Cysteamine (oral)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Turky Alkathery, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Cysteamine (oral) is a renal-urologic agent that is FDA approved for the treatment of nephropathic cystinosis in children and adults. Common adverse reactions include rash, abdominal pain, unpleasant breath smells, diarrhea, loss of appetite, nausea, vomiting, dizziness, headache, lethargy, and fever.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indication
- Cysteamine is indicated for the management of nephropathic cystinosis in children and adults.
Dosage
- New patients should be started on ¼ to 1/6 of the maintenance dose of Cysteamine. The dose should then be raised gradually over four to six weeks to avoid intolerance.
- If a dose is missed, it should be taken as soon as possible. If it is within two hours of the next dose, skip the missed dose and go back to the regular dosing schedule. Do not double dose.
- When Cysteamine is well tolerated, the goal of therapy is to keep leukocyte cystine levels below 1 nmol/½ cystine/mg protein five to six hours following administration of Cysteamine. Patients with poorer tolerability still receive significant benefit if white cell cystine levels are below 2 nmol/½ cystine/mg protein. The Cysteamine dose can be increased to a maximum of 1.95 grams/m2/day to achieve this level.
- The dose of 1.95 grams/m2/day has been associated with an increased rate of withdrawal from treatment due to intolerance and an increased incidence of adverse events.
- Cystinotic patients taking cysteamine hydrochloride or phosphocysteamine solutions may be transferred to equimolar doses of Cysteamine capsules.
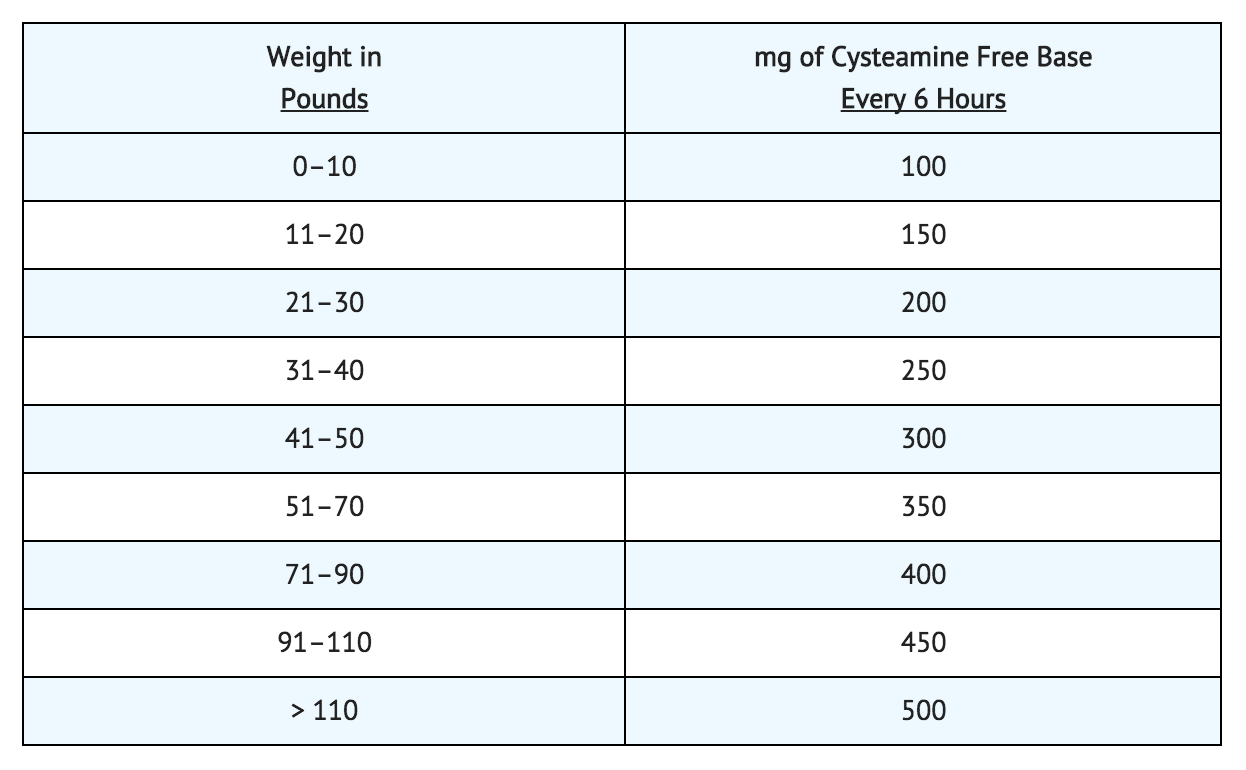
- The recommended maintenance dose of 1.30 grams/m2/day can be approximated by administering Cysteamine according to the following table, which takes surface area as well as weight into consideration.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
- There is limited information regarding Off-Label Guideline-Supported Use of Cysteamine in adult patients.
Non–Guideline-Supported Use
- There is limited information regarding Off-Label Non–Guideline-Supported Use of Cysteamine in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Indication
- Cysteamine is indicated for the management of nephropathic cystinosis in children.
Dosage
- The recommended Cysteamine maintenance dose for children up to age 12 years is 1.30 grams/m2/day of the free base, given in four divided doses. Intact Cysteamine capsules should not be administered to children under the age of approximately six years due to the risk of aspiration. Cysteamine capsules may be administered to children under the age of approximately six years by sprinkling the capsule contents over food. Patients over age 12 and over 110 pounds weight should receive 2.0 grams/day, divided four times daily.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
- There is limited information regarding Off-Label Guideline-Supported Use of Cysteamine in pediatric patients.
Non–Guideline-Supported Use
- There is limited information regarding Off-Label Non–Guideline-Supported Use of Cysteamine in pediatric patients.
Contraindications
- Cysteamine is contraindicated in patients who have developed hypersensitivity to it or to cysteamine or penicillamine.
Warnings
- If a skin rash develops, Cysteamine should be withheld until the rash clears. Cysteamine may be restarted at a lower dose under close supervision, then slowly titrated to the therapeutic dose. If a severe skin rash develops such as erythema multiforme bullosa or toxic epidermal necrolysis, Cysteamine should not be readministered.
- CNS symptoms such as seizures, lethargy, somnolence, depression, and encephalopathy have been associated with cysteamine. If CNS symptoms develop, the patient should be carefully evaluated and the dose adjusted as necessary. Neurological complications have been described in some cystinotic patients not on cysteamine treatment. This may be a manifestation of the primary disorder. Patients should not engage in hazardous activities until the effects of Cysteamine on mental performance are known.
- Gastrointestinal ulceration and bleeding have been reported in patients receiving cysteamine bitartrate. Physicians should remain alert for signs of ulceration and bleeding and should inform patients and/or guardians about the signs and symptoms of serious G.I. toxicity and what steps to take if they occur.
Precautions
General
- Gastrointestinal tract symptoms including nausea, vomiting, anorexia and abdominal pain have been associated with cysteamine, sometimes severe. In addition, gastrointestinal ulceration and bleeding have been reported in patients on cysteamine therapy. If these develop, therapy may have to be interrupted and the dose adjusted. A cysteamine dose of 1.95 grams/m2/day (approximately 80 to 90 mg/kg/day) was associated with an increased number of withdrawals from treatment due to intolerance and an increased incidence of adverse events.
- Cysteamine has occasionally been associated with reversible leukopenia and abnormal liver function studies. Therefore, blood counts and liver function studies should be monitored.
- There have been reports of benign intracranial hypertension (or pseudotumor cerebri; PTC) and/or papilledema associated with Cysteamine treatment that has resolved with the addition of diuretic therapy. PTC may be more common in cystinotic patients because of concurrent medication and renal transplantation. Although a causal relationship of PTC to Cysteamine has not been established, physicians should monitor patients receiving Cysteamine for this condition. Physicians should instruct patients to report any of the following symptoms: headache, tinnitus, dizziness, nausea, diplopia, blurry vision, loss of vision, pain behind the eye or pain with eye movement. A periodic eye examination is needed to identify this condition early and timely treatment should be provided when it occurs to prevent vision loss.
- There have been reports of serious skin lesions in patients treated with high doses of Cysteamine or other cysteamine salts that have responded to cysteamine dose reduction. These skin lesions are purplish hemorrhagic lesions over the elbow area on both arms and have been described as molluscoid pseudotumors. Skin striae, bone lesions (that have been described as osteopenia, compression fractures, scoliosis and genu valgum) along with leg pain and joint hyperextension may also be present. One patient with serious skin lesions subsequently died of acute cerebral ischemia with marked vasculopathy. Physicians should routinely monitor the skin and bones of patients receiving CYSTAGON. If similar skin or bone abnormalities appear, the dose of CYSTAGON should be reduced.
Adverse Reactions
Clinical Trials Experience
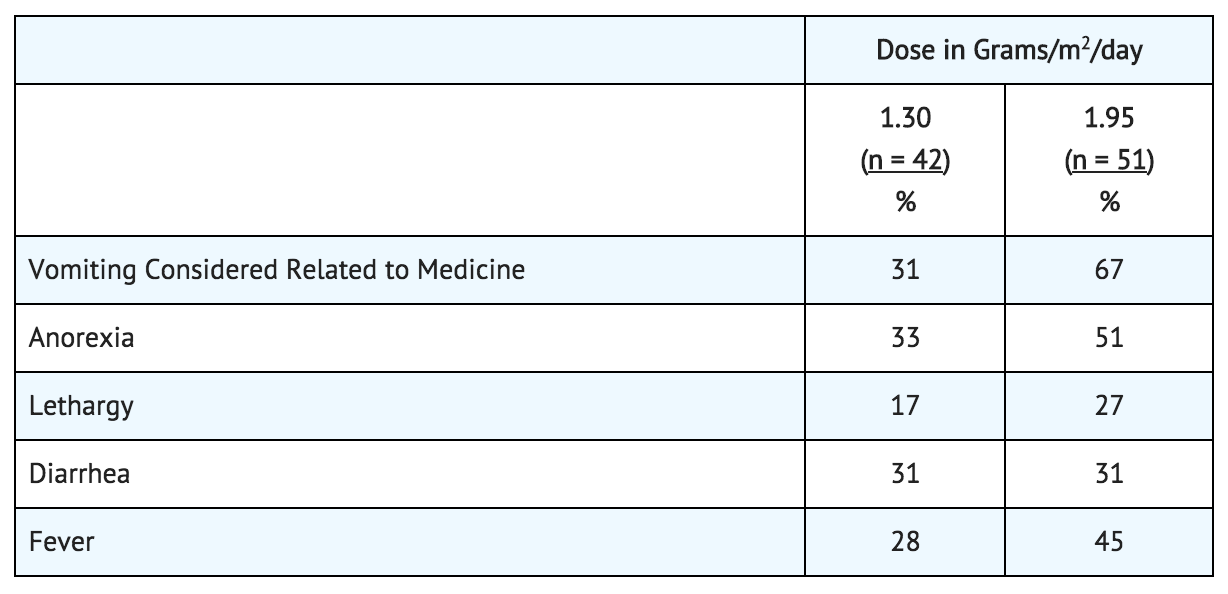
In three clinical trials, cysteamine or phosphocysteamine have been administered to 246 children with cystinosis. Causality of side effects is sometimes difficult to determine because adverse effects may result from the underlying disease.
The most frequent adverse reactions seen involve the gastrointestinal and central nervous systems. These are especially prominent at the initiation of cysteamine therapy. Temporarily suspending treatment, then gradual re-introduction may be effective in improving tolerance.
Adverse reactions were not collected systematically in the NCCS, but were often listed by investigators. The following rates may therefore be underestimated. The most common events (> 5%) were vomiting 35%, anorexia 31%, fever 22%, diarrhea 16%, lethargy 11%, and rash 7%.
Less common adverse events are:
- Body as a whole: Dehydration.
- Cardiovascular: Hypertension.
- Digestive: nausea, bad breath, abdominal pain, dyspepsia, constipation, gastroenteritis, duodenitis, gastrointestinal ulceration and bleeding.
- Central Nervous System: Somnolence, encephalopathy, headache, seizures, ataxia, confusion, tremor, hyperkinesia, decreasing hearing, dizziness, jitteriness.
- Psychiatric: Nervousness, abnormal thinking, depression, emotional lability, hallucinations, nightmares.
- Integumentary: Urticaria.
- Urogenital: Interstitial nephritis, renal failure.
- Clinical Laboratory: Abnormal liver function, anemia, leukopenia.
Adverse reactions or intolerance leading to cessation of treatment occurred in 8% of patients in the U.S. Studies.
Withdrawals due to intolerance, vomiting associated with medication, anorexia, lethargy, and fever appeared dose related, occurring more frequently in those patients receiving 1.95 grams/m2/day as compared to 1.30 grams/m2/day.
Sudden deaths have been reported in this disease state.
Postmarketing Experience
- Benign intracranial hypertension (or pseudotumor cerebri; PTC) with papilledema; skin lesions, molluscoid pseudotumors, skin striae, skin fragility; joint hyperextension, leg pain, genu valgum, osteopenia, compression fracture and scoliosis have been reported.
- Post marketing reports include one report of interstitial nephritis with early renal failure. A causal relationship between this event and cysteamine bitartrate therapy has not been established.
Drug Interactions
- None have been described. Cysteamine can be administered with electrolyte and mineral replacements necessary for management of the Fanconi Syndrome as well as vitamin D and thyroid hormone.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C
Teratology studies have been performed in rats at oral doses in a range of 37.5 to 150 mg/kg/day (about 0.2 to 0.7 times the recommended human maintenance dose on a body surface basis) and have revealed cysteamine bitartrate to be teratogenic and fetotoxic. Observed teratogenic findings were cleft palate, Kyphosis, heart ventricular septal defects, microcephaly and exencephaly. There are no adequate and well-controlled studies in pregnant women. Cysteamine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Cysteamine (oral) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Cysteamine (oral) during labor and delivery.
Nursing Mothers
It is not known whether cysteamine is excreted in human milk. Because many drugs are excreted in human milk and because of the manifested potential of cysteamine for developmental toxicity in suckling rat pups when it was administered to their lactating mothers at an oral dose of 375 mg/kg/day (2,250 mg/m2/day, 1.7 times the recommended human dose based on body surface area), a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
The safety and effectiveness of Cysteamine for cystinotic children have been established. Cysteamine therapy should be initiated as soon as the diagnosis of nephropathic cystinosis has been confirmed.
Geriatic Use
There is no FDA guidance on the use of Cysteamine (oral) in geriatric settings.
Gender
There is no FDA guidance on the use of Cysteamine (oral) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Cysteamine (oral) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Cysteamine (oral) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Cysteamine (oral) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Cysteamine (oral) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Cysteamine (oral) in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral.
Monitoring
- White cell cystine is monitored in these patients to determine adequacy of dosing, levels being measured 5 to 6 hours after dosing.
- Cysteamine has occasionally been associated with reversible leukopenia and abnormal liver function studies. Therefore, blood counts and liver function studies should be monitored.
- Monitor patients receiving Cysteamine for pseudotumor cerebri.
- Physicians should routinely monitor the skin and bones of patients receiving CYSTAGON.
IV Compatibility
There is limited information regarding the compatibility of Cysteamine (oral) and IV administrations.
Overdosage
- A single oral dose of cysteamine at 660 mg/kg was lethal to rats. Symptoms of acute toxicity were reduction of motor activity and generalized hemorrhage in gastrointestinal tract and kidneys.
- Two cases of human overdosage have been reported. In one case, the patient immediately vomited the drug and did not develop any symptoms. The second incident involved an accidental ingestion of a 200 to 250 mg/kg dose by a healthy 13 month old child. vomiting and dehydration were experienced. The child was hospitalized and fluids were administered. A full recovery was made. Should overdose occur, the respiratory and cardiovascular systems should be supported appropriately. No specific antidote is known. Hemodialysis may be considered since cysteamine is poorly bound to plasma proteins.
Pharmacology
Template:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox entryTemplate:Chembox E numberTemplate:Chembox EUClassTemplate:Chembox SPhrasesTemplate:Chembox Supplement| Template:Chembox header2 | Cysteamine (oral) | |
|---|---|
| Identifiers | |
3D model (JSmol)
|
|
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
| DrugBank | |
| ECHA InfoCard | Lua error in Module:Wikidata at line 879: attempt to index field 'wikibase' (a nil value). Lua error in Module:Wikidata at line 879: attempt to index field 'wikibase' (a nil value). |
| KEGG | |
PubChem CID
|
|
| UNII | |
| |
| |
| Properties | |
| C2H7NS | |
| Molar mass | 77.15 g·mol−1 |
| Hazards | |
| Template:Chembox header2 | Except where noted otherwise, data are given for materials in their standard state (at 25 °C, 100 kPa) Infobox disclaimer and references | |
Mechanism of Action
Cystinosis is an autosomal recessive inborn error of metabolism in which the transport of cystine out of lysosomes is abnormal; in the nephropathic form, accumulation of cystine and formation of crystals damage various organs, especially the kidney, leading to renal tubular Fanconi Syndrome and progressive glomerular failure, with end stage renal failure by the end of the first decade of life. In four studies of cystinosis patients before cysteamine was available, renal death (need for transplant or dialysis) occurred at median age of less than 10 years. Patients with cystinosis also experience growth failure, rickets, and photophobia due to cystine deposits in the cornea. With time most organs are damaged, including the retina, muscles and central nervous system.
Cysteamine is an aminothiol that participates within lysosomes in a thiol-disulfide interchange reaction converting cystine into cysteine and cysteine-cysteamine mixed disulfide, both of which can exit the lysosome in patients with cystinosis.
Structure
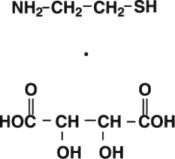
CYSTAGON® (cysteamine bitartrate) Capsules for oral administration, contain cysteamine bitartrate, a cystine depleting agent which lowers the cystine content of cells in patients with cystinosis, an inherited defect of lysosomal transport. Cysteamine is the bitartrate salt of cysteamine, an aminothiol, beta-mercaptoethylamine. Cysteamine bitartrate is a highly water soluble white powder with a molecular weight of 227 and the molecular formula C2H7NS • C4H6O6. It has the following chemical structure:
Pharmacodynamics
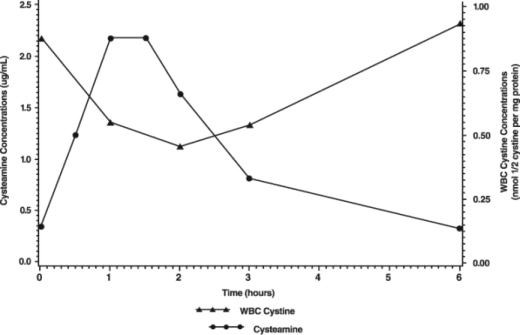
The pharmacokinetics and pharmacodynamics of Cysteamine were studied in eleven pediatric patients with nephropathic cystinosis who received 225 to 550 mg of cysteamine bitartrate every 6 hours daily for more than one year. Following repeated oral administration of 225 to 550 mg cysteamine bitartrate, the mean time to maximum plasma concentration (Tmax) occurred at about 1.4 hours post dose with mean steady-state peak plasma concentration (Cmax) and area under the concentration-time curve (AUC) of 2.6 µg/mL and 6.3 µg∙hr/mL, respectively. The apparent volume of distribution and apparent plasma clearance of cysteamine were 156 L and 1.2 L/min, respectively.
Cysteamine was moderately bound to human plasma proteins, predominantly to albumin, with mean protein binding of about 52%. Plasma protein binding was independent of concentration over the concentration range achieved clinically with the recommended doses.
Pharmacokinetics
The pharmacodynamic response increased with the plasma cysteamine concentration, with maximum response occurring approximately 1.8 hours post dose with an average reduction of white cell cystine concentration of about 0.46 nmol/½ cystine/mg protein and returning to baseline level 6 hours post dose.
The mean white cell cystine concentration and mean cysteamine plasma concentration-time profile is shown below:
Most clinical data have been developed using cysteamine HCl or phosphocysteamine solutions. In all discussions that follow, administered amounts of various cysteamine salts will be expressed as amounts of cysteamine free base.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Cysteamine has not been tested for its carcinogenic potential in long-term animal studies.
- Cysteamine was not mutagenic in the Ames test. It produced a negative response in an in-vitro sister chromatid exchange assay in human lymphocytes, but a positive response in a similar assay in hamster ovarian cells.
- Repeat breeding reproduction studies were conducted in male and female rats. Cysteamine was found to have no effect on fertility and reproductive performance at an oral dose of 75 mg/kg/day (450 mg/m2/day, 0.4 times the recommended human dose based on body surface area). At an oral dose of 375 mg/kg/day (2,250 mg/m2/day, 1.7 times the recommended human dose based on body surface area), it reduced the fertility of the adult rats and the survival of their offspring.
Clinical Studies
There are approximately 200 pre-transplant cystinosis patients in the United States with nephropathic cystinosis and clinical studies have included almost all of them, in addition to about 40 studied in the United Kingdom. For all patients, mean age at entry into studies was just under 4 years. Patients were approximately equally divided between genders and about 85% were white, 9% were black, and 3% were hispanic.
The National Collaborative Cysteamine Study (NCCS) treated 94 children (mainly from the United States) with nephropathic cystinosis with increasing doses of cysteamine HCl (mean dose 54 mg/kg/day) to attain white cell cystine levels of less than 2 nmol/½ cystine/mg protein 5 to 6 hours post-dose, and compared their outcome with an historical control group of 17 children who had been in the placebo group of a randomized placebo-controlled trial of ascorbic acid. Cysteamine treated patients had been diagnosed at a mean age of 22 months and were a mean age of 46 months old at study entry; placebo patients had been diagnosed at about 29 months and were a mean age of about 52 months old at study entry. The principal measures of effectiveness were serum creatinine and calculated creatinine clearance and growth (height).
The average median white cell cystine level attained during treatment in the NCCS was 1.7 ± 0.2 nmol/½ cystine/mg protein. There were 70 cysteamine patients with baseline serum creatinine less than 2 mg/dL who were followed for at least a year and 17 placebo patients. Twelve of the 94 cysteamine treated patients required early dialysis or renal transplant. Median follow-up of cysteamine patients was over 32 months and 20% were followed more than 5 years. For the placebo group median follow-up was 20 months and only one was followed more than 24 months. Among cysteamine patients glomerular function was maintained over time despite the longer period of treatment and follow-up. Placebo treated patients, in contrast, experienced a gradual rise in serum creatinine. Height, corrected for age, was compared for treated patients with the height, at the various ages patients appeared, of the 143 patients initially screened for inclusion in the NCCS. Patients on treatment maintained growth (did not show increasing growth failure compared to normals) although growth velocity did not increase enough to allow patients to catch up to age norms. Renal tubular function was not affected by treatment.
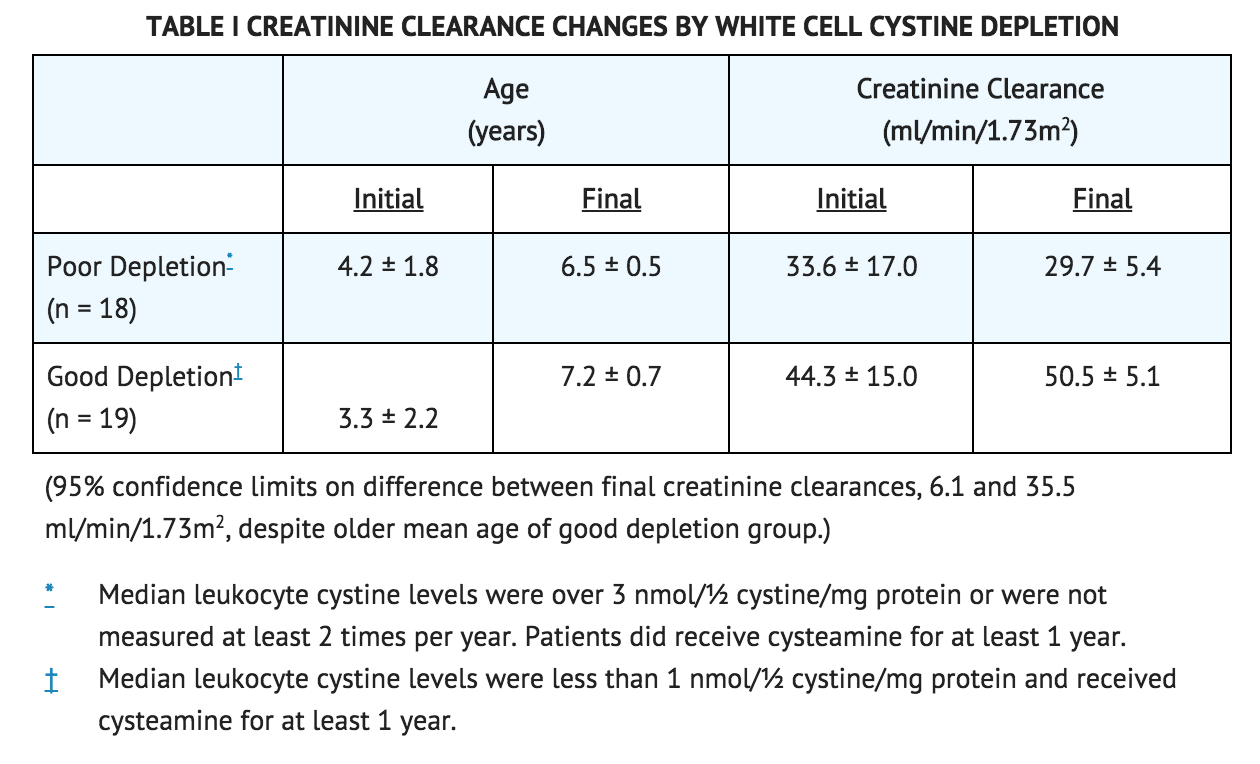
Calculated creatinine clearances were evaluated for two groups of children, one with poor white cell cystine depletion and one with good white cell cystine depletion as shown in Table I. The final mean creatinine clearance of the good depletion group was 20.8 ml/min/1.73 m2 greater than the mean for the poor depletion group, despite the older mean age of the good depletion group.
The Long Term Study, initiated in 1988, utilized both cysteamine HCl and phosphocysteamine (patient's choice) in 46 patients who had completed the NCCS (averaging 6.5 years of treatment) and 93 new patients. Patients had cystinosis diagnosed by elevated white cell cystine (mean 3.63 nmol/½ cystine/mg). New patients and 46 continuing patients were required to have serum creatinine less than 3.0 mg/dL and 4.0 mg/dL, respectively. Patients were randomized to doses of 1.3 or 1.95 g/m2/day and stratified according to whether the serum creatinine was above 1.2 mg/dL or not. Doses could be raised if white cell cystine levels were approximately 2 nmol/½ cystine/mg protein and lowered due to intolerance.
Mean doses were 1.27 g/m2/day and 1.87 g/m2/day in the two groups and white cell cystine levels averaged 1.72 ± 1.65 nmol/½ cystine/mg protein and 1.86 ± 0.92 nmol/½ cystine/mg protein in the 1.3 and 1.95 g/m2/day groups, respectively. In new patients, a group similar in age to the NCCS group, serum creatinine was essentially unchanged over the period of follow-up (about half of the patients were followed for 24 months) and phosphocysteamine and cysteamine HCl had similar effects. The long-term follow-up group, about nine years old on average at entry, stayed in the study (almost 80% were followed at least 2 years) and had essentially no change in renal function. In four studies of untreated cystinosis, renal death (need for transplant or dialysis) occurred at median age of less than 10 years. Both groups maintained height (although they did not catch up from baseline). There was no apparent difference between the two doses.
How Supplied
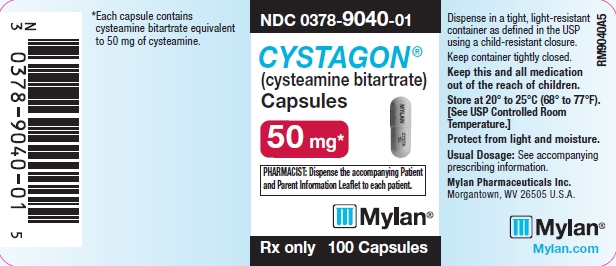
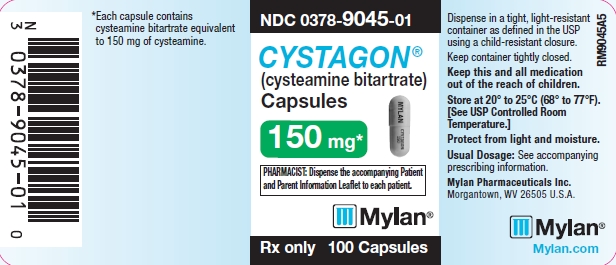
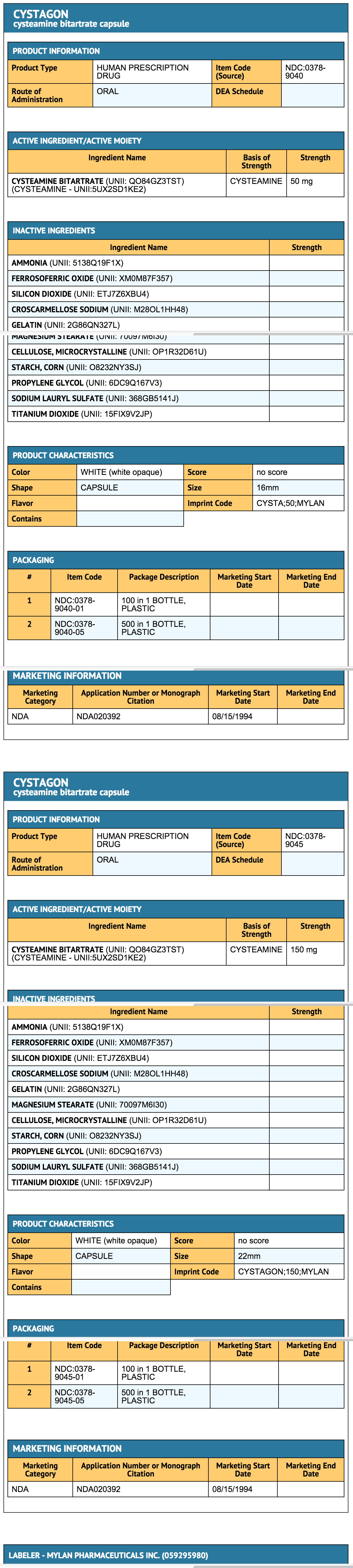
CYSTAGON® (cysteamine bitartrate) Capsules are hard gelatin capsules which provide 50 mg or 150 mg of cysteamine free base as cysteamine bitartrate:
- CYSTAGON® Capsules, 50 mg are white, opaque capsules printed with CYSTA 50 on the body and MYLAN on the cap. They are available as follows:
- NDC 0378-9040-05
- bottles of 500 capsules
- CYSTAGON® Capsules, 150 mg are white, opaque capsules printed with CYSTAGON 150 on the body and MYLAN on the cap. They are available as follows:
- NDC 0378-9045-05
- bottles of 500 capsules
Storage
- Store at 20° to 25°C (68° to 77°F). [See USP for Controlled Room Temperature.]
- Protect from light and moisture.
- Dispense in a tight, light-resistant container as defined in the USP using a child-resistant closure.
Images
Drug Images
{{#ask: Page Name::Cysteamine (oral) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Cysteamine (oral) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Precautions with Alcohol
Alcohol-Cysteamine interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- CYSTAGON ®[1]
Look-Alike Drug Names
There is limited information regarding Look-Alike Drug Names.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- Pages with script errors
- Chemical articles with multiple compound IDs
- Multiple chemicals in an infobox that need indexing
- Chemical articles with multiple CAS registry numbers
- Chemical articles with unknown parameter in Chembox
- ECHA InfoCard ID from Wikidata
- Chembox having DSD data
- Amines
- Drug
- Orphan drugs
- Thiols