Bone fracture: Difference between revisions
No edit summary |
m (Bot: Automated text replacement (-{{SIB}} + & -{{EH}} + & -{{EJ}} + & -{{Editor Help}} + & -{{Editor Join}} +)) |
||
| Line 129: | Line 129: | ||
{{Fractures}} | {{Fractures}} | ||
Revision as of 23:05, 8 August 2012
For patient information click here
| Bone fracture | |
 | |
|---|---|
| Internal and external views of an arm with a compound fracture, both before and after surgery | |
| ICD-10 | T14.2 |
| ICD-9 | 829 |
| DiseasesDB | 4939 |
| MeSH | D050723 |
|
WikiDoc Resources for Bone fracture |
|
Articles |
|---|
|
Most recent articles on Bone fracture Most cited articles on Bone fracture |
|
Media |
|
Powerpoint slides on Bone fracture |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Bone fracture at Clinical Trials.gov Trial results on Bone fracture Clinical Trials on Bone fracture at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Bone fracture NICE Guidance on Bone fracture
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Bone fracture Discussion groups on Bone fracture Patient Handouts on Bone fracture Directions to Hospitals Treating Bone fracture Risk calculators and risk factors for Bone fracture
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Bone fracture |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
A bone fracture is a medical condition in which a bone is cracked or broken. While many fractures are the result of high force impact or stress, bone fracture can also occur as a result of certain medical conditions that weaken the bones, such as osteoporosis, certain types of cancer or osteogenesis imperfecta.
Any type of bone break is a fracture. The word break is not used in a formal orthopaedic terminology.
In orthopedic medicine, fractures are classified as closed or open (compound) and simple or multi-fragmentary (formerly comminuted).
- Closed fractures are those in which the skin is intact, while open (compound) fractures involve wounds that communicate with the fracture and may expose bone to contamination. Open injuries carry an elevated risk of infection; they require antibiotic treatment and usually urgent surgical treatment (debridement). This involves removal of all dirt, contamination, and dead tissue.
- Simple fractures are fractures that only occur along one line, splitting the bone into two pieces, while multi-fragmentary fractures involve the bone splitting into multiple pieces. A simple, closed fracture is much easier to treat and has a much better prognosis than an open, contaminated fracture. Other considerations in fracture care are displacement (fracture gap) and angulation. If angulation or displacement is large, reduction (manipulation) of the bone may be required and, in adults, frequently requires surgical care. These injuries may take longer to heal than injuries without displacement or angulation.
Another type of bone fracture is a compression fracture. An example of a compression fracture is when the front portion of a vertebra in the spine collapses due to osteoporosis, a medical condition which causes bones to become brittle and susceptible to fracture (with or without trauma).
Other types of fracture are:
- Complete Fracture- A fracture in which bone fragments separate completely.
- Incomplete Fracture- A fracture in which the bone fragments are still partially joined.
- Linear Fracture- A fracture that is parallel to the bone's long axis.
- Transverse Fracture- A fracture that is at a right angle to the bone's long axis.
- Oblique Fracture- A fracture that is diagonal to a bone's long axis.
- Compression Fracture-A fracture that usually occurs in the vertebrae.
- Spiral Fracture- A fracture where at least one part of the bone has been twisted.
- Comminuted Fracture- A fracture causing many fragments.
- Compacted Fracture- A fracture caused when bone fragments are driven into each other
- Open Fracture- A fracture when the bone reaches the skin
OTA classification
The Orthopaedic Trauma Association, an association for Orthopaedic surgeons, devised an elaborate classification system to describe the injury accurately and guide treatment.[1][2] There are five parts to the code:
- Bone: Description of a fracture starts by naming the bone
- Location: the part of the bone involved (e.g. shaft of the femur).
- 1) proximal
- 2) diaphyseal
- 3) distal
- Type: It is important to note whether the fracture is simple or multifragmentary and whether it is closed or open.
- A=simple fracture
- B=wedge fracture
- C=complex fracture
- Group: The geometry of the fracture is also described by terms such as transverse, oblique, spiral, or segmental.
- Subgroup: Other features of the fracture are described in terms of displacement, angulation and shortening. A stable fracture is one which is likely to stay in a good (functional) position while it heals; an unstable one is likely to shorten, angulate or rotate before healing and lead to poor function in the long term.
Other classification systems
There are other systems used to classify different types of bone fractures:
Bone healing
The natural process of healing a fracture starts when the injured bone and surrounding tissues bleed. The blood coagulates to form a blood clot situated between the broken fragments. Within a few days blood vessels grow into the jelly-like matrix of the blood clot. The new blood vessels bring white blood cells to the area, which gradually remove the non-viable material. The blood vessels also bring fibroblasts in the walls of the vessels and these multiply and produce collagen fibres. In this way the blood clot is replaced by a matrix of collagen. Collagen's rubbery consistency allows bone fragments to move only a small amount unless severe or persistent force is applied.
At this stage, some of the fibroblasts begin to lay down bone matrix (calcium hydroxyapatite) in the form of insoluble crystals. This mineralization of the collagen matrix stiffens it and transforms it into bone. In fact, bone is a mineralized collagen matrix; if the mineral is dissolved out of bone, it becomes rubbery. Healing bone callus is on average sufficiently mineralized to show up on X-ray within 6 weeks in adults and less in children. This initial "woven" bone does not have the strong mechanical properties of mature bone. By a process of remodeling, the woven bone is replaced by mature "lamellar" bone. The whole process can take up to 18 months, but in adults the strength of the healing bone is usually 80% of normal by 3 months after the injury.
Several factors can help or hinder the bone healing process. For example, any form of nicotine hinders the process of bone healing, and adequate nutrition (including calcium intake) will help the bone healing process. Weight-bearing stress on bone, after the bone has healed sufficiently to bear the weight, also builds bone strength.
-
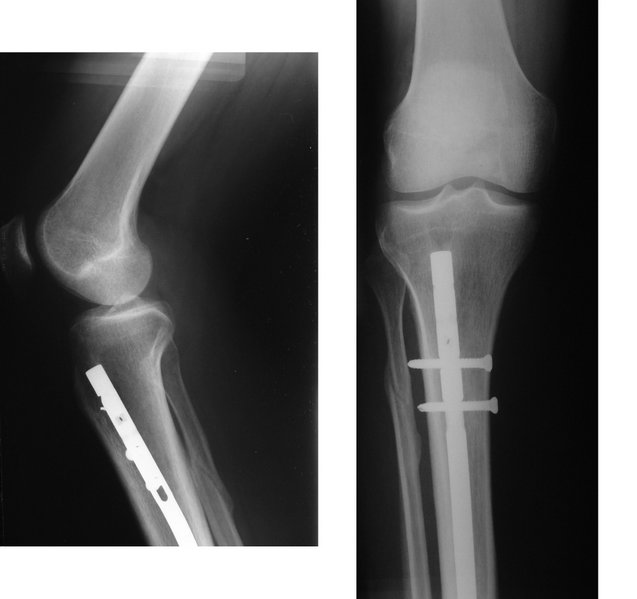
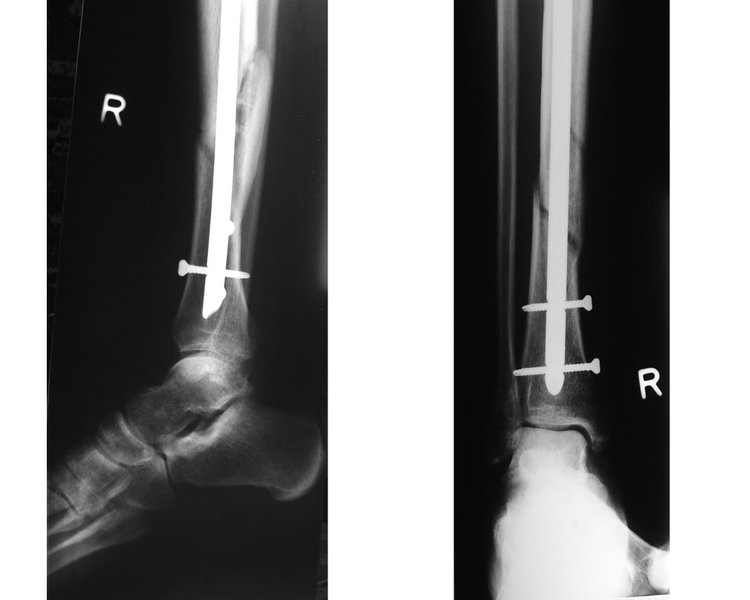
X-ray showing a healed tibia fracture with pins.
-
X-ray showing fractured tibia and pinning.
Treatment
First aid for fractures includes stabilizing the break with a splint in order to prevent movement of the injured part, which could sever blood vessels and cause further tissue damage. Waxed cardboard splints are inexpensive, lightweight, waterproof and strong. Compound fractures are treated as open wounds in addition to fractures.
At the hospital, closed fractures are diagnosed by taking an X-ray photograph of the injury.
Since bone healing is a natural process which will most often occur, fracture treatment aims to ensure the best possible function of the injured part after healing. Bone fractures are typically treated by restoring the fractured pieces of bone to their natural positions (if necessary), and maintaining those positions while the bone heals. To put them back into the natural positions, the doctor often "snaps" the bones back into place. This process is extremely painful without anesthesia, about as painful as breaking the bone itself. To this end, a fractured limb is usually immobilized with a plaster or fiberglass cast which holds the bones in position and immobilizes the joints above and below the fracture. If being treated with surgery, surgical nails, screws, plates and wires are used to hold the fractured bone together more directly. Alternatively, fractured bones may be treated by the Ilizarov method which is a form of external fixator.
Occasionally smaller bones, such as toes, may be treated without the cast, by buddy wrapping them, which serves a similar function to making a cast. By allowing only limited movement, fixation helps preserve anatomical alignment while enabling callus formation, towards the target of achieving union.
Surgical methods of treating fractures have their own risks and benefits, but usually surgery is done only if conservative treatment has failed or is very likely to fail. With some fractures such as hip fractures (usually caused by osteoporosis or Osteogenesis Imperfecta), surgery is offered routinely, because the complications of non-operative treatment include deep vein thrombosis (DVT) and pulmonary embolism, which are more dangerous than surgery. When a joint surface is damaged by a fracture, surgery is also commonly recommended to make an accurate anatomical reduction and restore the smoothness of the joint.
Infection is especially dangerous in bones, due to their limited blood flow. Bone tissue is predominantly extracellular matrix, rather than living cells, and the few blood vessels needed to support this low metabolism are only able to bring a limited number of immune cells to an injury to fight infection. For this reason, open fractures and osteotomies call for very careful antiseptic procedures and prophylactic antibiotics.
Sometimes bones are reinforced with metal, but these fracture implants must be designed and installed with care. Stress shielding occurs when plates or screws carry too large of a portion of the bone's load, causing atrophy. This problem is reduced, but not eliminated, by the use of low-modulus materials, including titanium and its alloys. The heat generated by the friction of installing hardware can easily accumulate and damage bone tissue, reducing the strength of the connections. If dissimilar metals are installed in contact with one another (i.e., a titanium plate with cobalt-chromium alloy or stainless steel screws), galvanic corrosion will result. The metal ions produced can damage the bone locally and may cause systemic effects as well.
In children
In children, whose bones are still developing, there are risks of either a growth plate injury or a greenstick fracture.
- A greenstick fracture occurs because the bone is not as brittle as it would be in an adult, and thus does not completely fracture, but rather exhibits bowing without complete disruption of the bone's cortex.
- Growth plate injuries, as in Salter-Harris fractures, require careful treatment and accurate reduction to make sure that the bone continues to grow normally.
- Plastic deformation of the bone, in which the bone permanently bends but does not break, is also possible in children. These injuries may require an osteotomy (bone cut) to realign the bone if it is fixed and cannot be realigned by closed methods.
See also
References
- ↑ "Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification" (pdf). J Orthop Trauma. 10 Suppl 1: v–ix, 1–154. 1996. PMID 8814583. Retrieved 2007-11-28.
- ↑ "Orthopaedic Trauma Association/ Committee for Coding and Classification: Fracture and Dislocation Compendium". Orthopaedic Trauma Association. Retrieved 2007-11-28.
- ↑ Mourad L (1997). "Neer classification of fractures of the proximal humerus". Orthop Nurs. 16 (2): 76. PMID 9155417.
- ↑ "eMedicine - Proximal Humerus Fractures : Article by Mark Frankle, MD". Retrieved 2007-12-15.
- ↑ Template:GPnotebook
- ↑ "Seinsheimer's Classification of Subtrochanteric Frxs - Wheeless' Textbook of Orthopaedics". Retrieved 2007-12-15.
ar:كسر عظم ca:Fractura (medicina) de:Knochenbruch el:Κάταγμα eo:Frakturo (medicino) gl:Fractura ko:골절 it:Frattura (medicina) he:שבר (רפואה) lt:Kaulo lūžimas nl:Botbreuk no:Beinbrudd qu:Tullup'aki sk:Zlomenina kosti fi:Luunmurtuma sv:Fraktur (medicin) uk:Переломи кісток