Chickenpox differential diagnosis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 101: | Line 101: | ||
===Differentiating chickenpox infection in [[immunocompromised]] host=== | ===Differentiating chickenpox infection in [[immunocompromised]] host=== | ||
[[Varicella Zoster Virus|Varicella Zoster virus]] infection is common among [[immunocompromised]] patients who are at high risk for other [[fungal]], [[bacterial]], and [[viral]] infections. It should be differentiated from the following diseases, which may present as [[confusion]], [[fever]] and [[headache]] in [[immunocompromised]] patients: | |||
{| class="wikitable" | {| class="wikitable" | ||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Disease | ! align="center" style="background:#4479BA; color: #FFFFFF;" + |Disease | ||
| Line 110: | Line 110: | ||
| | | | ||
* Patient is [[immunocompetent]] | * Patient is [[immunocompetent]] | ||
* Focal symptoms indicative of a mass [[lesion]] | * Focal [[symptoms]] indicative of a mass [[lesion]] | ||
* [[Seizure]] | * [[Seizure]] | ||
| | | | ||
| Line 121: | Line 121: | ||
| | | | ||
* [[PCR]] of [[CSF]] for [[tuberculosis]] | * [[PCR]] of [[CSF]] for [[tuberculosis]] | ||
* Mycobacterial culture of [[CSF]] | * [[Mycobacterial]] [[Culture media|culture]] of [[CSF]] | ||
* [[Brain]] biopsy for [[acid-fast bacilli]] staining | * [[Brain]] biopsy for [[acid-fast bacilli]] staining | ||
* Culture and acid stain positive for [[acid-fast bacilli]] | * [[Culture medium|Culture]] and acid stain positive for [[acid-fast bacilli]] | ||
* CXR shows [[Cavitation|cavitations]] | * [[Chest X-ray|CXR]] shows [[Cavitation|cavitations]] | ||
|- | |- | ||
|[[Aspergillosis]]<ref name="pmid10194462">{{cite journal |vauthors=Latgé JP |title=Aspergillus fumigatus and aspergillosis |journal=Clin. Microbiol. Rev. |volume=12 |issue=2 |pages=310–50 |year=1999 |pmid=10194462 |pmc=88920 |doi= |url=}}</ref> | |[[Aspergillosis]]<ref name="pmid10194462">{{cite journal |vauthors=Latgé JP |title=Aspergillus fumigatus and aspergillosis |journal=Clin. Microbiol. Rev. |volume=12 |issue=2 |pages=310–50 |year=1999 |pmid=10194462 |pmc=88920 |doi= |url=}}</ref> | ||
| | | | ||
* [[Pulmonary]] [[lesions]] in addition to [[CNS]] [[lesions]] | * [[Pulmonary]] [[lesions]] in addition to [[CNS]] [[lesions]] | ||
* Symptoms may include [[cough]], [[chest pain]], and [[hemoptysis]] | * [[Symptoms]] may include [[cough]], [[chest pain]], and [[hemoptysis]] | ||
| | | | ||
*[[CSF]] fungal culture, [[galactomannan]] | *[[CSF]] [[fungal]] [[Culture medium|culture]], [[galactomannan]] | ||
|- | |- | ||
|[[Cryptococcosis]] | |[[Cryptococcosis]] | ||
| | | | ||
*Symptoms include [[cough]], [[chest pain]], and [[hemoptysis]] | *[[Symptoms]] include [[cough]], [[chest pain]], and [[hemoptysis]] | ||
| | | | ||
*[[Cryptococcal infection|Cryptococcal]] [[antigen]] from [[CSF]] and [[serum]] | *[[Cryptococcal infection|Cryptococcal]] [[antigen]] from [[CSF]] and [[serum]] | ||
*[[CSF]] fungal culture | *[[CSF]] [[fungal]] [[Culture medium|culture]] | ||
|- | |- | ||
|[[Chagas disease]]<ref name="pmid20399979">{{cite journal |vauthors=Rassi A, Rassi A, Marin-Neto JA |title=Chagas disease |journal=Lancet |volume=375 |issue=9723 |pages=1388–402 |year=2010 |pmid=20399979 |doi=10.1016/S0140-6736(10)60061-X |url=}}</ref> | |[[Chagas disease]]<ref name="pmid20399979">{{cite journal |vauthors=Rassi A, Rassi A, Marin-Neto JA |title=Chagas disease |journal=Lancet |volume=375 |issue=9723 |pages=1388–402 |year=2010 |pmid=20399979 |doi=10.1016/S0140-6736(10)60061-X |url=}}</ref> | ||
| | | | ||
*History of residence in Central or | *History of residence in Central or South America | ||
*Acute infection is rarely symptomatic | *Acute infection is rarely symptomatic | ||
*[[Encephalitis]] or focal [[brain]] [[lesions]] | *[[Encephalitis]] or focal [[brain]] [[lesions]] | ||
| Line 154: | Line 154: | ||
*Most common [[CNS]] [[opportunistic infection]] in [[AIDS]] patients | *Most common [[CNS]] [[opportunistic infection]] in [[AIDS]] patients | ||
*Presents with [[encephalitis]], [[retinitis]], progressive [[myelitis]], or [[polyradiculitis]] | *Presents with [[encephalitis]], [[retinitis]], progressive [[myelitis]], or [[polyradiculitis]] | ||
*In [[disseminated disease]], it involves both the [[liver]] and kidneys | *In [[disseminated disease]], it involves both the [[liver]] and [[kidneys]] | ||
| | | | ||
*[[Brain]] [[CT]]/[[MRI]]/[[biopsy]]: location of [[lesions]] is usually near the [[brain stem]] or periventricular areas | *[[Brain]] [[CT]]/[[MRI]]/[[biopsy]]: location of [[lesions]] is usually near the [[brain stem]] or periventricular areas | ||
| Line 171: | Line 171: | ||
|[[Chickenpox|Varicella Zoster infection]]<ref name="pmid15864101">{{cite journal |vauthors=Hambleton S |title=Chickenpox |journal=Curr. Opin. Infect. Dis. |volume=18 |issue=3 |pages=235–40 |year=2005 |pmid=15864101 |doi= |url=}}</ref> | |[[Chickenpox|Varicella Zoster infection]]<ref name="pmid15864101">{{cite journal |vauthors=Hambleton S |title=Chickenpox |journal=Curr. Opin. Infect. Dis. |volume=18 |issue=3 |pages=235–40 |year=2005 |pmid=15864101 |doi= |url=}}</ref> | ||
| | | | ||
*Multifocal involvement has subacute course, usually only in [[immunosuppressed]], with [[headache]], [[fever]], focal deficits, and [[seizures]] | *Multifocal involvement has subacute course, usually only in [[immunosuppressed]], with [[headache]], [[fever]], focal deficits, and [[seizures]] | ||
*Unifocal involvement is more typically seen in [[immunocompetent]] hosts, occurring after [[contralateral]] [[cranial nerve]] [[herpes zoster]], with [[Altered mental status|mental status changes]], [[TIA|TIAs]], and [[stroke]] | *Unifocal involvement is more typically seen in [[immunocompetent]] hosts, occurring after [[contralateral]] [[cranial nerve]] [[herpes zoster]], with [[Altered mental status|mental status changes]], [[TIA|TIAs]], and [[stroke]] | ||
*[[Disseminated disease|Disseminated]] [[varicella zoster virus]] can occur in adults during primary [[infection]], presenting with [[pneumonitis]] and/or [[hepatitis]] | *[[Disseminated disease|Disseminated]] [[varicella zoster virus]] can occur in adults during primary [[infection]], presenting with [[pneumonitis]] and/or [[hepatitis]] | ||
| Line 181: | Line 181: | ||
| | | | ||
*Associated with [[sinusitis]] (abutting the sinuses) or with [[bacteremia]] | *Associated with [[sinusitis]] (abutting the sinuses) or with [[bacteremia]] | ||
*Signs and symptoms includes [[fever]] and [[necrotizing]] [[brain]] [[lesions]] with [[mass effect]] | *Signs and [[symptoms]] includes [[fever]] and [[necrotizing]] [[brain]] [[lesions]] with [[mass effect]] | ||
| | | | ||
*[[CSF]] culture or culture of [[brain abscess]] | *[[CSF]] [[Culture medium|culture]] or [[Culture media|culture]] of [[brain abscess]] | ||
|- | |- | ||
|[[Progressive multifocal leukoencephalopathy]]<ref name="pmid20298966">{{cite journal |vauthors=Tan CS, Koralnik IJ |title=Progressive multifocal leukoencephalopathy and other disorders caused by JC virus: clinical features and pathogenesis |journal=Lancet Neurol |volume=9 |issue=4 |pages=425–37 |year=2010 |pmid=20298966 |pmc=2880524 |doi=10.1016/S1474-4422(10)70040-5 |url=}}</ref> | |[[Progressive multifocal leukoencephalopathy]]<ref name="pmid20298966">{{cite journal |vauthors=Tan CS, Koralnik IJ |title=Progressive multifocal leukoencephalopathy and other disorders caused by JC virus: clinical features and pathogenesis |journal=Lancet Neurol |volume=9 |issue=4 |pages=425–37 |year=2010 |pmid=20298966 |pmc=2880524 |doi=10.1016/S1474-4422(10)70040-5 |url=}}</ref> | ||
| | | | ||
*Symptoms are often more insidious in onset and progress over months. Symptoms include progressive [[weakness]], poor [[coordination]], with gradual slowing of [[mental]] function. Only seen in the [[immunosuppressed]]. Rarely associated with [[fever]] or other systemic symptoms | *[[Symptoms]] are often more insidious in onset and progress over months. [[Symptoms]] include progressive [[weakness]], poor [[coordination]], with gradual slowing of [[mental]] function. Only seen in the [[immunosuppressed]]. Rarely associated with [[fever]] or other systemic [[symptoms]] | ||
| | | | ||
Revision as of 21:24, 16 August 2017
|
Chickenpox Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Chickenpox differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Chickenpox differential diagnosis |
|
Risk calculators and risk factors for Chickenpox differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Michael Maddaleni, B.S. João André Alves Silva, M.D. [2] Aravind Reddy Kothagadi M.B.B.S[3]
Overview
Chickenpox must be differentiated from various rash-causing conditions like Coxsackievirus, Stevens-Johnson syndrome (SJS), measles, rubella, Rocky mountain spotted fever and syphilis.
Differentiating Chickenpox from other Diseases
Different rash-like conditions can be confused with chickenpox and are thus included in its differential diagnosis. The various conditions that should be differentiated from chickenpox include:[1][2][3][4][5][6][7]
Common conditions to be differentiated from chickenpox:
| Common Conditions | Features |
|---|---|
| Coxsackievirus |
|
| Stevens-Johnson syndrome |
|
| Kawasaki disease |
|
| Measles |
|
| Syphilis | It commonly presents with gneralized systemic symptoms such as malaise, fatigue, headache and fever. Skin eruptions may be subtle and asymptomatic It is classically described as:
|
| Rubella |
|
| Cytomegalovirus |
|
| Meningococcemia |
|
| Meningitis |
|
| Rocky Mountain spotted fever |
|
| Molluscum contagiosum |
|
| Mononucleosis |
|
Less common conditions to be differentiated from chickenpox:
| Less Common Diseases | Features |
|---|---|
| Atypical measles |
|
| Parvovirus B19 |
|
| Rickettsial pox | |
| Toxic erythema | |
| Monkeypox |
|
| Rat-bite fever | |
| Scarlet fever |
|
Differentiating chickenpox infection in immunocompromised host
Varicella Zoster virus infection is common among immunocompromised patients who are at high risk for other fungal, bacterial, and viral infections. It should be differentiated from the following diseases, which may present as confusion, fever and headache in immunocompromised patients:
| Disease | Differentiating signs and symptoms | Differentiating tests |
|---|---|---|
| CNS lymphoma[8] |
|
|
| Disseminated tuberculosis[9] |
|
|
| Aspergillosis[10] |
|
|
| Cryptococcosis |
|
|
| Chagas disease[11] |
|
|
| CMV infection[12] |
|
|
| HSV infection[13] |
|
|
| Varicella Zoster infection[14] |
|
|
| Brain abscess[15][16] |
|
|
| Progressive multifocal leukoencephalopathy[17] |
|
Oral lesions to be differentiated from chicken pox:
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Coxsackie virus |
|
|
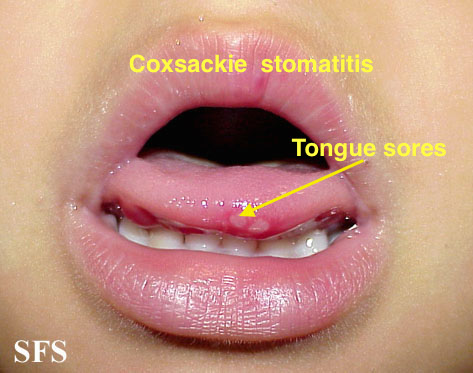
| |||
| Chicken pox |
|
|
|
|
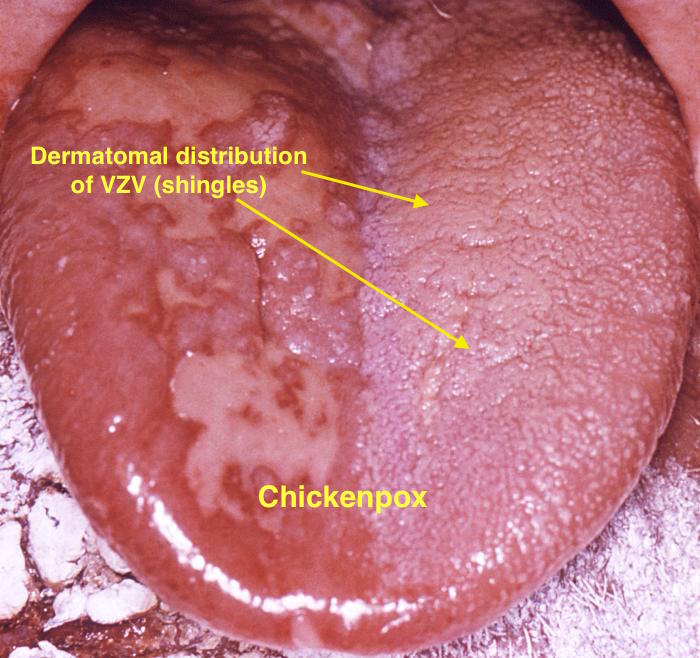
| |
| Measles |
|
|
|
|
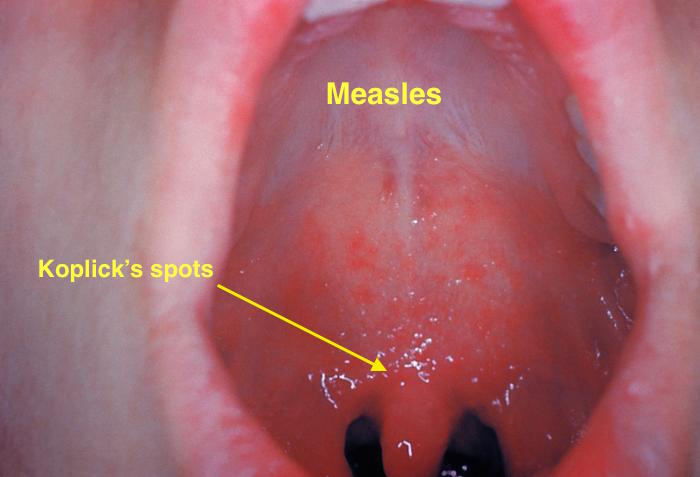
| |
| Herpangina |
|
|
|
|
|
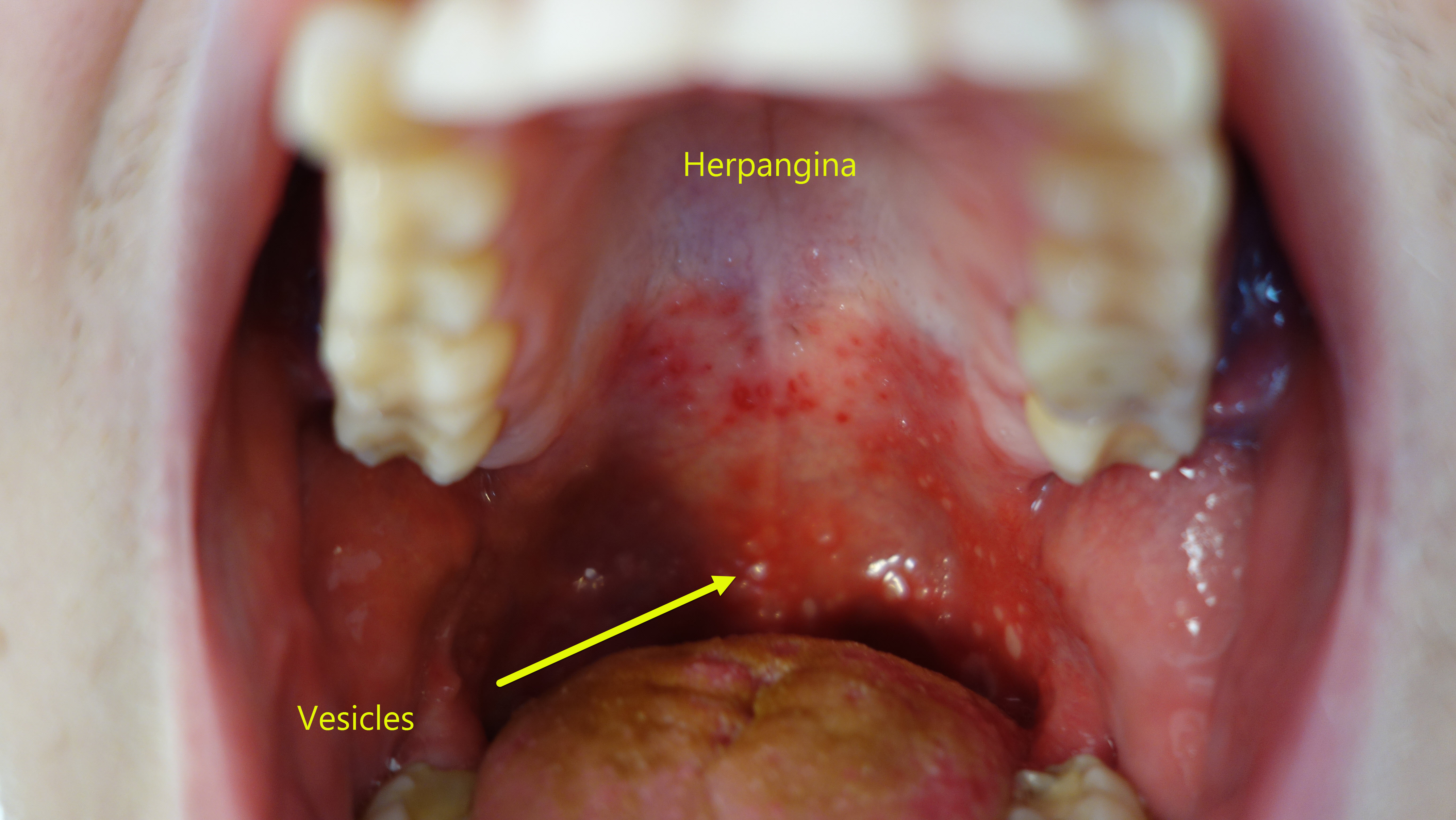 |
| Primary herpetic gingivoestomatitis[20] |
|
|
|
|
|
|
| Oral Candidiasis |
|
|
Localized candidiasis
Invasive candidasis |
|
 |
References
- ↑ Hartman-Adams H, Banvard C, Juckett G (2014). "Impetigo: diagnosis and treatment". Am Fam Physician. 90 (4): 229–35. PMID 25250996.
- ↑ Mehta N, Chen KK, Kroumpouzos G (2016). "Skin disease in pregnancy: The approach of the obstetric medicine physician". Clin Dermatol. 34 (3): 320–6. doi:10.1016/j.clindermatol.2016.02.003. PMID 27265069.
- ↑ Moore, Zack S; Seward, Jane F; Lane, J Michael (2006). "Smallpox". The Lancet. 367 (9508): 425–435. doi:10.1016/S0140-6736(06)68143-9. ISSN 0140-6736.
- ↑ Ibrahim F, Khan T, Pujalte GG (2015). "Bacterial Skin Infections". Prim Care. 42 (4): 485–99. doi:10.1016/j.pop.2015.08.001. PMID 26612370.
- ↑ Ramoni S, Boneschi V, Cusini M (2016). "Syphilis as "the great imitator": a case of impetiginoid syphiloderm". Int J Dermatol. 55 (3): e162–3. doi:10.1111/ijd.13072. PMID 26566601.
- ↑ Kimura U, Yokoyama K, Hiruma M, Kano R, Takamori K, Suga Y (2015). "Tinea faciei caused by Trichophyton mentagrophytes (molecular type Arthroderma benhamiae ) mimics impetigo : a case report and literature review of cases in Japan". Med Mycol J. 56 (1): E1–5. doi:10.3314/mmj.56.E1. PMID 25855021.
- ↑ CEDEF (2012). "[Item 87--Mucocutaneous bacterial infections]". Ann Dermatol Venereol. 139 (11 Suppl): A32–9. doi:10.1016/j.annder.2012.01.002. PMID 23176858.
- ↑ Gerstner ER, Batchelor TT (2010). "Primary central nervous system lymphoma". Arch. Neurol. 67 (3): 291–7. doi:10.1001/archneurol.2010.3. PMID 20212226.
- ↑ von Reyn CF, Kimambo S, Mtei L, Arbeit RD, Maro I, Bakari M, Matee M, Lahey T, Adams LV, Black W, Mackenzie T, Lyimo J, Tvaroha S, Waddell R, Kreiswirth B, Horsburgh CR, Pallangyo K (2011). "Disseminated tuberculosis in human immunodeficiency virus infection: ineffective immunity, polyclonal disease and high mortality". Int. J. Tuberc. Lung Dis. 15 (8): 1087–92. doi:10.5588/ijtld.10.0517. PMID 21740673.
- ↑ Latgé JP (1999). "Aspergillus fumigatus and aspergillosis". Clin. Microbiol. Rev. 12 (2): 310–50. PMC 88920. PMID 10194462.
- ↑ Rassi A, Rassi A, Marin-Neto JA (2010). "Chagas disease". Lancet. 375 (9723): 1388–402. doi:10.1016/S0140-6736(10)60061-X. PMID 20399979.
- ↑ Emery VC (2001). "Investigation of CMV disease in immunocompromised patients". J. Clin. Pathol. 54 (2): 84–8. PMC 1731357. PMID 11215290.
- ↑ Bustamante CI, Wade JC (1991). "Herpes simplex virus infection in the immunocompromised cancer patient". J. Clin. Oncol. 9 (10): 1903–15. doi:10.1200/JCO.1991.9.10.1903. PMID 1919640.
- ↑ Hambleton S (2005). "Chickenpox". Curr. Opin. Infect. Dis. 18 (3): 235–40. PMID 15864101.
- ↑ Alvis Miranda H, Castellar-Leones SM, Elzain MA, Moscote-Salazar LR (2013). "Brain abscess: Current management". J Neurosci Rural Pract. 4 (Suppl 1): S67–81. doi:10.4103/0976-3147.116472. PMC 3808066. PMID 24174804.
- ↑ Patel K, Clifford DB (2014). "Bacterial brain abscess". Neurohospitalist. 4 (4): 196–204. doi:10.1177/1941874414540684. PMC 4212419. PMID 25360205.
- ↑ Tan CS, Koralnik IJ (2010). "Progressive multifocal leukoencephalopathy and other disorders caused by JC virus: clinical features and pathogenesis". Lancet Neurol. 9 (4): 425–37. doi:10.1016/S1474-4422(10)70040-5. PMC 2880524. PMID 20298966.
- ↑ Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE (2000). "Individual and community risks of measles and pertussis associated with personal exemptions to immunization". JAMA. 284 (24): 3145–50. PMID 11135778.
- ↑ Ratnam S, West R, Gadag V, Williams B, Oates E (1996). "Immunity against measles in school-aged children: implications for measles revaccination strategies". Can J Public Health. 87 (6): 407–10. PMID 9009400.
- ↑ Kolokotronis, A.; Doumas, S. (2006). "Herpes simplex virus infection, with particular reference to the progression and complications of primary herpetic gingivostomatitis". Clinical Microbiology and Infection. 12 (3): 202–211. doi:10.1111/j.1469-0691.2005.01336.x. ISSN 1198-743X.
- ↑ Chauvin PJ, Ajar AH (2002). "Acute herpetic gingivostomatitis in adults: a review of 13 cases, including diagnosis and management". J Can Dent Assoc. 68 (4): 247–51. PMID 12626280.
