Arginemia
| Arginemia | |
 | |
|---|---|
| Arginine | |
| OMIM | 207800 |
| DiseasesDB | 29677 |
| eMedicine | ped/132 |
| MeSH | D020162 |
|
WikiDoc Resources for Arginemia |
|
Articles |
|---|
|
Most recent articles on Arginemia |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Arginemia at Clinical Trials.gov Clinical Trials on Arginemia at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Arginemia
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Arginemia Discussion groups on Arginemia Directions to Hospitals Treating Arginemia Risk calculators and risk factors for Arginemia
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Arginemia |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
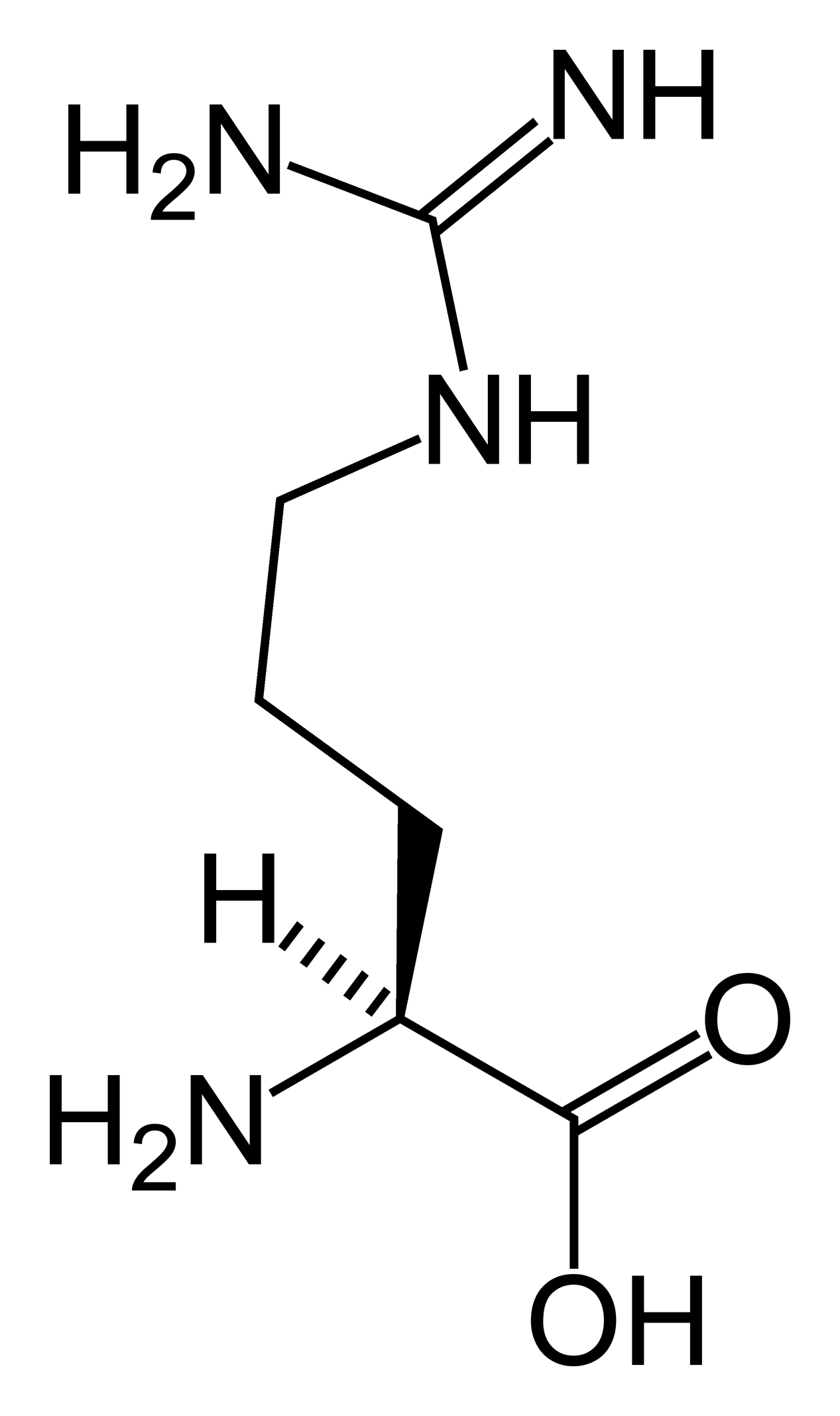
Arginemia (also called arginase deficiency) is a congenital disorder where arginase deficiency causes a high level of arginine and ammonia in the blood. Ammonia, which is formed when proteins are broken down in the body, is toxic if levels become too high. The nervous system is especially sensitive to the effects of excess ammonia.
Arginase deficiency usually becomes evident by about the age of 3. It most often appears as stiffness, especially in the legs, caused by abnormal tensing of the muscles (spasticity). Other symptoms may include slower than normal growth, developmental delay and eventual loss of developmental milestones, mental retardation, seizures, tremor, and difficulty with balance and coordination (ataxia). Occasionally, high protein meals or stress caused by illness or periods without food (fasting) may cause ammonia to accumulate more quickly in the blood. This rapid increase in ammonia may lead to episodes of irritability, refusal to eat, and vomiting.
In some affected individuals, signs and symptoms of arginase deficiency may be less severe, and may not appear until later in life.
Mutations in the ARG1 gene cause arginase deficiency. Arginase deficiency belongs to a class of genetic diseases called urea cycle disorders. The urea cycle is a sequence of reactions that occurs in liver cells. This cycle processes excess nitrogen, generated when protein is used by the body, to make a compound called urea that is excreted by the kidneys.
The ARG1 gene provides instructions for making an enzyme called arginase. This enzyme controls the final step of the urea cycle, which produces urea by removing nitrogen from arginine. In people with arginase deficiency, arginase is damaged or missing, and arginine is not broken down properly. As a result, urea cannot be produced normally, and excess nitrogen accumulates in the blood in the form of ammonia. The accumulation of ammonia and arginine are believed to cause the neurological problems and other signs and symptoms of arginase deficiency.

This condition is inherited in an autosomal recessive pattern, which means two copies of the gene in each cell are altered. Most often, the parents of an individual with an autosomal recessive disorder are carriers of one copy of the altered gene but do not show signs and symptoms of the disorder.
Differential diagnosis
Arginase deficiency must be differentiated from other diseases that cause neurological manifestations in infants.
| Diseases | Type of motor abnormality | Clinical findings | Laboratory findings and diagnostic tests | Radiographic findings | |||
|---|---|---|---|---|---|---|---|
| Spasticity | Hypotonia | Ataxia | Dystonia | ||||
| Leigh syndrome | - | - | + | + |
|
| |
| Niemann-Pick disease type C | - | - | + | + |
|
|
|
| Infantile Refsum disease | - | + | + | - |
|
Elevated plasma VLCFA levels | -- |
| Adrenoleukodystrophy | + | - | - | - |
|
|
-- |
| Zellweger syndrome | - | + | - | - |
|
|
-- |
| Pyruvate dehydrogenase deficiency | + | + | + | - | -- | ||
| Arginase deficiency | + | - | - | - | -- | ||
| Holocarboxylase synthetase deficiency | - | + | - | - | Elevated levels of:
|
-- | |
| Glutaric aciduria type 1 | - | - | - | + |
|
Elevated levels of:
|
|
| Ataxia telangiectasia | - | - | + | - |
|
|
-- |
| Pontocerebellar hypoplasias | - | + | - | - |
|
Genetic testing for PCH gene mutations |
|
| Metachromatic leukodystrophy | - | + | + | - |
|
|
-- |
| Pelizaeus-Merzbacher | + | - | + | - |
|
| |
| Angelman syndrome | - | - | + | - |
|
|
-- |
| Rett syndrome | + | - | - | + |
|
-- | |
| Lesch-Nyhan syndrome | + | - | - | + |
|
-- | |
| Miller-Dieker lissencephaly | + | + | - | - |
|
|
-- |
| Dopa-responsive dystonia | + | - | - | + |
|
|
-- |