COVID-19 interventions
For COVID-19 frequently asked outpatient questions, click here
For COVID-19 frequently asked inpatient questions, click here
|
COVID-19 Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
COVID-19 interventions On the Web |
|
American Roentgen Ray Society Images of COVID-19 interventions |
|
Risk calculators and risk factors for COVID-19 interventions |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Javaria Anwer M.D.[2]
Synonyms and keywords: SARS Cov2 interventions, Interventions in covid19, Novel coronavirus interventions
Overview
The feasibility of the strategy utilized for the management of a patient with COVID-19 depends on the patient's condition at the time of presentation. Continuous evaluation and titration of ongoing interventions ensure optimal results. The respiratory manifestations of COVID-19 may require some oxygen supplementation to ventilatory support. Autopsy findings of patients with COVID-19-associated acute respiratory distress syndrome (CARDS) demonstrated small airway occlusion due to necrosis and inflammation. The finding advocates the use of positive pressure ventilation to restore the collapsed airways. A balanced approach is required as a high end-inspiratory pressure increases the risk of lung alveolar injury. Interventions posing a risk of aerosol transmissions should be carried out following using all the required precautions such as the use of PPE and AIIR room with minimal healthcare personnel in the room.
Ventilatory support in COVID-19
- The feasibility of the strategy utilized for the management of a patient with COVID-19 depends on the patient's condition at the time of presentation. Continuous evaluation and titration of ongoing interventions ensure optimal results. The respiratory manifestations of COVID-19 may require some oxygen supplementation to ventilatory support. Autopsy findings of patients with COVID-19-associated acute respiratory distress syndrome (CARDS) demonstrated small airway occlusion due to necrosis and inflammation. The finding advocates the use of positive pressure ventilation to restore the collapsed airways. A balanced approach is required as a high end-inspiratory pressure increases the risk of lung alveolar injury.[1]
- The COVID-19 respiratory complications that may require mechanical ventilation include: COVID-19-associated pneumonia, COVID-19-associated acute respiratory distress syndrome (CARDS) and COVID-19-associated respiratory failure. At the start, the recommendation to treat CARDS was similar to the ones utilized to treat ARDS due to other causes. During the initial course of the disease, in the absence of bacterial infection in COVID-19-associated pneumonia or CARDS, the patient has normal or even high pulmonary compliance. Thus, a patient can have severe hypoxemia in the absence of tachypnoea or dyspnea. Knowledge and experience of the unique features of the disease have led the guidelines to be modified/ specified.
- Acute hypoxemic respiratory failure and ARDS are more common respiratory complications among COVID-19 patients.[2]
Supplemental Oxygen
- A patient with L type (low lung elastance and V/Q ratio) of COVID-19-associated pneumonia or CARDS benefit from increased FiO2 the most. The therapy is particularly useful if the patient is non-dyspneic.[3]
- Among COVID-19 positive adult patients the Surviving Sepsis Campaign (SSC) strongly recommends (with moderate-quality evidence):[2]
- To start the supplemental oxygen if the Spo2 is < 90%. Starting the supplemental oxygen at < 92% saturation has weak recommendation.
- Maintain Spo2 no higher than 96% among patients with with acute hypoxemic respiratory failure on supplemental oxygen therapy. The recommendation is based upon the systematic review and meta-analysis of 25 RCTs that showed a linear association between the death risk and higher Spo2 targets.
Non-Invasive ventilation (NIV)
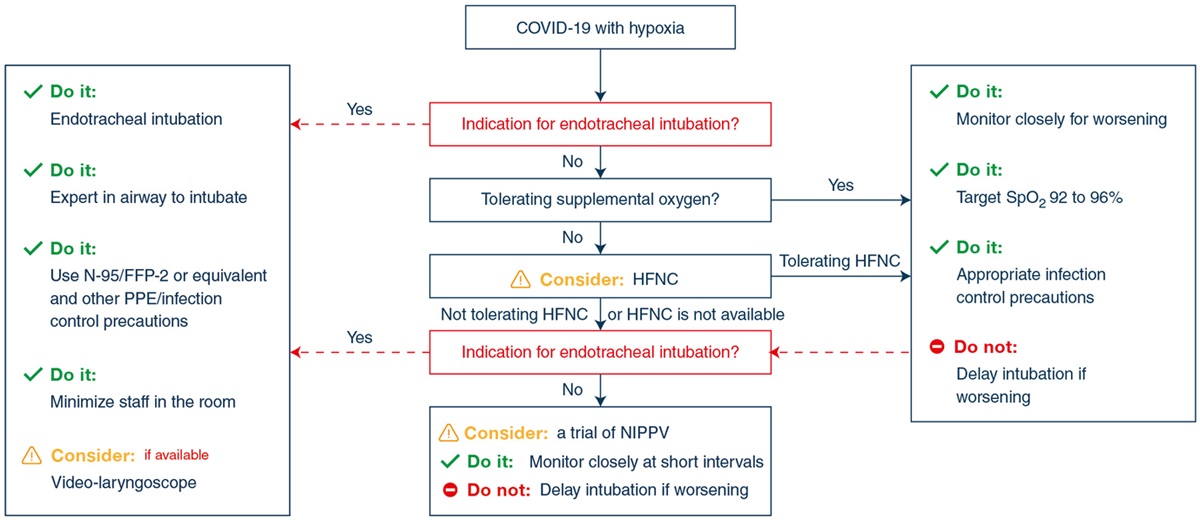
- NIV methods are easier and comfortable to use and work by inducing PEEP thus decreased the respiratory workload. Based on the COVID-19 experience of the Chinese experts , both HFNC and NIPPV methods should probably be utilized among patients with PaO2/FiO2 > 150 mmHg.[1]
- Close monitoring for a deteriorating respiratory status and early intubation when indicated in a controlled setting, can help minimize the infection of health personnel and promise better patient health outcomes.[2]
- Inspiratory pressures should be 10 cmH2O and expiratory pressures be 5 cmH2O with 1.0 FiO2.[4]
High Flow Nasal Cannula (HFNC)
- Also known as high flow nasal oxygen (HFNO) or Heated humidified high-flow (HHHF) therapy is a non-invasive technique. It is a technique of delivering heated and humidified high-flow oxygen via soft and flexible nasal prongs. Humidification prevents the drying of epithelium and facilitates the removal of mucosal secretions. Other advantages include pharyngeal dead space washout and PEEP effect.[5] A hypercapnic patient should not be administered HFNC.
- Sufficient evidence to prove the superiority of one of the methods (HFNC or NIPPV) is lacking. But HFNC is preferred over Non-invasive positive pressure ventilation (NIPPV). It is possibly due to reduced mortality and decreased intubation risk, as proved by a RCT and a meta-analysis respectively. Patient comfort better oxygenation with HFNC than NIPPV is also one of the considering factors.[1][6]
- In acute hypoxemic respiratory failure despite supplemental oxygen therapy, SSC suggests using HFNC over conventional oxygen therapy (weak recommendation). A systematic review and meta-analysis of 9 RCTs showed that High Flow Nasal Cannula (HFNC) reduces the need for intubation.[2]
- Target SpO2 should be 88% -94% with minimal flow rates under 30L/min. Low flow rates help minimize aerosolization. PEEP ranges from 5-15 and peak airway pressure ranges from 8-10 cmH2O.[4]
Non-Invasive Positive Pressure Ventilation (NIPPV)
- Non-invasive positive pressure ventilation (NIPPV) is a technique utilized for delivering mechanical ventilation without the use of endotracheal intubation or tracheostomy. It can be administered through a face mask, nasal mask, or a helmet and includes CPAP and BiPAP.
- Numerous patients who develop ARDS were administered a trial of non-invasive positive pressure ventilation (NIPPV) before intubation for mechanical ventilation before they clinically deteriorate or become unable to maintain adequate oxygenation. Studies from China reported (4% to 13%) of COVID-19 patients to have administered NIPPV.[2]
- Among adults with COVID-19 and hypoxemic respiratory failure, if HFNC is not available and endotracheal intubation not urgently indicated, a trial of NIPPV can be administered. Type L patients with dyspnea can benefit from NIV.[3] Close monitoring and short-interval assessment for worsening of respiratory failure is required. (weak recommendation by SSC).[2]
- The safety and efficacy of helmet NIPPV among COVID-19 patients is questionable. One study advocates the use of helmet NIPPV in COVID-19 care due to potential avoidance of air dispersion through the spring-valve.[7] Having said that, the cost of a helmet may be an essential consideration for healthcare systems struggling financially.
Invasive Mechanical Ventilation (IMV)
- The vascular endothelial injury in COVID-19-associated acute respiratory distress syndrome (CARDS) and diverse mortality rates across the world among CARDS patients arbitrates the importance of different mechanical ventilation strategies.
- The Chinese CDC reports the case-fatality rate to be higher than 50% among patients who were administered invasive mechanical ventilation.[8]
- According to the American Society of Anesthesiology based upon the experience of Chinese anesthesiologists, timely (neither premature nor late) intubation and ventilation are the most effectual breathing assistance.[9] Early intubation may prevent the transition from type L (low elastance and V/Q ratio) to (high elastance and V/Q ratio) phenotype of CARDS.[3]
Intubation
According to American Heart Association (AHA), intubation is indicated in:
- Gas exchange abnormality: Respiratory failure (usually hypoxic in COVID-19), PaO2/FiO2 <150 (corrected for altitude), NIV with FiO2 >0.6 and inability to maintain SpO2 >90%, unresponsiveness to HFNC therapy, hypercapnia (PaCO2 > 45 mm Hg) with acidosis (PH< 7.3), increased work of breathing with deteriorating respiratory function.
- Airway protection: Altered mental status and neurological dysfunctions.
- Pulmonary toilet: To remove excessive pulmonary secretions.
Ventilator settings
The following ventilator setting should be utilized:[10][11][12]
- Mode: No mode of ventilation has been suggested to be superior to others. AHA recommends assist control PRVC.
- Respiratory rate: 20-25 breaths/min.
- Tidal volume (Vt): 4–8 ml/kg predicted body weight and lower inspiratory pressures. Excess Vt is associated with alveolar overdistension and worse CARDS.
- Plateau pressure (Pplat): <30 cm H2O and peak inspiratory pressure:<35 cmH2O.
- FiO2: <0.6
- Positive end-expiratory pressure (PEEP): Based upon the data of 8 RCTs on ARDS, mean ± SD PEEP was 15.1 ± 3.6 cm H2O (higher) versus 9.1 ± 2.7 cm H2O (lower). Patients receiving higher PEEP had better oxygenation (PaO2/FiO2). It is recommended that moderate or severe CARDS patients administered higher levels of PEEP.[12]
- Titration for CARDS: Following lung recruitment maneuvers, PEEP can be titrated down from a maximum of 20 cm H2O until the goals of oxygenation, plateau pressure, and compliance are all achieved. In Wuhan, COID-19 patients with acute hypoxemic respiratory failure showed a poor tolerance to high PEEP, possibly due to the severe lung damage by the SARS-CoV-2 virus and inflammatory reactions. The PEEP should be reduced to 8–10 cmH2O in prone positioning ventilation. [3][10] The CARDS Ventilator PEEP Titration Protocol can be viewed by clicking here.
- Types: Patients with “H type” (high elastance and V/Q ratio) CARDS, may benefit from higher PEEP and lower tidal volumes. Patients with “L type” (low lung elastance and V/Q ratio) CARDS may benefit from lower PEEP and higher tidal volumes.[13] If Type L patient is hypercapnic, volumes greater than 6 ml/kg (up to 8–9 ml/kg) can be helpful.
- Contraindications for the use of the PEEP may include untreated pneumothorax, very low blood pressure, elevated ICP, and pulmonary hypertension.
- Complications of PEEP may include barotrauma, such as pneumothorax and/or decreased cardiac output. CARDS patients on high PEEP had no associated complications or increased mortality.[12]
- Maintenance Goals: pH= 7.25-7.42, paO2 >60/ SpO2= 88-96%, paCO2= 40-65/ETCO= 35-60 mmHg (permissive hypercapnia).
Extracorporeal membrane oxygenation (ECMO)
- Venovenous type of ECMO (VV ECMO) drains blood from a large central vein, oxygenates it, and removes carbon dioxide via the gas-exchange device. The blood is then reinfused. ECMO can help avoid ventilator-induced lung injury.
- The use of ECMO is has been recommended among COVID-19 patients with refractory hypoxemia or high driving pressure, or hypercapnia/respiratory acidosis despite invasive mechanical ventilation (IMV) and lung-protective measures such as higher PEEP or prone positioning. The strategies can be combined such as among Type H patients, who should be treated as severe ARDS patients with higher PEEP, if compatible with hemodynamics, prone positioning and ECMO.[3][14][1] The WHO suggested referring patients with refractory hypoxemia despite lung-protective ventilation to the settings with expertise in ECMO.[15]
- It is not known whether ECMO reduces mortality but 6.2% patients were treated with ECMO in Wuhan, China.[16][17] A definitive recommendation requires additional evidence for or against the use of ECMO among patients with CARDS.[12]
Strategies to improve oxygenation
Prone position ventilation
- Prone positioning is thought to improve oxygenation by improving ventilation/perfusion (V/Q) mismatching via reduced shunting of blood through under-ventilated lung tissue.
- Prone position ventilation among ARDS patients with acute hypoxemic respiratory failure and spontaneous or assisted breathing reduces the mortality by 28 and 90-days.[18]
- The strategy was widely used among COVID-19 patients in Wuhan, China.[10]
- Prone position is an early strategy rather than a desperate rescue therapy.[19] A study by Lin Ding et al. suggests that the early application of prone ventilation with HFNC and NIV, especially in COVID-19 patients with moderate ARDS, can help avoid intubation.[20] Prone position, with other adjunct therapies may probably be administered for critically ill patients even during ECMO.[1]
- Prone position for awake patients during spontaneous or assisted breathing during NIPPV or HFNC with mild-moderate ARDS was associated with an improved oxygenation.[21] In addition, patients with an Spo2 of 95% or greater following an hour of the prone position had a lower rate of intubation.[22] To answer the question regarding the effectiveness, two RCTs are in progress NCT04347941 and NCT04350723.[19]
- The American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice and SSC guidelines strongly recommend (moderate evidence) Prone positioning for greater than 12 hours/day among patients with severe ARDS. Among mechanically ventilated patients with PaO2/FiO2 <150, prone positioning can be utilized.[14][12][23]
{{#ev:youtube|https://www.youtube.com/watch?v=lcBPaHQUvXY}}
Special considerations
- Lung recruitment maneuvers[10][24][25]: Lung recruitment maneuver is the application of very high (up to 40 cm H2O) positive airway pressure during mechanical ventilation. It opens the collapsed alveoli, decreasing ventilation/perfusion (V/Q) mismatching thus improving the gas exchange. For ARDS patients, the maneuvers may help improve oxygenation and decrease the length of hospital stay with no positive effect on reducing mortality. The decision varies on a case by case basis depending upon lung condition and patient hemodynamics. On the trouble side, the maneuver may generate aerosols. High-quality evidence is lacking to support the use in ARDS patients.
- Paralytics:[26][27] The paralytics may be administered with analgesics (fentanyl, hydromorphone) and sedatives (benzodiazepines, propofol). Among CARDS patients, Richmond Agitation Sedation Scale (RASS) score of (+2 to +4) even following optimal ventilatory settings may indicate the use of deep sedation with paralytics. If administered, short-term (24– 48 hours) and intermittent muscle relaxation is recommended. Prone position ventilation may also require muscle relaxation along with sedation. Paralytics are not recommended unless PaO2/FiO2 < 150 mmHg. The paralytics that are being administered among CARDS patients include: Succinylcholine chloride injection USP 200 mg/10 mL and cisatracurium besylate injection USP 20 mg/10 mL.
- Aerosol Generation Risk Factors and Protective Measures: Concerns have been raised for a possible risk for transmission of COVID-19 to health care personnel due to aerosol transmission.[28] With the judicious use of the standard precautions and protective measures, the results for the mentioned interventions have been promising.
| Source of aerosol generation | Protective Measures |
|---|---|
| Coughing |
|
| Face Mask Seal Leak |
|
| Non-Invasive ventilation, bronchoscopy, CPR extubation, and manual ventilation |
|
| Intubation |
|
| Tracheostomy |
|
Bronchoscopy
- Very limited studies are available on the use of bronchoscopy among COVID-19 patients due to a very high risk of aerosol transmission. Bronchoscopy as a well-tolerated therapeutic intervention, performed among mechanically ventilated patients with COVID-19 have been reported in an observational study. FiO2 was increased to SpO2 95%–98% before the intervention. Precautions such as the use of a negative-pressure room, PPE, and duration of the procedure never greater than 10 minutes were observed. The study showed that patients can benefit from therapeutic bronchoscopy for the removal of thick hyper-secretions in the airway (most common complication observed). Guided mini-BAL can also help confirm the clinical suspicion of superinfection. [34]
- In addition to the above-mentioned precautions (table) recommended by CDC and WHO for the use of PPE, eye protection and AIIR room for the procedure, using disposable bronchoscope if possible is also advised. It is important to clean the suction channels with the cleaning solutions utilized for highly infectious materials.[30]
Tracheostomy
- Standard decision making for tracheostomy in a COVID patient is practiced. But owing to the potential of aerosol spread of the infection certain considerations should be kept in mind, such as the safety of other the patient's family, other patients, healthcare personnel, and the resources available.[35]
- Tracheostomy should be delayed until at least the 10th day of mechanical ventilation. It should be considered only when the patient is clinically improving. The decision of extubation should be limited to the patients who have a high chance of success.[33]
Cardiopulmonary resuscitation (CPR)
American Heart Association's (AHA) interim BLS Healthcare Provider Adult Cardiac Arrest Algorithm for Suspected or Confirmed COVID-19 Patients can be accessed by clicking here.[36]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Shang Y, Pan C, Yang X, Zhong M, Shang X, Wu Z, Yu Z, Zhang W, Zhong Q, Zheng X, Sang L, Jiang L, Zhang J, Xiong W, Liu J, Chen D (June 2020). "Management of critically ill patients with COVID-19 in ICU: statement from front-line intensive care experts in Wuhan, China". Ann Intensive Care. 10 (1): 73. doi:10.1186/s13613-020-00689-1. PMC 7275657 Check
|pmc=value (help). PMID 32506258 Check|pmid=value (help). - ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Alhazzani, Waleed; Møller, Morten Hylander; Arabi, Yaseen M.; Loeb, Mark; Gong, Michelle Ng; Fan, Eddy; Oczkowski, Simon; Levy, Mitchell M.; Derde, Lennie; Dzierba, Amy; Du, Bin; Aboodi, Michael; Wunsch, Hannah; Cecconi, Maurizio; Koh, Younsuck; Chertow, Daniel S.; Maitland, Kathryn; Alshamsi, Fayez; Belley-Cote, Emilie; Greco, Massimiliano; Laundy, Matthew; Morgan, Jill S.; Kesecioglu, Jozef; McGeer, Allison; Mermel, Leonard; Mammen, Manoj J.; Alexander, Paul E.; Arrington, Amy; Centofanti, John E.; Citerio, Giuseppe; Baw, Bandar; Memish, Ziad A.; Hammond, Naomi; Hayden, Frederick G.; Evans, Laura; Rhodes, Andrew (2020). "Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19)". Critical Care Medicine. 48 (6): e440–e469. doi:10.1097/CCM.0000000000004363. ISSN 0090-3493.
- ↑ 3.0 3.1 3.2 3.3 3.4 Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, Camporota L (June 2020). "COVID-19 pneumonia: different respiratory treatments for different phenotypes?". Intensive Care Med. 46 (6): 1099–1102. doi:10.1007/s00134-020-06033-2. PMC 7154064 Check
|pmc=value (help). PMID 32291463 Check|pmid=value (help). - ↑ 4.0 4.1 "Oxygenation and Ventilation of COVID 19 Patients | American Heart Association CPR & First Aid".
- ↑ Zhang J, Lin L, Pan K, Zhou J, Huang X (December 2016). "High-flow nasal cannula therapy for adult patients". J. Int. Med. Res. 44 (6): 1200–1211. doi:10.1177/0300060516664621. PMC 5536739. PMID 27698207.
- ↑ Frat, Jean-Pierre; Thille, Arnaud W.; Mercat, Alain; Girault, Christophe; Ragot, Stéphanie; Perbet, Sébastien; Prat, Gwénael; Boulain, Thierry; Morawiec, Elise; Cottereau, Alice; Devaquet, Jérôme; Nseir, Saad; Razazi, Keyvan; Mira, Jean-Paul; Argaud, Laurent; Chakarian, Jean-Charles; Ricard, Jean-Damien; Wittebole, Xavier; Chevalier, Stéphanie; Herbland, Alexandre; Fartoukh, Muriel; Constantin, Jean-Michel; Tonnelier, Jean-Marie; Pierrot, Marc; Mathonnet, Armelle; Béduneau, Gaëtan; Delétage-Métreau, Céline; Richard, Jean-Christophe M.; Brochard, Laurent; Robert, René (2015). "High-Flow Oxygen through Nasal Cannula in Acute Hypoxemic Respiratory Failure". New England Journal of Medicine. 372 (23): 2185–2196. doi:10.1056/NEJMoa1503326. ISSN 0028-4793.
- ↑ Cabrini L, Landoni G, Zangrillo A (February 2020). "Minimise nosocomial spread of 2019-nCoV when treating acute respiratory failure". Lancet. 395 (10225): 685. doi:10.1016/S0140-6736(20)30359-7. PMC 7137083 Check
|pmc=value (help). PMID 32059800 Check|pmid=value (help). - ↑ Wu, Zunyou; McGoogan, Jennifer M. (2020). "Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China". JAMA. 323 (13): 1239. doi:10.1001/jama.2020.2648. ISSN 0098-7484.
- ↑ 10.0 10.1 10.2 10.3 10.4 Meng, Lingzhong; Qiu, Haibo; Wan, Li; Ai, Yuhang; Xue, Zhanggang; Guo, Qulian; Deshpande, Ranjit; Zhang, Lina; Meng, Jie; Tong, Chuanyao; Liu, Hong; Xiong, Lize (2020). "Intubation and Ventilation amid the COVID-19 Outbreak". Anesthesiology. 132 (6): 1317–1332. doi:10.1097/ALN.0000000000003296. ISSN 0003-3022.
- ↑ "NHLBI ARDS Network | Tools".
- ↑ 12.0 12.1 12.2 12.3 12.4 Fan, Eddy; Del Sorbo, Lorenzo; Goligher, Ewan C.; Hodgson, Carol L.; Munshi, Laveena; Walkey, Allan J.; Adhikari, Neill K. J.; Amato, Marcelo B. P.; Branson, Richard; Brower, Roy G.; Ferguson, Niall D.; Gajic, Ognjen; Gattinoni, Luciano; Hess, Dean; Mancebo, Jordi; Meade, Maureen O.; McAuley, Daniel F.; Pesenti, Antonio; Ranieri, V. Marco; Rubenfeld, Gordon D.; Rubin, Eileen; Seckel, Maureen; Slutsky, Arthur S.; Talmor, Daniel; Thompson, B. Taylor; Wunsch, Hannah; Uleryk, Elizabeth; Brozek, Jan; Brochard, Laurent J. (2017). "An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: Mechanical Ventilation in Adult Patients with Acute Respiratory Distress Syndrome". American Journal of Respiratory and Critical Care Medicine. 195 (9): 1253–1263. doi:10.1164/rccm.201703-0548ST. ISSN 1073-449X.
- ↑ Marini, John J.; Gattinoni, Luciano (2020). "Management of COVID-19 Respiratory Distress". JAMA. 323 (22): 2329. doi:10.1001/jama.2020.6825. ISSN 0098-7484.
- ↑ 14.0 14.1 Fan E, Beitler JR, Brochard L, Calfee CS, Ferguson ND, Slutsky AS, Brodie D (July 2020). "COVID-19-associated acute respiratory distress syndrome: is a different approach to management warranted?". Lancet Respir Med. doi:10.1016/S2213-2600(20)30304-0. PMC 7338016 Check
|pmc=value (help). PMID 32645311 Check|pmid=value (help). - ↑ "Clinical management of COVID-19".
- ↑ Zeng, Yingchun; Cai, Zhongxiang; Xianyu, Yunyan; Yang, Bing Xiang; Song, Ting; Yan, Qiaoyuan (2020). "Prognosis when using extracorporeal membrane oxygenation (ECMO) for critically ill COVID-19 patients in China: a retrospective case series". Critical Care. 24 (1). doi:10.1186/s13054-020-2840-8. ISSN 1364-8535.
- ↑ Li, Chenglong; Hou, Xiaotong; Tong, Zhaohui; Qiu, Haibo; Li, Yimin; Li, Ang (2020). "Extracorporeal membrane oxygenation programs for COVID-19 in China". Critical Care. 24 (1). doi:10.1186/s13054-020-03047-6. ISSN 1364-8535.
- ↑ Xie H, Zhou ZG, Jin W, Yuan CB, Du J, Lu J, Wang RL (2018). "Ventilator management for acute respiratory distress syndrome associated with avian influenza A (H7N9) virus infection: A case series". World J Emerg Med. 9 (2): 118–124. doi:10.5847/wjem.j.1920-8642.2018.02.006. PMC 5847497. PMID 29576824.
- ↑ 19.0 19.1 Telias, Irene; Katira, Bhushan H.; Brochard, Laurent (2020). "Is the Prone Position Helpful During Spontaneous Breathing in Patients With COVID-19?". JAMA. 323 (22): 2265. doi:10.1001/jama.2020.8539. ISSN 0098-7484.
- ↑ Ding L, Wang L, Ma W, He H (January 2020). "Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi-center prospective cohort study". Crit Care. 24 (1): 28. doi:10.1186/s13054-020-2738-5. PMC 6993481 Check
|pmc=value (help). PMID 32000806 Check|pmid=value (help). - ↑ Sartini, Chiara; Tresoldi, Moreno; Scarpellini, Paolo; Tettamanti, Andrea; Carcò, Francesco; Landoni, Giovanni; Zangrillo, Alberto (2020). "Respiratory Parameters in Patients With COVID-19 After Using Noninvasive Ventilation in the Prone Position Outside the Intensive Care Unit". JAMA. 323 (22): 2338. doi:10.1001/jama.2020.7861. ISSN 0098-7484.
- ↑ Thompson, Alison E.; Ranard, Benjamin L.; Wei, Ying; Jelic, Sanja (2020). "Prone Positioning in Awake, Nonintubated Patients With COVID-19 Hypoxemic Respiratory Failure". JAMA Internal Medicine. doi:10.1001/jamainternmed.2020.3030. ISSN 2168-6106.
- ↑ Rhodes, Andrew; Evans, Laura E.; Alhazzani, Waleed; Levy, Mitchell M.; Antonelli, Massimo; Ferrer, Ricard; Kumar, Anand; Sevransky, Jonathan E.; Sprung, Charles L.; Nunnally, Mark E.; Rochwerg, Bram; Rubenfeld, Gordon D.; Angus, Derek C.; Annane, Djillali; Beale, Richard J.; Bellinghan, Geoffrey J.; Bernard, Gordon R.; Chiche, Jean-Daniel; Coopersmith, Craig; De Backer, Daniel P.; French, Craig J.; Fujishima, Seitaro; Gerlach, Herwig; Hidalgo, Jorge Luis; Hollenberg, Steven M.; Jones, Alan E.; Karnad, Dilip R.; Kleinpell, Ruth M.; Koh, Younsuk; Lisboa, Thiago Costa; Machado, Flavia R.; Marini, John J.; Marshall, John C.; Mazuski, John E.; McIntyre, Lauralyn A.; McLean, Anthony S.; Mehta, Sangeeta; Moreno, Rui P.; Myburgh, John; Navalesi, Paolo; Nishida, Osamu; Osborn, Tiffany M.; Perner, Anders; Plunkett, Colleen M.; Ranieri, Marco; Schorr, Christa A.; Seckel, Maureen A.; Seymour, Christopher W.; Shieh, Lisa; Shukri, Khalid A.; Simpson, Steven Q.; Singer, Mervyn; Thompson, B. Taylor; Townsend, Sean R.; Van der Poll, Thomas; Vincent, Jean-Louis; Wiersinga, W. Joost; Zimmerman, Janice L.; Dellinger, R. Phillip (2017). "Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016". Intensive Care Medicine. 43 (3): 304–377. doi:10.1007/s00134-017-4683-6. ISSN 0342-4642.
- ↑ Cui, Yu; Cao, Rong; Wang, Yu; Li, Gen (2020). "Lung Recruitment Maneuvers for ARDS Patients: A Systematic Review and Meta-Analysis". Respiration. 99 (3): 264–276. doi:10.1159/000501045. ISSN 0025-7931.
- ↑ Hodgson C, Goligher EC, Young ME, Keating JL, Holland AE, Romero L, Bradley SJ, Tuxen D (November 2016). "Recruitment manoeuvres for adults with acute respiratory distress syndrome receiving mechanical ventilation". Cochrane Database Syst Rev. 11: CD006667. doi:10.1002/14651858.CD006667.pub3. PMC 6464835. PMID 27855477.
- ↑ Payen JF, Chanques G, Futier E, Velly L, Jaber S, Constantin JM (June 2020). "Sedation for critically ill patients with COVID-19: Which specificities? One size does not fit all". Anaesth Crit Care Pain Med. 39 (3): 341–343. doi:10.1016/j.accpm.2020.04.010. PMC 7189860 Check
|pmc=value (help). PMID 32360979 Check|pmid=value (help). - ↑ Schünemann HJ, Khabsa J, Solo K, Khamis AM, Brignardello-Petersen R, El-Harakeh A, Darzi A, Hajizadeh A, Bognanni A, Bak A, Izcovich A, Cuello-Garcia CA, Chen C, Borowiack E, Chamseddine F, Schünemann F, Morgano GP, Muti-Schünemann G, Chen G, Zhao H, Neumann I, Brozek J, Schmidt J, Hneiny L, Harrison L, Reinap M, Junek M, Santesso N, El-Khoury R, Thomas R, Nieuwlaat R, Stalteri R, Yaacoub S, Lotfi T, Baldeh T, Piggott T, Zhang Y, Saad Z, Rochwerg B, Perri D, Fan E, Stehling F, Akl IB, Loeb M, Garner P, Aston S, Alhazzani W, Szczeklik W, Chu DK, Akl EA (May 2020). "Ventilation Techniques and Risk for Transmission of Coronavirus Disease, Including COVID-19: A Living Systematic Review of Multiple Streams of Evidence". Ann. Intern. Med. doi:10.7326/M20-2306. PMC 7281716 Check
|pmc=value (help). PMID 32442035 Check|pmid=value (help). Vancouver style error: initials (help) - ↑ 29.0 29.1 29.2 "apps.who.int" (PDF).
- ↑ Hatipoglu Z, Turktan M, Avci A (November 2016). "The anesthesia of trachea and bronchus surgery". J Thorac Dis. 8 (11): 3442–3451. doi:10.21037/jtd.2016.11.35. PMC 5179431. PMID 28066625.
- ↑ "Transmission-Based Precautions | Basics | Infection Control | CDC"".
- ↑ 33.0 33.1 McGrath, Brendan A; Brenner, Michael J; Warrillow, Stephen J; Pandian, Vinciya; Arora, Asit; Cameron, Tanis S; Añon, José Manuel; Hernández Martínez, Gonzalo; Truog, Robert D; Block, Susan D; Lui, Grace C Y; McDonald, Christine; Rassekh, Christopher H; Atkins, Joshua; Qiang, Li; Vergez, Sébastien; Dulguerov, Pavel; Zenk, Johannes; Antonelli, Massimo; Pelosi, Paolo; Walsh, Brian K; Ward, Erin; Shang, You; Gasparini, Stefano; Donati, Abele; Singer, Mervyn; Openshaw, Peter J M; Tolley, Neil; Markel, Howard; Feller-Kopman, David J (2020). "Tracheostomy in the COVID-19 era: global and multidisciplinary guidance". The Lancet Respiratory Medicine. 8 (7): 717–725. doi:10.1016/S2213-2600(20)30230-7. ISSN 2213-2600.
- ↑ Torrego A, Pajares V, Fernández-Arias C, Vera P, Mancebo J (July 2020). "Bronchoscopy in Patients with COVID-19 with Invasive Mechanical Ventilation: A Single-Center Experience". Am. J. Respir. Crit. Care Med. 202 (2): 284–287. doi:10.1164/rccm.202004-0945LE. PMC 7365381 Check
|pmc=value (help). PMID 32412787 Check|pmid=value (help). - ↑ Zhang, Xiaomeng; Huang, Qiling; Niu, Xun; Zhou, Tao; Xie, Zhen; Zhong, Yi; Xiao, Hongjun (2020). "Safe and effective management of tracheostomy in
COVID
‐19 patients". Head & Neck. 42 (7): 1374–1381. doi:10.1002/hed.26261. ISSN 1043-3074. line feed character in
|title=at position 49 (help)