COVID-19-associated acute respiratory distress syndrome
|
COVID-19 Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
COVID-19-associated acute respiratory distress syndrome On the Web |
|
American Roentgen Ray Society Images of COVID-19-associated acute respiratory distress syndrome |
|
FDA on COVID-19-associated acute respiratory distress syndrome |
|
CDC on COVID-19-associated acute respiratory distress syndrome |
|
COVID-19-associated acute respiratory distress syndrome in the news |
|
Blogs on COVID-19-associated acute respiratory distress syndrome |
|
Risk calculators and risk factors for COVID-19-associated acute respiratory distress syndrome |
For COVID-19 frequently asked inpatient questions, click here
For COVID-19 frequently asked outpatient questions, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ayesha Javid, MBBS[2] Usman Ali Akbar, M.B.B.S.[3]
Overview
ARDS has been distributed over different phenotypes over the last decade. The management of COVID-19 related ARDS has been therefore led to a different proposal for the management strategies that are stratified according to the type of phenotype. ARDS developed in 20 percent a median of eight days after the onset of symptoms; mechanical ventilation was implemented in 12.3 percent. The mortality rate of COVID-19 related ARDS is higher in elderly patients. Given the importance of heterogeneity of the ARDS profile, appropriate intervention at an appropriate time is needed to help to prevent the deterioration of lung function. Recent advances in RECOVERY trial has further strengthened this notion that the use of dexamethasone in patients on a ventilator can reduce the mortality rate of patients by 1/3rd. The treatment of COVID-19 related ARDS is evolving with time and different treatment options are now available for the better management of ARDS.
Historical Perspective
- In 2002–2003, the novel coronavirus was named as the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) due to its high similarity to SARS-CoV, which caused acute respiratory distress syndrome (ARDS).
- SARS-CoV-2 virus primarily affects the respiratory system causing a wide variety of respiratory symptoms which can range from symptoms of lower respiratory tract infection to severe hypoxia to acute respiratory distress syndrome within a very short span of time.
- The acute respiratory distress syndrome (ARDS) is a common cause of morbidity and mortality in critically ill COVID-19 infected patients. It is defined by the acute onset of noncardiogenic pulmonary edema, hypoxemia and the need for mechanical ventilation.
Classification
Several authors in a case report highlighted the nonuniformity of patients with COVID-19-associated ARDS and proposed the existence of two primary phenotypes:
- Type L (low values of elastance, pulmonary ventilation/ perfusion ratio, lung weight, and recruitability).
- Type H (high values of elastance, right-to-left shunt, lung weight, and recruitability), more consistent with typical severe ARDS.
Pathophysiology
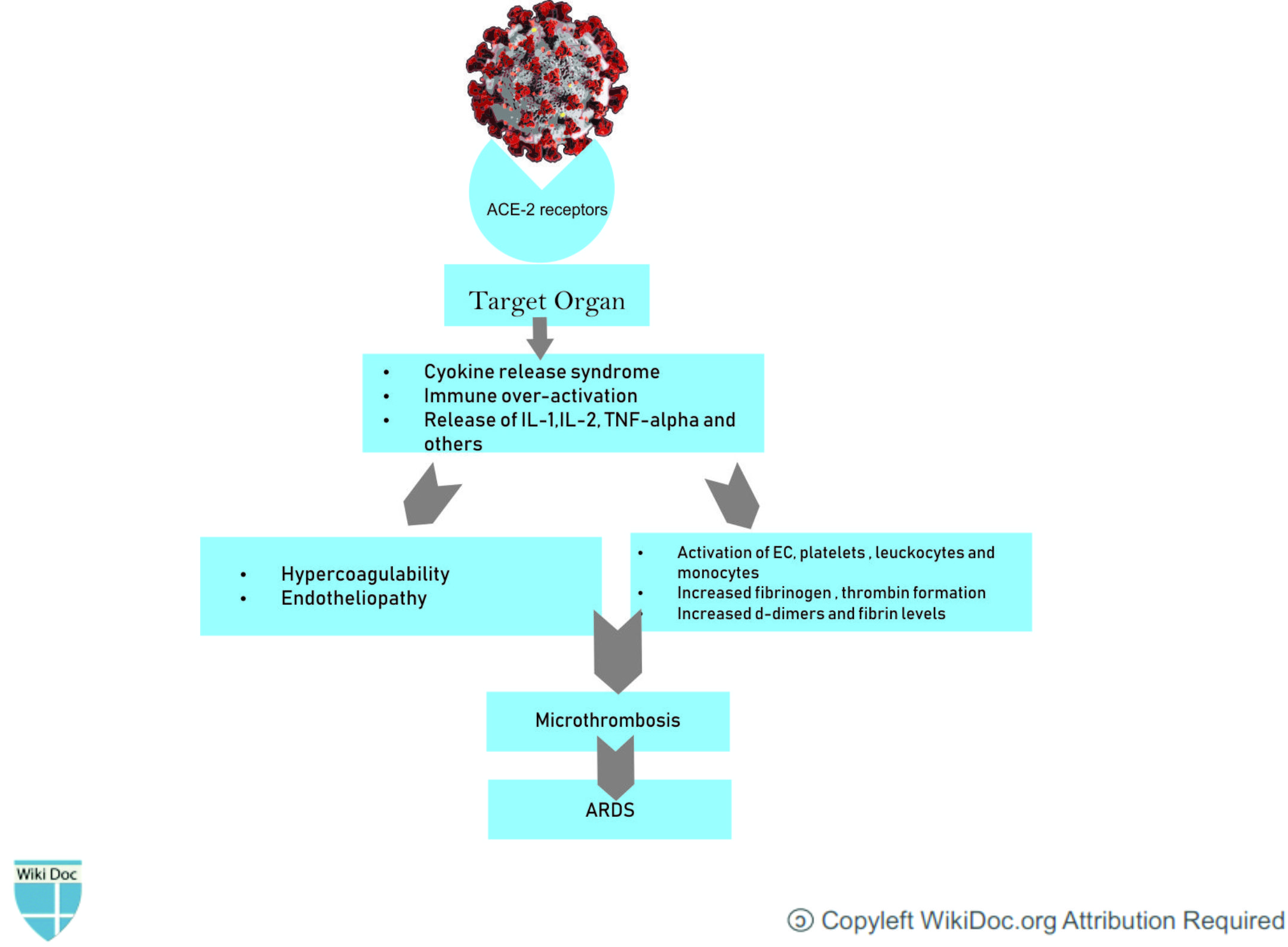
- ARDS arises as a complication of COVID-19 infection due to acute inflammation of the alveolar space which prevents normal gas exchange. The increase in proinflammatory cytokines within the lung leads to recruitment of leukocytes, further propagating the local inflammatory response.
- The cytokine storm and the deadly uncontrolled systemic inflammatory response resulting from the release of large amounts of proinflammatory cytokines including interferons and interleukins and, chemokines by immune effector cells resulting in acute inflammation within the alveolar space. The exudate containing plasma proteins, including albumin, fibrinogen, proinflammatory cytokines and coagulation factors will increase alveolar-capillary permeability and decrease the normal gas exchange and plasma proteins, including albumin, fibrinogen, proinflammatory cytokines and coagulation factors.
- The COVID-19 patients with ARDS show elevated levels of IL-6, IFN-a, and CCL5, CXCL8, CXCL-10 in serum as compared to those with the mild to moderate disease.
- This inflammatory process leads to the fibrin deposition in the air spaces and lung parenchyma and contributes to hyaline-membrane formation and subsequent alveolar fibrosis.
- Patients infected with COVID‐19 also exhibit coagulation abnormalities.This procoagulant pattern can lead to acute respiratory distress syndrome.
Clinical Features
- Clinical presentations of COVID-19 range from asymptomatic (81.4%), through mildly symptomatic with or without seasonal flu-like symptoms, to severe pneumonia (13.9%).
- Respiratory problems manifest as dyspnea that ranges from effort dyspnea to dyspnea occurring at rest.
- Patients with dyspnea can revert to an asymptomatic phase or progress to ARDS, requiring positive pressure oxygen therapy and intensive care therapy [18] in 17–19.6% of symptomatic patients.
Differentiating COVID-associated ARDS from other Diseases
COVID-19 associated ARDS must be differentiated from other diseases that also cause ARDS by the following parameters:
- Positive SARS-CoV-2 infection on PCR
- COVID-19 ARDS causes the typical ARDS pathological changes of diffuse alveolar damage in the lung.
- As patients move through the course of their illness, the longer term outcomes of ARDS are being reported, with lung fibrosis appearing as part of COVID-19 ARDS.
- Pulmonary thrombosis is also associated with COVID-19 related ARDS.
- Deaths from COVID-19 associated ARDS have been reported due to thrombotic disseminated intravascular coagulation.
Epidemiology and Demographics
| Date of publication | Country | Author | Total Number of patients | Prevalence |
|---|---|---|---|---|
| January 24,2020 | China | Huang C et al. | 41 | 29.26 %
(16.13-45.53) |
| January 29,2020 | China | Nanshan Chen et al.[1] | 99 |
17.17 %
(10.33-26.06) |
| March 13, 2020 | China | Chaomin Wu et al. | 201 | 41.8 % |
| May 14, 2020 | Multiple | Zhang et al. | 4203 | 18.4% |
Age
- Patients of all age groups may develop ARDS.
- It is more commonly observed among patients aged ≥65 years years old.
Gender
- Some case studies report that men are more commonly affected by ARDS than women.
- In the public data set, the number of men who died from COVID-19 is 2.4 times that of women (70.3 vs. 29.7%, P = 0.016).
Race
- A large study in the United States reported that that African Americans were at a higher risk of ARDS than white individuals.
Risk Factors
- In a retrospective study conducted in China, following risk factors were the main predisposing factors for the development of ARDS:
- Older age (≥65 years old)
- High fever (≥39 °C)
- Comorbidities (eg, hypertension, diabetes)
- Neutrophilia
- Lymphocytopenia (as well as lower CD3 and CD4 T-cell counts)
- Elevated end-organ related indices (eg, AST, urea, LDH)
- Elevated inflammation-related indices (high-sensitivity C-reactive protein and serum ferritin)
- Elevated coagulation function–related indicators (PT and D-dimer)
Natural History, Complications and Prognosis
Natural History
The natural history of ARDS is hallmarked by three histopathological phases—exudative, proliferative, and fibrotic phase—each correlated to distinctive clinical manifestations.
| Exudative Phase | Proliferative Phase | Fibrotic Phase |
|---|---|---|
|
|
|
Complications
Common complications include:
- ARDS is complicated by VAP in approximately 37% to 60% of cases.
- VAP usually develops 5 to 7 days after the initial exposure to the precipitating factor.
- The most likely microorganisms of VAP include non-fermenting Gram-negative bacilli, methicillin-resistant Staphylococcus aureus, and Enterobacteriaceae.
- Barotrauma (e.g., pneumothorax, pneumomediastinum, and subcutaneous emphysema)
- Barotrauma occurs as a consequence of inappropriate positive airway pressure in regions with reduced pulmonary compliance and may complicate ARDS in approximately 10% of cases.
Other complications include:
- Significant weakness due to critical illness myoneuropathy and muscle atrophy as a result of long-term immobilization
- Impaired lung function
- Chronic ventilator dependency due to advanced weakness and atrophy of the muscles of respiration
- Pulmonary fibrosis and restrictive lung disease
- Psychiatric illness, including post-traumatic stress disorder (PTSD), anxiety, and depression
- Impaired cognition
- Persistent vegetative state or brain death due to prolonged hypoxemia
Prognosis
- The survival rate for patients with COVID-19 with ARDS is approximately 25%.
- Factors associated with increased mortality in patients with COVID-19 pneumonia included age ≥65 years, presence of cardiovascular or cerebrovascular disease, lymphopenia, and elevation in troponin I levels.
- Despite major progress in the care of patients with ARDS, survivors are at high risk for cognitive decline, depression, post-traumatic stress disorder, and physical deconditioning.
Diagnosis
Diagnostic Criteria
- COVID-19 ARDS is diagnosed when someone with confirmed COVID-19 infection meets the Berlin 2012 ARDS diagnostic criteria of:
- Acute hypoxemic respiratory failure.
- Presentation within 1 week of worsening respiratory symptoms.
- Bilateral airspace disease on chest x-ray, computed tomography (CT) or ultrasound that is not fully explained by effusions, lobar or lung collapse, or nodules.
- Cardiac failure is not the primary cause of acute hypoxemic respiratory failure.
Symptoms
- Dyspnea: The onset of dyspnea is relatively late around the 6th day.
- Acute Hypoxemia due to respiratory failure is a dominant finding.
- Hypercapnia could be present but it is rare.
Physical Examination
- The physical exam findings of a patient with ARDS vary according to the underlying cause and typically develop within 24 to 48 hours of the precipitating illness or injury and progress over the course of 1 to 2 weeks. However, ARDS related to COVID-19 has sometimes late-onset. Common physical findings include:
Vital Signs
- The presence of the following signs of shock or infection on physical examination are highly suggestive of ARDS:
- Temperature (Temp, T): Hyperpyrexia ≥ 38°C or 100.4°F) or low temperature < 36°C or 96.8°F.
- Blood pressure (BP): inappropriately low, with a low mean arterial pressure (MAP).
- Heart rate (HR): rapid (tachycardia > 100 beats/minute), normal, or slow (bradycardia <60 beats/minute).
- Respiratory rate (RR): Tachypnea > 20 breaths/minute or bradypnea <12 breaths/minute.
- Peripheral capillary oxygen saturation (SpO2): low (< 90% on ambient air or a fraction of inspired oxygen, (FIO2) of 21% at sea level).
Skin
- Cyanosis due to poor oxygenation.
- Pallor due to poor perfusion.
Lungs
- Tachypnea
- Dyspnea
- Coarse breath sounds, rhonchi, crackles, or decreased breath sounds
Heart
- Tachycardia or bradycardia on heart auscultation.
Extremities
- Cyanosis
- Cool extremities or reduced peripheral pulses due to poor perfusion.
Laboratory Findings
- Blood plasma has elevated levels of IL-6, IL-1, tumour necrosis factor-α (TNF α) and C-reactive protein.
- Thrombocytopenia.
- Increased D-dimer levels. The elevated level of D-dimer is strongly associated with a higher mortality rate.
- Increased fibrin degradation products.[2]
- Increased fibrinogen.[2]
- Prothrombin time and activated partial thromboplastin time may be slightly elevated.[2]
Imaging Findings
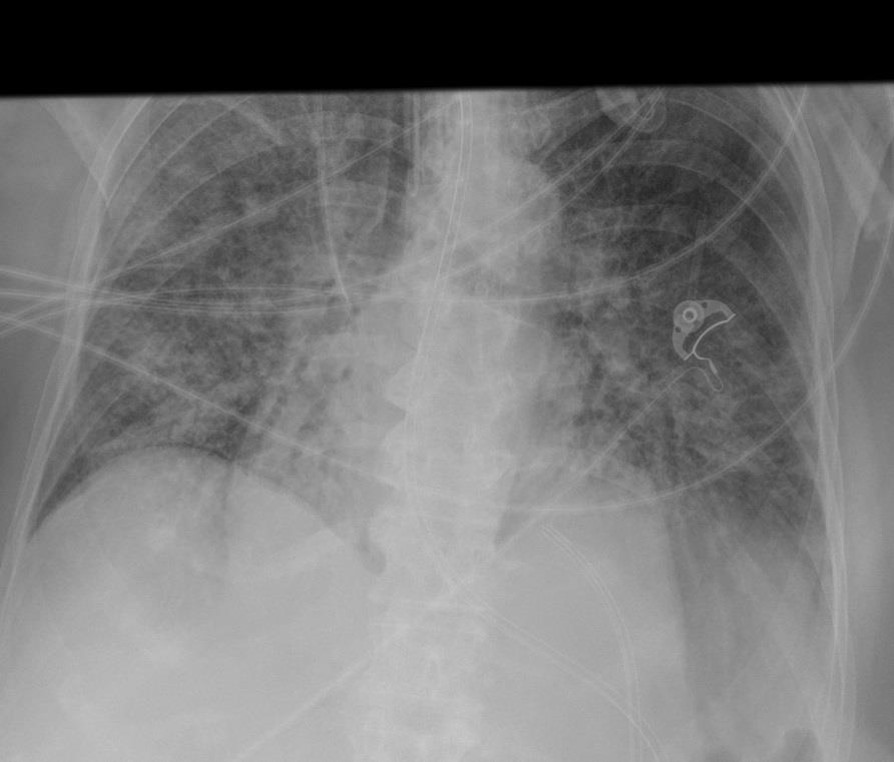
Chest-X ray
On Chest X-ray following findings can be seen.
- Ground-glass opacification and consolidation
- Early findings on the chest radiograph include normal or diffuse alveolar opacities (consolidation), which are often bilateral and which obscure the pulmonary vascular markings.
- Later, these opacities progress to more extensive consolidation that is diffuse, and they are often asymmetrical.
Chest CT-Scan
- Chest CT scan shows characteristic ground-glass opacities (GCO). This indicates the presence of exudate in the bronchoalveolar airspace.[3]
- Lung biopsy shows fibrin deposition.[3]

Treatment
Medical Therapy
Fluid and electrolytes management
- Studies have shown that in ARDS, conservative fluid management may help patients by reducing edema formation.
- Conservative fluid management with buffered or non-buffered crystalloid is recommended for ARDS patients.
- The conservative fluid strategy results in an increased number of ventilator-free days and a decreased length of ICU stay. However, its effect on mortality remains uncertain.
Corticosteroids
- Recent studies have shown that the corticosteroid dexamethasone may reduce mortality of severe COVID-19 patients.
- In England, a non-peer-reviewed randomized trial was issued as a press release which suggested that dexamethasone has a potential survival benefit in hospitalized COVID-19 patients requiring oxygen.
- The Society of Critical Care Medicine (SCCM) provided a weak conditional recommendation in the favor of glucocorticoids in patients with COVID-19 who have severe ARDS with a partial arterial pressure of oxygen/fraction of inspired oxygen PaO2:FiO2] <100 mmHg). This recommendation suggests benefit in patients with moderate to severe ARDS which is refractory to low tidal volume ventilation.
Mechanical Ventilation
- Mechanical ventilation along with supportive therapies are the mainstay of treatment of ARDS.
- Invasive mechanical ventilation (ie, ventilation via an endotracheal tube or tracheostomy with breaths delivered by a mechanical ventilator) is preferred for patients with ARDS, particularly those with moderate or severe ARDS (ie, arterial oxygen tension/fraction of inspired oxygen PaO2/FiO2 ≤200 mmHg on positive end-expiratory pressure (PEEP) ≥5 cm H2O).[4]
- It is recommended to use low tidal volume ventilation (LTVV) with 4 to 8 mL/kg predicted body weight [PBW]. Several meta-analyses and randomized trials that report a mortality benefit from LTVV in patients with ARDS.
- The aim is to maintain oxygen saturation between 90% to 96%. The severe hypoxemia of the COVID-19 ARDS best responds when Positive end-expiratory pressure (PEEP) is high with Pplat ≤30 cm H2O. It is beneficial if the physician starts with higher than usual levels of PEEP (10 to 15 cm H2O).
Anticoagulant or thrombolytic therapy
- Fibrinolytic drugs such as tissue-type plasminogen activator (tPA) degrade pre-existing fibrin in the lungs.[2]
- Nebulizer plasminogen activators may provide more targeted therapy to degrade fibrin and improving oxygenation in critically ill patients. It is in Phase II of the clinical trial.
Prevention
Primary Prevention
- The best way to prevent being infected by COVID-19 is to avoid being exposed to this virus by adopting the following practices for infection control:
- Often wash hands with soap and water for at least 20 seconds.
- Use an alcohol-based hand sanitizer containing at least 60% alcohol in case soap and water are not available.
- Avoid touching the eyes, nose, and mouth without washing hands.
- Avoid being in close contact with people sick with COVID-19 infection.
- Stay home while being symptomatic to prevent spread to others.
- Cover mouth while coughing or sneezing with a tissue paper, and then throw the tissue in the trash.
- Clean and disinfect the objects and surfaces which are touched frequently.
- There is currently no vaccine available to prevent COVID-19.
Secondary Prevention
- The secondary prevention measures of Coronavirus disease 2019 (COVID-19) constitute protective measures to make sure that an infected individual does not transfer the disease to others by maintaining self-isolation at home or designated quarantine facilities.
- The ARDS patients have an increased risk of hospital-associated venous thromboembolism (VTE).
- Due to this reason, it is advised to take low molecular weight heparin (LMWH) prophylactically in patients who do not have the contraindications. Studies have shown that the heparin, either unfractionated or LMWH, can also reduce inflammatory biomarkers hence could help in reducing the inflammation.
References
- ↑ "Redirecting". Page Redirection. Retrieved 2020-07-15.
- ↑ 2.0 2.1 2.2 2.3 Tang N, Li D, Wang X, Sun Z (2020). "Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia". J Thromb Haemost. 18 (4): 844–847. doi:10.1111/jth.14768. PMC 7166509 Check
|pmc=value (help). PMID 32073213 PMID: 32073213 Check|pmid=value (help). - ↑ 3.0 3.1 Whyte CS, Morrow GB, Mitchell JL, Chowdary P, Mutch NJ (2020). "Fibrinolytic abnormalities in acute respiratory distress syndrome (ARDS) and versatility of thrombolytic drugs to treat COVID-19". J Thromb Haemost. doi:10.1111/jth.14872. PMC 7264738 Check
|pmc=value (help). PMID 32329246 PMID: 32329246 Check|pmid=value (help). - ↑ Wang, Dawei; Hu, Bo; Hu, Chang; Zhu, Fangfang; Liu, Xing; Zhang, Jing; Wang, Binbin; Xiang, Hui; Cheng, Zhenshun; Xiong, Yong; Zhao, Yan; Li, Yirong; Wang, Xinghuan; Peng, Zhiyong (2020-03-17). "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China". JAMA. American Medical Association (AMA). 323 (11): 1061. doi:10.1001/jama.2020.1585. ISSN 0098-7484. PMC 7042881 Check
|pmc=value (help). PMID 32031570 Check|pmid=value (help).