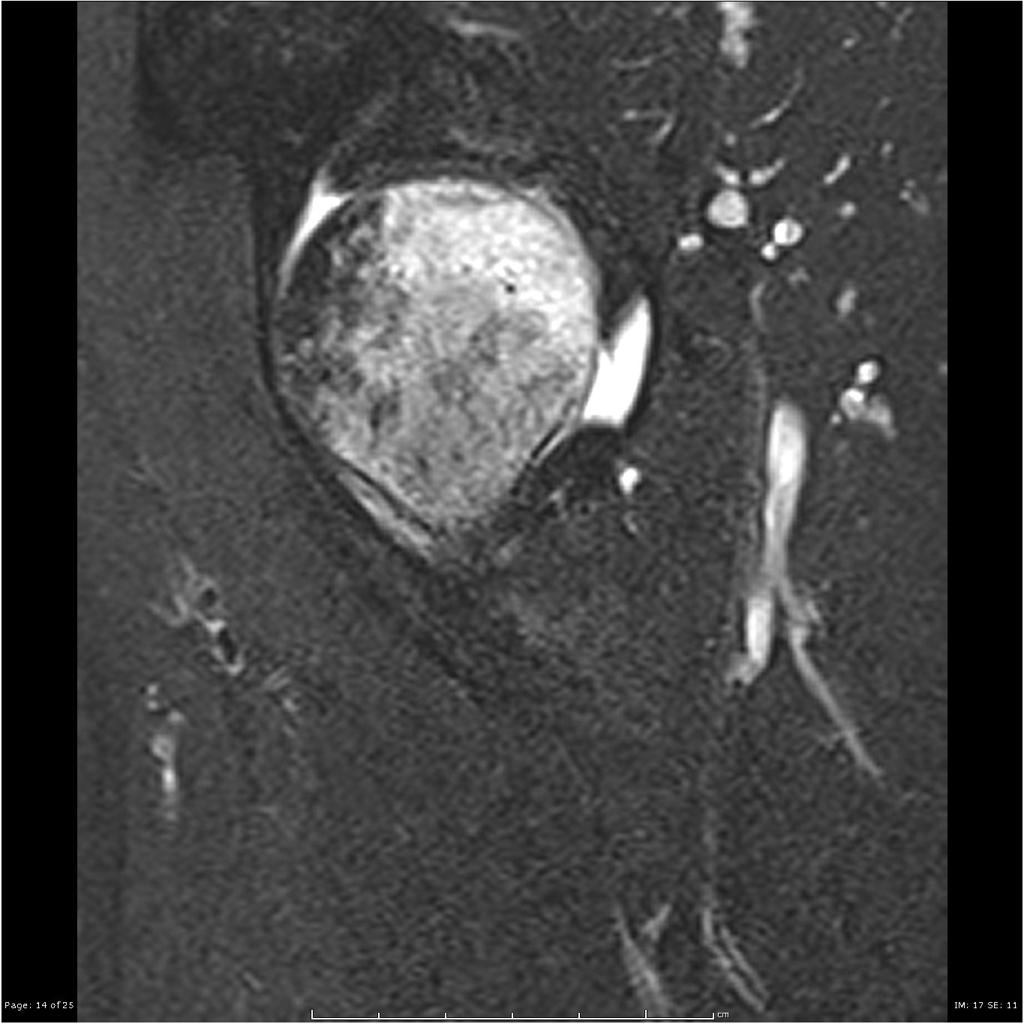
Coronal Axial T2 fat sat Extensive marrow edema within the femoral head and neck. There is a subchondral fracture within the femoral head.
-
Coronal Sagittal T2 fat sat Extensive marrow edema within the femoral head and neck. There is a subchondral fracture within the femoral head.
Other Imaging Finding[35]s
There are no other imaging findings associated with Hip fracture.
Other Diagnostic Studies[35]
There are no other imaging findings associated with Hip fracture.
The first step in managing a patient with a fracture is to stabilize the patient if he/she is unstable due to blood loss, etc by giving them intravenous fluids and giving them some painkillers if the pain is severe. If only one bone is broken, using cast or brace might be a possible treatment option. The hip fracture management is usually a combination of surgery and rehabilitation. It also depends on the location of the fracture and whether that fracture is displaced. Specific types of hip fractures can be considered stable enough to be managed with nonsurgical treatment.
- The first step in managing a patient with a fracture is to stabilize the patient if he/she is unstable due to blood loss, etc by giving them intravenous fluids and giving them some painkillers if the pain is severe.
- In children, the usual plan is to attempt closed reduction followed by cast immobilization. In adults, treatment with immobilization in a molded long arm cast can be used in those rare occasions of a non-displaced fracture of the leg bone. If the fracture shifts in position, it may require surgery to put the bones back together.
- Rigid immobilization is suggested in preference to removable splints in nonoperative treatment for the management of Hip bone fractures.
- For all patients with Hip fractures, a post-reduction true lateral radiograph is suggested .
- Patients probably do not need to begin early leg motion routinely after stable fracture fixation.
- Adjuvant treatment of Hip fractures with vitamin C is suggested for the prevention of disproportionate pain.
- If operative treatment is refused or the risks of surgery are considered to be too high the main emphasis of treatment is on pain relief. Skeletal traction may be considered for long term treatment.
-
Shortened left leg due to displacement of the femoral head superiorly and severe degenerative changes of the hip joint. The femoral head and neck have lost their normal anatomical configuration and morphology due to callus formation. Left greater trochanter is several centimeters higher when compared to the contralateral side.
Complications of Non-surgical therapy
Failure of non-surgical therapy is common:
- Re-displacement to its original position even in a cast
- Stiffness
- Post traumatic osteoarthritis leading to hip pain and loss of function
- Other risks specific to cast treatment include:
- Compression of the swollen leg causing compartment syndrome
- Reflex sympathetic dystrophy is a serious complication
- Stiffness is universal following a prolonged period of immobilization and swelling
- DVT/pulmonary embolism
- Pressure sores and
- Treatment of Hip fractures is important. Important complications such as avascular necrosis and non-union are very common without surgical intervention. The treatment options include non-operative management, internal fixation or prosthetic replacement.
- There are a variety of methods and implants useful to stabilize the Hip bone fracture, ranging from closed reduction and percutaneous pin fixation to the use of intra-medullary devices.
- However, the most common fixation methods to treat complex Hip fracture include external fixation, and open reduction and internal fixation.
| Intracapsular Fracture | Aim: fixing the cartilage on the head of the injured or displaced femur.
Associated with the socket, or acetabulum injuries. Fix the fracture with percutaneous pinning or a single larger screw |
Using an individual screws
Using a single compression hip screw Hemiarthroplasty A total hip replacement replaces Kocher-Langenbeck approach: Ideal choice of treatment used for an isolated fracture of the posterior wall and/or column with or without dislocation. |
|
| Intertrochanteric Fracture | Fix the fracture with either a compression hip screw or an intramedullary nail | Compression hip screw (sliding hip screw):
A compression hip screw device consists of: a screw, pin, or nail. This screw system inserted into a premade drill hole within the femoral neck and head with an angled side plate placed on the distal end of the screw and fixed with screws to the proximal femoral shaft. Cephalomedullary fixation: Is a treatment alternative for this type of fractures. Multiple solid nails with thin-diameter placed in a retrograde fashion through patients knee. Medial displacement osteotomy: This method has been employed for unstable intertrochanteric fractures prior to the main fixation but nowadays it is not indicated by orthopedics. Arthroplasty |
|
| Subtrochanteric Fracture | Fix the fracture with:
a long intramedullary nail with a large lag screw screws that capture the neck and head of the femur |
External fixation:
is rarely used method but it is indicated in severe open hip fractures. Open reduction with plates and screws: Intramedullary fixation: Is a treatment alternative for this type of fractures. Consisted of: a) centromedullary nail (placed within the medullary canal) b) cephalomedullary (placed to the femoral neck and head) |
-
A minimally displaced periprosthetic fracture is visible around the lateral aspect of the stem of the prosthesis, corresponding to a Vancouver B1 fracture (see key image). Porotic bone structure. Incidentally an inhomogenous calcified mass is visible in the pelvis.
-
Vancouver type B2 periprosthetic femur fracture of the right hip.
-
The right hip hemiarthroplasty is normally aligned and uncomplicated. There is a segment (approx 10cm) of disconnected surgical drain tubing in the lateral soft tissues of the left hip. Mild left hip osteoarthritis.
External Fixation With or Without Percutaneous Pin Fixation
- Spanning external fixation employs ligamentotaxis to restore and maintain length, alignment, and rotation of bone.
- Reduction is typically obtained through closed or minimally open methods and preserves the fracture biology.
- The addition of percutaneous pins enhances the ability to reduce and stabilize fracture fragments.
Complications of External Fixation
- Pin tract infection
- Injury to the superficial branch of the nerve
- Complex regional pain syndrome
Open reduction and internal fixation with plates and screws
- This is the most common type of surgical repair for Hip Fracture
- During this type of procedure, the bone fragments are first repositioned (reduced) into their normal alignment.
- The bones held together with special screws and metal plates attached to the outer surface of the bone.
Complications of open reduction and internal fixation with plates and screws
- Infection
- Damage to nerves and blood vessels
- Synostosis
- Nonunion
Pain Management[46]
Pain after an injury or surgery is a natural part of the healing process.
Medications are often prescribed for short-term pain relief after surgery or an injurysuch as:
- opioids
- non-steroidal anti-inflammatory drugs (NSAIDs)
- local anesthetics
Be aware that although opioids help relieve pain after surgery or an injury, they are a narcotic and can be addictive. It is important to use opioids only as directed by doctor.
The following options can be helpful for patients to rehabilitate after their fracture :
- Joints mobilization
- compression bandage
- Soft tissue massage
- Exercises and Activity modification
- Complex Hip fracture warrant individualized immobilization and rehabilitation strategies.
- Because some Hip bone fractures are the result of high-energy injuries, a prolonged period of leg immobilization and soft-tissue rest may be beneficial and has not been shown to affect clinical outcomes.
- The hip is typically immobilized for 2 weeks post-operatively in a sugar tong splint with neutral leg rotation.
- Full weight bearing exercises at approximately 3 months post-operatively
- The presence of varying degrees of Hip area stiffness is inevitable and may result from poor pain control, lack of effort in controlled mobilization, edema, concomitant ipsilateral upper extremity fractures, or peripheral nerve injuries.
- Internal rotation from hip flexion
- Avoiding the impact activities for six weeks postoperative
- unloaded or partially loaded mobilize postoperatively crucial to the joint with active and passive range of motion (ROM) based on the surgical procedure
- Avoiding straight leg raise for 4 weeks postoperatively
- Cardiovascular training is important
- Hip flexion greater than 70–90°
- External rotation of the leg
- Adduction of the leg past midline
- Should not bend forward from the waist more than 90
- Early stretching and mobilization of the intrinsic and extrinsic tendons of the hand is important to prevent finger stiffness.
- Edema control can be initiated with compression gloves, digital massage, and active and passive ROM of the leg.
- A home exercise program or outpatient occupational therapy is started immediately post-operatively to maintain full range of motion of the leg and limit the development of intrinsic muscle tightness
There are various preventive options to reduce the incidence of the Hip bone fracture-dislocation
- Using suitable hip joint guards during practicing sports (skating, biking) and/or driving motorbikes
- Avoid falls in elderly individuals
- Prevention and/or treatment of osteoporosis
- Healthy diet
It should be noted that the Post-menopausal women specially older than the age of 65 are at the higher risk of osteoporosis consequently these type of patients at greater risk for the pathological fractures .
So the Calcium and vitamin D supplementation play important role in increasing the bone mineral density (BMD) consequently decrease the risk of fracture in these type of patients. Also, avoiding excessive alcohol and quitting smoking play important role in this regard.
Detecting osteoporosis[22]
- DEXA(dual-energy x-ray absorptiometry) scan
- Serum calcium and vitamin D levels
- Ultrasonography of the calcaneus
- The primary goal for the treatment of osteoporosis is to reduce longtime fracture risk in patients. Increasing bone mineral density (BMD) in response to the treatment is far less important than improvement of clinical aspects of osteoporosis, i.e., osteoporotic fracture. Therefore, most of the drugs efficacy is measured by the extent they improve the fracture risk instead of increasing BMD.
- During the treatment, if a single fracture happens, it does not necessarily indicate treatment failure or the need to be started on an alternative treatment or patient referral to a specialist.
- Calcium and vitamin D supplementation have been found to be effective in reducing the long term fracture risk, significantly. In order to suggest the people to use vitamin D and calcium supplements, the physician needs to make sure that patient is not able to obtain the nutrients through the daily intake. The available supplemental ions of calcium include calcium carbonate, calcium citrate, and vitamin D3 in various dosage forms.
- Exercise: Exercise promotes the mineralization of bone and bone accumulation particularly during growth. High impact exercise, in particular, has been shown to prevent the development of osteoporosis. However, it can have a negative effect on bone mineralization in cases of poor nutrition, such as anorexia nervosa and celiac disease.
- Nutrition: A diet high in calcium and vitamin D prevents bone loss. Patients at risk for osteoporosis, such as persons with chronic steroid use are generally treated with vitamin D and calcium supplementation. In renal disease, more active forms of vitamin D, such as 1,25-dihydroxycholecalciferol or calcitriol are used; as the kidney cannot adequately generate calcitriol from calcidiol (25-hydroxycholecalciferol), which is the storage form of vitamin D.
- By quitting smoking, osteoporosis as well as other diseases can be prevented.
- Avoiding excessive alcohol intake or drinking only in moderation (1–2 alcoholic beverages/day).
- Taking least possible dosages of certain medications that are associated with osteoporosis (anticonvulsants or corticosteroids).
See also
- Hip fracture treatment
- Pipkin classification
- Garden classification
- Pauwel's classification
- Evans-Jensen classification
- Seinsheimer classification
- AAOS classification of periprosthetic hip fracture
- Cooke and Newman classification
- Johansson classification
- Vancouver classification
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Collin PG, D'Antoni AV, Loukas M, Oskouian RJ, Tubbs RS (January 2017). "Hip fractures in the elderly-: A Clinical Anatomy Review". Clin Anat. 30 (1): 89–97. doi:10.1002/ca.22779. PMID 27576301.
- ↑ Rocos B, Whitehouse MR, Kelly MB (May 2017). "Resuscitation in hip fractures: a systematic review". BMJ Open. 7 (4): e015906. doi:10.1136/bmjopen-2017-015906. PMC 5623376. PMID 28473523.
- ↑ 3.0 3.1 3.2 3.3 Bhandari M, Swiontkowski M (November 2017). "Management of Acute Hip Fracture". N. Engl. J. Med. 377 (21): 2053–2062. doi:10.1056/NEJMcp1611090. PMID 29166235.
- ↑ 4.0 4.1 4.2 Malafarina V, Reginster JY, Cabrerizo S, Bruyère O, Kanis JA, Martinez JA, Zulet MA (April 2018). "Nutritional Status and Nutritional Treatment Are Related to Outcomes and Mortality in Older Adults with Hip Fracture". Nutrients. 10 (5). doi:10.3390/nu10050555. PMC 5986435. PMID 29710860.
- ↑ 5.0 5.1 Guerado E, Cruz E, Cano JR, Crespo PV, Alaminos M, Sánchez-Quevedo Mdel C, Campos A (January 2016). "Bone mineral density aspects in the femoral neck of hip fracture patients". Injury. 47 Suppl 1: S21–4. doi:10.1016/S0020-1383(16)30005-5. PMID 26768284.
- ↑ Parker M, Johansen A (July 2006). "Hip fracture". BMJ. 333 (7557): 27–30. doi:10.1136/bmj.333.7557.27. PMC 1488757. PMID 16809710.
- ↑ 7.0 7.1 Della Rocca GJ, Crist BD (April 2013). "Hip fracture protocols: what have we changed?". Orthop. Clin. North Am. 44 (2): 163–82. doi:10.1016/j.ocl.2013.01.009. PMID 23544822.
- ↑ 8.0 8.1 8.2 8.3 Magaziner J, Chiles N, Orwig D (2015). "Recovery after Hip Fracture: Interventions and Their Timing to Address Deficits and Desired Outcomes--Evidence from the Baltimore Hip Studies". Nestle Nutr Inst Workshop Ser. 83: 71–81. doi:10.1159/000382064. PMC 5494960. PMID 26484873.
- ↑ Coomber R, Alshameeri Z, Masia AF, Mela F, Parker MJ (December 2017). "Hip fractures and Parkinson's disease: A case series". Injury. 48 (12): 2730–2735. doi:10.1016/j.injury.2017.08.042. PMID 28985911.
- ↑ Braithwaite RS, Col NF, Wong JB (March 2003). "Estimating hip fracture morbidity, mortality and costs". J Am Geriatr Soc. 51 (3): 364–70. PMID 12588580.
- ↑ 11.0 11.1 Xiao Z, Ren D, Feng W, Chen Y, Kan W, Xing D (2016). "Height and Risk of Hip Fracture: A Meta-Analysis of Prospective Cohort Studies". Biomed Res Int. 2016: 2480693. doi:10.1155/2016/2480693. PMC 5080474. PMID 27818998.
- ↑ 12.0 12.1 Hall AJ, Lang IA, Endacott R, Hall A, Goodwin VA (December 2017). "Physiotherapy interventions for people with dementia and a hip fracture-a scoping review of the literature". Physiotherapy. 103 (4): 361–368. doi:10.1016/j.physio.2017.01.001. PMID 28843451.
- ↑ 13.0 13.1 Sheehan KJ, Sobolev B, Guy P (October 2017). "Mortality by Timing of Hip Fracture Surgery: Factors and Relationships at Play". J Bone Joint Surg Am. 99 (20): e106. doi:10.2106/JBJS.17.00069. PMID 29040134.
- ↑ 14.0 14.1 14.2 14.3 Rogmark C, Kristensen MT, Viberg B, Rönnquist SS, Overgaard S, Palm H (August 2018). "Hip fractures in the non-elderly-Who, why and whither?". Injury. 49 (8): 1445–1450. doi:10.1016/j.injury.2018.06.028. PMID 29983171.
- ↑ 15.0 15.1 Sheehan KJ, Sobolev B, Villán Villán YF, Guy P (August 2017). "Patient and system factors of time to surgery after hip fracture: a scoping review". BMJ Open. 7 (8): e016939. doi:10.1136/bmjopen-2017-016939. PMC 5724192. PMID 28827264.
- ↑ Johansen A, Golding D, Brent L, Close J, Gjertsen JE, Holt G, Hommel A, Pedersen AB, Röck ND, Thorngren KG (October 2017). "Using national hip fracture registries and audit databases to develop an international perspective". Injury. 48 (10): 2174–2179. doi:10.1016/j.injury.2017.08.001. PMID 28803651.
- ↑ Veronese N, Maggi S (August 2018). "Epidemiology and social costs of hip fracture". Injury. 49 (8): 1458–1460. doi:10.1016/j.injury.2018.04.015. PMID 29699731.
- ↑ Kannus P, Parkkari J, Sievänen H, Heinonen A, Vuori I, Järvinen M (January 1996). "Epidemiology of hip fractures". Bone. 18 (1 Suppl): 57S–63S. PMID 8717549.
- ↑ Osaki M (April 2015). "[Hip Fracture--Epidemiology, Management and Liaison Service. Rehabilitation for the hip fracture]". Clin Calcium (in Japanese). 25 (4): 577–84. doi:CliCa1504577584 Check
|doi=value (help). PMID 25814019. - ↑ Johnell O, Kanis J (March 2005). "Epidemiology of osteoporotic fractures". Osteoporos Int. 16 Suppl 2: S3–7. doi:10.1007/s00198-004-1702-6. PMID 15365697.
- ↑ Chang W, Lv H, Feng C, Yuwen P, Wei N, Chen W, Zhang Y (April 2018). "Preventable risk factors of mortality after hip fracture surgery: Systematic review and meta-analysis". Int J Surg. 52: 320–328. doi:10.1016/j.ijsu.2018.02.061. PMID 29530826.
- ↑ 22.0 22.1 Sheehan KJ, Sobolev B, Chudyk A, Stephens T, Guy P (April 2016). "Patient and system factors of mortality after hip fracture: a scoping review". BMC Musculoskelet Disord. 17: 166. doi:10.1186/s12891-016-1018-7. PMC 4832537. PMID 27079195.
- ↑ 23.0 23.1 23.2 Santesso N, Carrasco-Labra A, Brignardello-Petersen R (March 2014). "Hip protectors for preventing hip fractures in older people". Cochrane Database Syst Rev (3): CD001255. doi:10.1002/14651858.CD001255.pub5. PMID 24687239.
- ↑ Yuan ZC, Mo H, Guan J, He JL, Wu ZJ (September 2016). "Risk of hip fracture following stroke, a meta-analysis of 13 cohort studies". Osteoporos Int. 27 (9): 2673–2679. doi:10.1007/s00198-016-3603-x. PMID 27101998.
- ↑ 25.0 25.1 Basu N, Natour M, Mounasamy V, Kates SL (October 2016). "Geriatric hip fracture management: keys to providing a successful program". Eur J Trauma Emerg Surg. 42 (5): 565–569. doi:10.1007/s00068-016-0685-2. PMID 27241865.
- ↑ 26.0 26.1 Ferrari S, Reginster JY, Brandi ML, Kanis JA, Devogelaer JP, Kaufman JM, Féron JM, Kurth A, Rizzoli R (December 2016). "Unmet needs and current and future approaches for osteoporotic patients at high risk of hip fracture". Arch Osteoporos. 11 (1): 37. doi:10.1007/s11657-016-0292-1. PMC 5306171. PMID 27800591.
- ↑ Sheehan SE, Shyu JY, Weaver MJ, Sodickson AD, Khurana B (2015). "Proximal Femoral Fractures: What the Orthopedic Surgeon Wants to Know". Radiographics. 35 (5): 1563–84. doi:10.1148/rg.2015140301. PMID 26186669.
- ↑ Altizer L (2005). "Hip fractures". Orthop Nurs. 24 (4): 283–92, quiz 293–4. PMID 16056174.
- ↑ 29.0 29.1 Su EP, Su SL (November 2014). "Femoral neck fractures: a changing paradigm". Bone Joint J. 96-B (11 Supple A): 43–7. doi:10.1302/0301-620X.96B11.34334. PMID 25381407.
- ↑ Kazley JM, Banerjee S, Abousayed MM, Rosenbaum AJ (February 2018). "Classifications in Brief: Garden Classification of Femoral Neck Fractures". Clin. Orthop. Relat. Res. 476 (2): 441–445. doi:10.1007/s11999.0000000000000066. PMC 6259691. PMID 29389800.
- ↑ 31.0 31.1 Wendt K, Heim D, Josten C, Kdolsky R, Oestern HJ, Palm H, Sintenie JB, Komadina R, Copuroglu C (August 2016). "Recommendations on hip fractures". Eur J Trauma Emerg Surg. 42 (4): 425–431. doi:10.1007/s00068-016-0684-3. PMC 4969356. PMID 27418204.
- ↑ 32.0 32.1 32.2 Bian S, Hu J, Zhang K, Wang Y, Yu M, Ma J (January 2018). "Dairy product consumption and risk of hip fracture: a systematic review and meta-analysis". BMC Public Health. 18 (1): 165. doi:10.1186/s12889-018-5041-5. PMC 5778815. PMID 29357845.
- ↑ Lv QB, Gao X, Liu X, Shao ZX, Xu QH, Tang L, Chi YL, Wu AM (June 2017). "The serum 25-hydroxyvitamin D levels and hip fracture risk: a meta-analysis of prospective cohort studies". Oncotarget. 8 (24): 39849–39858. doi:10.18632/oncotarget.16337. PMC 5503658. PMID 28418890.
- ↑ Mundi S, Pindiprolu B, Simunovic N, Bhandari M (February 2014). "Similar mortality rates in hip fracture patients over the past 31 years". Acta Orthop. 85 (1): 54–9. doi:10.3109/17453674.2013.878831. PMC 3940992. PMID 24397744.
- ↑ 35.0 35.1 35.2 35.3 35.4 35.5 Zanker J, Duque G (August 2017). "Rapid Geriatric Assessment of Hip Fracture". Clin. Geriatr. Med. 33 (3): 369–382. doi:10.1016/j.cger.2017.03.003. PMID 28689569.
- ↑ Boddaert J, Raux M, Khiami F, Riou B (December 2014). "Perioperative management of elderly patients with hip fracture". Anesthesiology. 121 (6): 1336–41. doi:10.1097/ALN.0000000000000478. PMID 25299743.
- ↑ Sanal HT, Boulton C, Neyisci C, Erdem Y, Lowe J (April 2019). "Imaging of Pelvic and Femoral Fixation Hardware: Normal Findings and Hardware Failure". Semin Musculoskelet Radiol. 23 (2): e1–e19. doi:10.1055/s-0039-1681048. PMID 30925631.
- ↑ 38.0 38.1 Deshmukh S, Omar IM (April 2019). "Imaging of Hip Arthroplasties: Normal Findings and Hardware Complications". Semin Musculoskelet Radiol. 23 (2): 162–176. doi:10.1055/s-0038-1677467. PMID 30925629.
- ↑ Sucato DJ (July 2018). "Approach to the Hip for SCFE: The North American Perspective". J Pediatr Orthop. 38 Suppl 1: S5–S12. doi:10.1097/BPO.0000000000001183. PMID 29877938.
- ↑ 40.0 40.1 Foex BA, Russell A (October 2018). "BET 2: CT versus MRI for occult hip fractures". Emerg Med J. 35 (10): 645–647. doi:10.1136/emermed-2018-208093.3. PMID 30249714.
- ↑ Berkowitz JL, Potter HG (September 2017). "Advanced MRI Techniques for the Hip Joint: Focus on the Postoperative Hip". AJR Am J Roentgenol. 209 (3): 534–543. doi:10.2214/AJR.16.17789. PMC 5578463. PMID 28537800.
- ↑ 42.0 42.1 42.2 Roberts KC, Brox WT, Jevsevar DS, Sevarino K (February 2015). "Management of hip fractures in the elderly". J Am Acad Orthop Surg. 23 (2): 131–7. doi:10.5435/JAAOS-D-14-00432. PMID 25624365.
- ↑ 43.0 43.1 43.2 Fernandez MA, Griffin XL, Costa ML (September 2015). "Management of hip fracture". Br. Med. Bull. 115 (1): 165–72. doi:10.1093/bmb/ldv036. PMID 26311503.
- ↑ Donnelly K, Bracchi R, Hewitt J, Routledge PA, Carter B (2017). "Benzodiazepines, Z-drugs and the risk of hip fracture: A systematic review and meta-analysis". PLoS ONE. 12 (4): e0174730. doi:10.1371/journal.pone.0174730. PMC 5407557. PMID 28448593.
- ↑ Coomber R, Porteous M, Hubble M, Parker MJ (October 2016). "Total hip replacement for hip fracture: Surgical techniques and concepts". Injury. 47 (10): 2060–2064. doi:10.1016/j.injury.2016.06.034. PMID 27451289. Vancouver style error: initials (help)
- ↑ 46.0 46.1 46.2 Peeters CM, Visser E, Van de Ree CL, Gosens T, Den Oudsten BL, De Vries J (July 2016). "Quality of life after hip fracture in the elderly: A systematic literature review". Injury. 47 (7): 1369–82. doi:10.1016/j.injury.2016.04.018. PMID 27178770.
- ↑ 47.0 47.1 Lee SY, Yoon BH, Beom J, Ha YC, Lim JY (December 2017). "Effect of Lower-Limb Progressive Resistance Exercise After Hip Fracture Surgery: A Systematic Review and Meta-Analysis of Randomized Controlled Studies". J Am Med Dir Assoc. 18 (12): 1096.e19–1096.e26. doi:10.1016/j.jamda.2017.08.021. PMID 29033325.
- ↑ Riddell M, Ospina M, Holroyd-Leduc JM (July 2016). "Use of Femoral Nerve Blocks to Manage Hip Fracture Pain among Older Adults in the Emergency Department: A Systematic Review". CJEM. 18 (4): 245–52. doi:10.1017/cem.2015.94. PMID 26354332.
- ↑ Smith T, Pelpola K, Ball M, Ong A, Myint PK (July 2014). "Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis". Age Ageing. 43 (4): 464–71. doi:10.1093/ageing/afu065. PMID 24895018.
- ↑ 50.0 50.1 Dyer SM, Crotty M, Fairhall N, Magaziner J, Beaupre LA, Cameron ID, Sherrington C (September 2016). "A critical review of the long-term disability outcomes following hip fracture". BMC Geriatr. 16: 158. doi:10.1186/s12877-016-0332-0. PMC 5010762. PMID 27590604.
- ↑ 51.0 51.1 51.2 Salamon A, Toldy E, Biró C, Mátrai Á, Balassa T, Lőcsei Z (October 2017). "[Vitamin D and calcium supplementation in elderly patients with hip fracture]". Orv Hetil (in Hungarian). 158 (43): 1699–1707. doi:10.1556/650.2017.30857. PMID 29135297.
- ↑ Fabi DW (May 2016). "Multimodal Analgesia in the Hip Fracture Patient". J Orthop Trauma. 30 Suppl 1: S6–S11. doi:10.1097/BOT.0000000000000561. PMID 27101321.
- ↑ 53.0 53.1 Rasmussen B, Uhrenfeldt L (December 2016). "Establishing well-being after hip fracture: a systematic review and meta-synthesis". Disabil Rehabil. 38 (26): 2515–29. doi:10.3109/09638288.2016.1138552. PMID 26860402.
External links
- Orthopedics.com article on hip fractures
- American Academy of Orthopedic Surgeons article on hip fractures
- Fractures of the Femoral Neck Wheeless Textbook of Orthopaedics
- Intertrochanteric Fractures Wheeless' Textbook of Orthopaedics
- Proximal femoral fracture Musculoskeletal Radiology of Fractures
- Hip fractures
- http://www.wheelessonline.com/ortho/Hip_fracture
- https://orthoinfo.aaos.org/en/diseases--conditions/hip-fractures