Gastric lymphoma: Difference between revisions
Mazia Fatima (talk | contribs) |
Mazia Fatima (talk | contribs) |
||
| Line 354: | Line 354: | ||
==Natural History, Complications and Prognosis== | ==Natural History, Complications and Prognosis== | ||
===Natural History=== | ===Natural History=== | ||
*The majority of patients with primary gastric lymphoma present with nonspecific symptoms in the 5th decade of life. | |||
*Early clinical features include epigastric pain, nausea, and vomiting. | |||
*If left untreated, patients with gastric lymphoma may progress to develop anorexia, weight loss, and early satiety. | |||
===Complications=== | ===Complications=== | ||
*Common complications of gastric lymphoma include perforation, hemorrhage, and obstruction. | |||
===Prognosis=== | ===Prognosis=== | ||
*Prognosis is generally good, and complete remission can be achieved after 6-8 rounds of chemotherapy or following surgery. | |||
==Diagnosis== | ==Diagnosis== | ||
Revision as of 16:07, 16 January 2018
|
WikiDoc Resources for Gastric lymphoma |
|
Articles |
|---|
|
Most recent articles on Gastric lymphoma Most cited articles on Gastric lymphoma |
|
Media |
|
Powerpoint slides on Gastric lymphoma |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Gastric lymphoma at Clinical Trials.gov Trial results on Gastric lymphoma Clinical Trials on Gastric lymphoma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Gastric lymphoma NICE Guidance on Gastric lymphoma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Gastric lymphoma Discussion groups on Gastric lymphoma Patient Handouts on Gastric lymphoma Directions to Hospitals Treating Gastric lymphoma Risk calculators and risk factors for Gastric lymphoma
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Gastric lymphoma |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Mazia Fatima, MBBS [2]
Overview
Primary gastric lymphoma is cancer derived from lymphocytes (a type of white blood cell) that originates in the stomach.[1][2]
Most common cause of primary gastric lymphoma is mucosa-associated lymphoid tissue (MALT) lymphoma and diffuse large B-cell lymphoma (DLBCL) of the stomach. These account for 90% of all diagnosed cases. Lymphomas originating outside the lymph nodes are referred to as extra nodal lymphoma. Primary gastric lymphoma is the most common type of extra nodal lymphoma.
Primary gastric Lymphoma is a rare condition Gastric lymphoma accounts for less than 15% of gastric malignancies and about 2% of all lymphomas. Most of the primary gastric lymphomas are B cell non-Hodgkin lymphoma(NHL).
Classification
Primary gastric lymphoma may be classified according to histology into the following subtypes:
- B-cell lymphomas are of two main types:
- MALT lymphoma
- DLBCL
- MALT lymphoma can be further divided into:
- H. pylori positive MALT lymphoma
- H. pylori negative MALT lymphoma
- DLBCL can be divided into 3 subgroups based on the gene expression:
- Germinal-center B-cell-like
- Activated B-cell-like
- Primary mediastinal DLBCL
Pathophysiology
- The exact pathogenesis of primary gastric lymphoma is not fully understood.[3][4]
- Most of the MALT lymphomas have an associated history of H.pylori infection. Chronic inflammation associated with H.pylori can cause T and B cell proliferation that increases the risk of malignant transformation.
In case of DLBCL, antibiotic eradication therapy for H.pylori has shown to result in complete remission of lymphoma highlighting the role of H.pylori in the pathogenesis.
- HBV plays a role in the pathogenesis of B-cell NHL, evidenced by an increased risk of developing NHL in HBsAg positive patients.
Histopathology
Most of the gastric lymphomas are predominantly non-Hodgkin’s lymphoma of B-cell origin. Primary gastric lymphoma can vary from being well-differentiated, low-grade lymphomas to high grade or large cell lymphomas.[5]
Symptoms
Common Symptoms
Common symptoms of primary gastric lymphoma include:[6][7]
- Epigastric discomfort
- Anorexia
- Weight loss
- Nausea associated with or without vomiting
- Occult gastrointestinal bleeding
- Early satiety
Less Common Symptoms
Less common symptoms include :
Physical Examination
Appearance of the Patient
Vital signs
Vital signs are within normal limits unless there is complication.
Abdominal Examination
- Physical examination of patients with primary gastric lymphoma is usually remarkable for palpable mass and peripheral lymphadenopathy.
Differential Diagnosis
Gastric lymphoma must be differentiated from conditions with similar presentation like acute gastritis, chronic gastritis, atrophic gastritis, Crohn's disease, gastroesophageal reflux disease, peptic ulcer disease, gastrinoma and gastric adenocarcinoma :[8][9][10][11][12][13][14][15][16]
| Disease | Cause | Symptoms | Diagnosis | Other findings | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pain | Nausea
& Vomiting |
Heartburn | Belching or
Bloating |
Weight loss | Loss of
Appetite |
Stools | Endoscopy findings | |||||
| Location | Aggravating Factors | Alleviating Factors | ||||||||||
| Primary gastric lymphoma |
|
- | - | - | - | - | ? | - | - | Useful in collecting the tissue for biopsy | Other symptoms
| |
| Acute gastritis |
|
Food | Antacids | ? | ? | ? | - | ? | Black stools | - | ||
| Chronic gastritis |
|
Food | Antacids | ? | ? | ? | ? | ? | - | H. pylori gastritis
Lymphocytic gastritis
|
- | |
| Atrophic gastritis | Epigastric pain | - | - | ? | - | ? | ? | - | H. pylori
|
Autoimmune gastritis diagnosis include:
| ||
| Crohn's disease | - | - | - | - | - | ? | ? |
|
|
|||
| GERD |
|
|
|
?
(Suspect delayed gastric emptying) |
? | - | - | - | - |
|
Other symptoms:
Complications
| |
| Peptic ulcer disease |
|
|
Duodenal ulcer
|
|
? | ? | - | - | - | Gastric ulcers
Duodenal ulcers
|
Other diagnostic tests | |
| Gastrinoma |
|
- | - | ?
(suspect gastric outlet obstruction) |
? | - | - | - | Useful in collecting the tissue for biopsy |
Diagnostic tests
| ||
| Gastric Adenocarcinoma |
|
- | - | ? | ? | ? | ? | ? |
|
Esophagogastroduodenoscopy
|
Other symptoms | |
Demographics
- Primary gastric lymphoma commonly affects elderly patients in the fifth or sixth decade of life.[17]
Risk Factors
Risk factors for gastric lymphoma include the following:[18]
- Helicobacter pylori
- Long-term immunosuppressant drug therapy
- HIV infection
Natural History, Complications and Prognosis
Natural History
- The majority of patients with primary gastric lymphoma present with nonspecific symptoms in the 5th decade of life.
- Early clinical features include epigastric pain, nausea, and vomiting.
- If left untreated, patients with gastric lymphoma may progress to develop anorexia, weight loss, and early satiety.
Complications
- Common complications of gastric lymphoma include perforation, hemorrhage, and obstruction.
Prognosis
- Prognosis is generally good, and complete remission can be achieved after 6-8 rounds of chemotherapy or following surgery.
Diagnosis
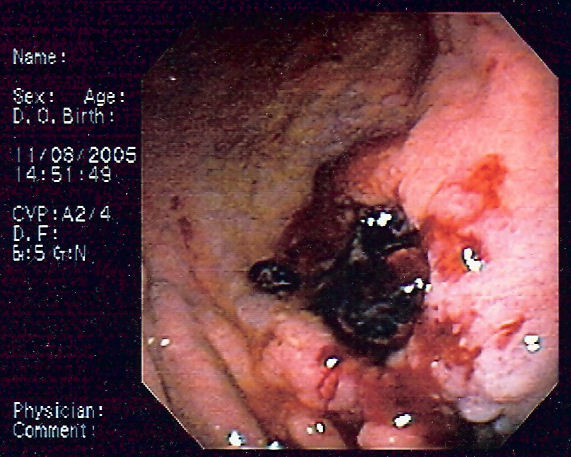
- Upper gastrointestinal endoscopy with biopsy is the gold standard test for the diagnosis of gastric lymphoma.[19][20][5]
- Laparotomy and laparoscopy should be performed when the patient presents with complications such as perforation or obstruction.
- Findings on upper gastrointestinal endoscopy suggestive of gastric lymphoma:
An endoscopic ultrasound (EUS) will help assess the depth of lymphoma invasion and involvement of perigastric nodes. MALT lymphoma presents as superficial spreading or diffuse infiltrating lesion whereas diffuse large B cell lymphoma has a typical mass forming lesion appearance on endoscopic ultrasound. Imaging investigations including CT scans or endoscopic ultrasound are useful to stage disease. Hematological parameters are usually checked to assist with staging and to exclude concomitant leukemia. An elevated LDH level may be suggestive of lymphoma. MRI features include irregularly thickened mucosal folds, irregular submucosal infiltration, annular constricting lesion, exophytic tumor growth, mesenteric masses and mesenteric/retroperitoneal lymphadenopathy. The tumors are usually homogeneous and intermediate in signal intensity on T1-weighted images. Heterogeneously increased signal intensities are noted on T2-weighted images. The enhancement is usually mild-moderate after intravenous administration of gadolinium dimeglumine
Treatment
- The predominant therapy for diffuse large B-cell lymphomas of the stomach is chemotherapy.[21][22]
- Second line therapy for MALT lymphomas is usually chemotherapy with a single agent, and complete response rates of greater than 70% have been observed.
- Chemotherapy includes treatment with CHOP with or without rituximab.
- The mainstay of therapy for MALT lymphomas is antibiotic treatment to eradicate H.pylori. Regression is seen in about 60% of cases with eradication therapy alone.
- Single drug chemotherapy is recommended as a second line therapy for MALT lymphomas and is associated with a complete resolution of symptoms in greater than 70% cases.
- In case of complications like gastric outlet obstruction, the recommended treatment is subtotal gastrectomy followed by post-operative.
Prevention
Primary Prevention
There are no established measures for the primary prevention of gastric lymphoma.
Secondary Prevention
There are no established measures for the secondary prevention of gastric lymphoma.
References
- ↑ Dawson IMP, Cornes JS, Morrison BC. Primary malignant lymphoid tumours of the intestinal tract. Br J Surg. 1961;49:80-89.
- ↑ Aisenberg AC. Coherent view of non-Hodgkin's lymphoma. J Clin Oncol. 1995;13:2656-2675.
- ↑ Hussell T, Isaacson PG, Crabtree JE, Spencer J (1996). "Helicobacter pylori-specific tumour-infiltrating T cells provide contact dependent help for the growth of malignant B cells in low-grade gastric lymphoma of mucosa-associated lymphoid tissue". J. Pathol. 178 (2): 122–7. doi:10.1002/(SICI)1096-9896(199602)178:2<122::AID-PATH486>3.0.CO;2-D. PMID 8683376.
- ↑ Engels EA, Cho ER, Jee SH (2010). "Hepatitis B virus infection and risk of non-Hodgkin lymphoma in South Korea: a cohort study". Lancet Oncol. 11 (9): 827–34. doi:10.1016/S1470-2045(10)70167-4. PMC 2933963. PMID 20688564.
- ↑ 5.0 5.1 Wang T, Gui W, Shen Q (2010). "Primary gastrointestinal non-Hodgkin's lymphoma: clinicopathological and prognostic analysis". Med. Oncol. 27 (3): 661–6. doi:10.1007/s12032-009-9265-1. PMID 19565363.
- ↑ Freeman C, Berg JW, Cutler SJ (1972). "Occurrence and prognosis of extranodal lymphomas". Cancer. 29 (1): 252–60. PMID 5007387.
- ↑ 7.0 7.1 Koch P, del Valle F, Berdel WE, Willich NA, Reers B, Hiddemann W, Grothaus-Pinke B, Reinartz G, Brockmann J, Temmesfeld A, Schmitz R, Rübe C, Probst A, Jaenke G, Bodenstein H, Junker A, Pott C, Schultze J, Heinecke A, Parwaresch R, Tiemann M (2001). "Primary gastrointestinal non-Hodgkin's lymphoma: I. Anatomic and histologic distribution, clinical features, and survival data of 371 patients registered in the German Multicenter Study GIT NHL 01/92". J. Clin. Oncol. 19 (18): 3861–73. doi:10.1200/JCO.2001.19.18.3861. PMID 11559724.
- ↑ Sugimachi K, Inokuchi K, Kuwano H, Ooiwa T (1984). "Acute gastritis clinically classified in accordance with data from both upper GI series and endoscopy". Scand J Gastroenterol. 19 (1): 31–7. PMID 6710074.
- ↑ Sipponen P, Maaroos HI (2015). "Chronic gastritis". Scand J Gastroenterol. 50 (6): 657–67. doi:10.3109/00365521.2015.1019918. PMC 4673514. PMID 25901896.
- ↑ Sartor RB (2006). "Mechanisms of disease: pathogenesis of Crohn's disease and ulcerative colitis". Nat Clin Pract Gastroenterol Hepatol. 3 (7): 390–407. doi:10.1038/ncpgasthep0528. PMID 16819502.
- ↑ Sipponen P (1989). "Atrophic gastritis as a premalignant condition". Ann Med. 21 (4): 287–90. PMID 2789799.
- ↑ Badillo R, Francis D (2014). "Diagnosis and treatment of gastroesophageal reflux disease". World J Gastrointest Pharmacol Ther. 5 (3): 105–12. doi:10.4292/wjgpt.v5.i3.105. PMC 4133436. PMID 25133039.
- ↑ Ramakrishnan K, Salinas RC (2007). "Peptic ulcer disease". Am Fam Physician. 76 (7): 1005–12. PMID 17956071.
- ↑ Banasch M, Schmitz F (2007). "Diagnosis and treatment of gastrinoma in the era of proton pump inhibitors". Wien Klin Wochenschr. 119 (19–20): 573–8. doi:10.1007/s00508-007-0884-2. PMID 17985090.
- ↑ Dicken BJ, Bigam DL, Cass C, Mackey JR, Joy AA, Hamilton SM (2005). "Gastric adenocarcinoma: review and considerations for future directions". Ann Surg. 241 (1): 27–39. PMC 1356843. PMID 15621988.
- ↑ Ghimire P, Wu GY, Zhu L (2011). "Primary gastrointestinal lymphoma". World J Gastroenterol. 17 (6): 697–707. doi:10.3748/wjg.v17.i6.697. PMC 3042647. PMID 21390139.
- ↑ Thirlby RC. Gastrointestinal lymphoma: a surgical perspective. Oncology (Huntingt). 1993;7:29-32.
- ↑ NEJM article
- ↑ Cogliatti SB, Schmid U, Schumacher U, Eckert F, Hansmann ML, Hedderich J, Takahashi H, Lennert K (1991). "Primary B-cell gastric lymphoma: a clinicopathological study of 145 patients". Gastroenterology. 101 (5): 1159–70. PMID 1936785.
- ↑ Muller AF, Maloney A, Jenkins D, Dowling F, Smith P, Bessell EM, Toghill PJ (1995). "Primary gastric lymphoma in clinical practice 1973-1992". Gut. 36 (5): 679–83. PMC 1382669. PMID 7797116.
- ↑ Hauptrock B, Hess G (2008). "Rituximab in the treatment of non-Hodgkin's lymphoma". Biologics. 2 (4): 619–33. PMC 2727901. PMID 19707443.
- ↑ Morgner A, Schmelz R, Thiede C, Stolte M, Miehlke S (2007). "Therapy of gastric mucosa associated lymphoid tissue lymphoma". World J. Gastroenterol. 13 (26): 3554–66. PMC 4146794. PMID 17659705.