COVID-19-associated arrhythmia and conduction system disease: Difference between revisions
| (195 intermediate revisions by the same user not shown) | |||
| Line 4: | Line 4: | ||
'''For COVID-19 frequently asked inpatient questions, click [[COVID-19 frequently asked inpatient questions|here]]'''<br> | '''For COVID-19 frequently asked inpatient questions, click [[COVID-19 frequently asked inpatient questions|here]]'''<br> | ||
'''For COVID-19 frequently asked outpatient questions, click [[COVID-19 frequently asked outpatient questions|here]]'''<br> | '''For COVID-19 frequently asked outpatient questions, click [[COVID-19 frequently asked outpatient questions|here]]'''<br> | ||
{{CMG}} {{AE}} {{TAM}} | {{CMG}} {{AE}} {{Sara.Zand}} {{TAM}} | ||
{{SK}}[[COVID-19-associated arrhythmia and conduction system disease|COVID-19-associated dysrhythmia]] | {{SK}}[[COVID-19-associated arrhythmia and conduction system disease|COVID-19-associated dysrhythmia]] | ||
==Overview== | ==Overview== | ||
[[Sever acute respiratory syndrome coronavirus-2]] ([[SARS-COV-2]]) is the [[virus]] that causes [[coronavirus disease 2019]] may affect every [[organ]] system including the [[heart]]. [[Arrhythmia]] is a disorder of [[conduction]] system including [[atrial arrhythmia]], [[ventricular arrhythmia]], [[bradyarrhythmia]] , resulting from direct effect of [[virus]] by attaching viral [[spike protein]] to [[ACE2]] receptors on [[myocardium]] and inducing [[myocardial injury]] and conduction damage system or indirect effect of [[covid-19]] such as coexisting [[hypoxia]], [[electrolytes]] disarray, and the administration of [[arrhythmogenic]] [[medications]] ([[hydroxychloroquine]], [[azithromycin]]). Reported case about new onset [[atrial fibrillation]] in [[covid-19]] [[infection]] may indicate the [[atrial arrhythmogenicity]] of [[covid-19]] [[infection]]. In the presence of [[covid-19]], approperiate approach to life threatening [[arrhythmia]] and considering [[fulminant myocarditis]] are warranted. High number of out-of hospital [[cardiac arrest]] in Italy during the 40 first days of initiation of pandemic, raised the concerns about the risk of [[arrhythmia]] in [[covid-19]]. [[Incidence]] of [[arrhythmia]] in [[ICU]] admitted [[covid-19]] [[patients]] increased to 10 folds. [[Cardiac ]] [[arrhythmia]] was associated with increased [[mortality]] and [[morbidity]] in [[hospitalized]] [[covid-19]] [[patients]]. | |||
[[ | |||
==Historical Perspective== | ==Historical Perspective== | ||
| Line 22: | Line 18: | ||
==Classification== | ==Classification== | ||
* [[Arrhythmia]] | * [[Arrhythmia]] related to [[COVID-19]] may be classified into [[atrial arrhythmia]] (81.8%), [[ventricular arrhythmia]] (21%), [[bradyarrhythmia]] (22.6%) as follows: | ||
* [[Atrial fibrillation]] | * [[Atrial fibrillation]] | ||
* [[Atrial flutter]] | * [[Atrial flutter]] | ||
* [[Supraventricular tachycardia]] | * [[Supraventricular tachycardia]] | ||
* [[ | * Nonsustained [[ventricular tachycardia]] | ||
* [[Ventricular tachycardia]] | * [[Ventricular tachycardia]] | ||
* [[Ventricular fibrillation]] | * [[Ventricular fibrillation]] | ||
* [[Atrioventricular block]] | * [[Atrioventricular block]] | ||
* Marked [[sinus bradycardia]] ([[heart rate]]<40 [[bpm]]) | * Marked [[sinus bradycardia]] ([[heart rate]]<40 [[bpm]]) | ||
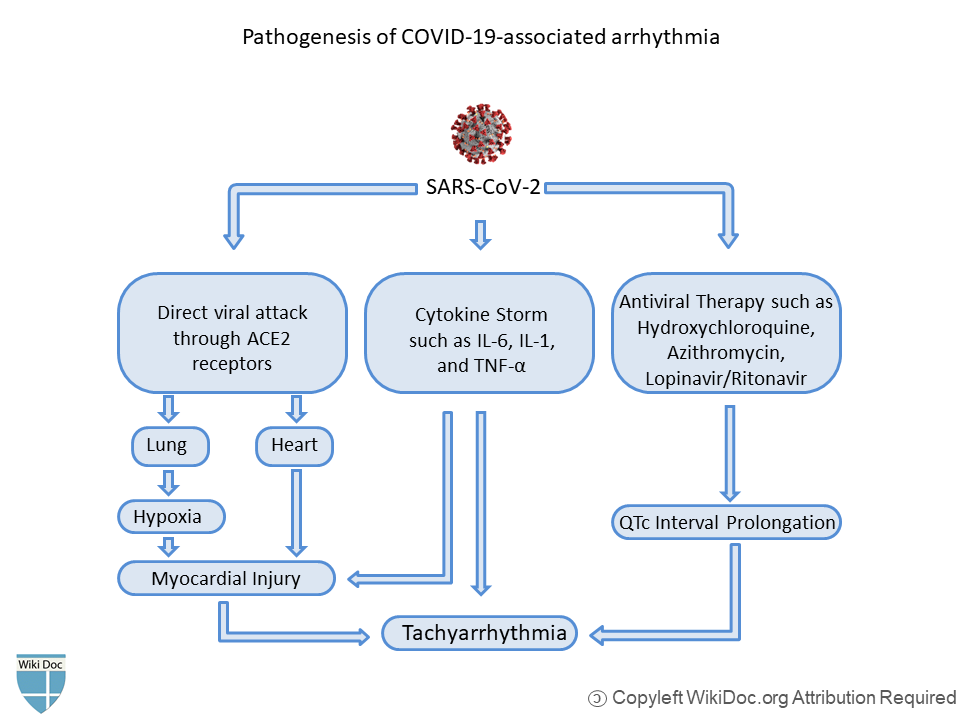
==Pathophysiology== | ==Pathophysiology== | ||
| Line 54: | Line 35: | ||
* The interaction between [[SARS-CoV-2]] and ACE2 can bring about changes in [[Angiotensin-converting enzyme 2|ACE2]] pathways prompting intense injury to the lung, heart, and [[Endothelium|endothelial cells]]. | * The interaction between [[SARS-CoV-2]] and ACE2 can bring about changes in [[Angiotensin-converting enzyme 2|ACE2]] pathways prompting intense injury to the lung, heart, and [[Endothelium|endothelial cells]]. | ||
*[[Hypoxemia|Hypoxia]] and [[Electrolyte disturbance|electrolyte abnormalities]] that are common in the acute phase of severe [[COVID-19]] can potentiate [[Cardiac arrhythmia|cardiac arrhythmias]]. | *[[Hypoxemia|Hypoxia]] and [[Electrolyte disturbance|electrolyte abnormalities]] that are common in the acute phase of severe [[COVID-19]] can potentiate [[Cardiac arrhythmia|cardiac arrhythmias]]. | ||
* Binding of [[SARS-CoV-2]] to ACE2 receptors can result in [[hypokalemia]] which causes various types of [[Cardiac arrhythmia|arrhythmia]]. | * Binding of [[SARS-CoV-2]] to [[ACE2]] receptors can result in [[hypokalemia]] which causes various types of [[Cardiac arrhythmia|arrhythmia]]. | ||
* Elevated levels of [[Cytokine|cytokines]] as a result of the [[Systemic inflammatory response syndrome|systemic inflammatory response]] of the severe [[COVID-19|Coronavirus disease 2019]] (COVID-19) can cause injury to multiple organs, including [[Cardiac muscle|cardiac myocytes]].<ref name="ChenPrendergast2020">{{cite journal|last1=Chen|first1=Mao|last2=Prendergast|first2=Bernard|last3=Redwood|first3=Simon|last4=Xiong|first4=Tian-Yuan|title=Coronaviruses and the cardiovascular system: acute and long-term implications|journal=European Heart Journal|volume=41|issue=19|year=2020|pages=1798–1800|issn=0195-668X|doi=10.1093/eurheartj/ehaa231}}</ref> | * Elevated levels of [[Cytokine|cytokines]] as a result of the [[Systemic inflammatory response syndrome|systemic inflammatory response]] of the severe [[COVID-19|Coronavirus disease 2019]] (COVID-19) can cause injury to multiple organs, including [[Cardiac muscle|cardiac myocytes]].<ref name="ChenPrendergast2020">{{cite journal|last1=Chen|first1=Mao|last2=Prendergast|first2=Bernard|last3=Redwood|first3=Simon|last4=Xiong|first4=Tian-Yuan|title=Coronaviruses and the cardiovascular system: acute and long-term implications|journal=European Heart Journal|volume=41|issue=19|year=2020|pages=1798–1800|issn=0195-668X|doi=10.1093/eurheartj/ehaa231}}</ref> | ||
*In COVID-19 patients, excessive ranges of circulating [[Cytokine|cytokines]], especially interleukin [[Interleukin 6|(IL)-6]] is related to in-hospital death.<ref name="pmid32201335">{{cite journal| author=Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G | display-authors=etal| title=Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic. | journal=J Am Coll Cardiol | year= 2020 | volume= 75 | issue= 18 | pages= 2352-2371 | pmid=32201335 | doi=10.1016/j.jacc.2020.03.031 | pmc=7198856 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32201335 }} </ref> | *In [[COVID-19]] [[patients]], excessive ranges of circulating [[Cytokine|cytokines]], especially [[interleukin]] [[Interleukin 6|(IL)-6]] is related to in-hospital death.<ref name="pmid32201335">{{cite journal| author=Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G | display-authors=etal| title=Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic. | journal=J Am Coll Cardiol | year= 2020 | volume= 75 | issue= 18 | pages= 2352-2371 | pmid=32201335 | doi=10.1016/j.jacc.2020.03.031 | pmc=7198856 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32201335 }} </ref> | ||
* As a result of cytokine storm triggered by | * As a result of [[cytokine storm]] triggered by [[SARS-CoV-2]] that includes IL-6, [[tumor necrosis factor]] (TNF) α, and IL-1, duration of [[ventricular ]] [[action potential]] can be prolonged. | ||
*Studies suggest that cytokine storm can modulate the function of cardiomyocyte ion channels such as Na+, K+ and Ca+ channels (inflammatory cardiac channelopathies).<ref name="pmid30552387">{{cite journal| author=Lazzerini PE, Laghi-Pasini F, Boutjdir M, Capecchi PL| title=Cardioimmunology of arrhythmias: the role of autoimmune and inflammatory cardiac channelopathies. | journal=Nat Rev Immunol | year= 2019 | volume= 19 | issue= 1 | pages= 63-64 | pmid=30552387 | doi=10.1038/s41577-018-0098-z | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30552387 }} </ref> | *Studies suggest that [[cytokine storm]] can modulate the function of [[cardiomyocyte]] [[ion channels]] such as Na+, K+ and Ca+ channels ([[inflammatory]] [[cardiac channelopathies]]).<ref name="pmid30552387">{{cite journal| author=Lazzerini PE, Laghi-Pasini F, Boutjdir M, Capecchi PL| title=Cardioimmunology of arrhythmias: the role of autoimmune and inflammatory cardiac channelopathies. | journal=Nat Rev Immunol | year= 2019 | volume= 19 | issue= 1 | pages= 63-64 | pmid=30552387 | doi=10.1038/s41577-018-0098-z | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30552387 }} </ref> | ||
* According to the data based on studies on previous [[Severe acute respiratory syndrome]] ([[Severe acute respiratory syndrome|SARS]]) and the [[Middle East respiratory syndrome coronavirus infection|Middle East respiratory syndrome]] ([[Middle East respiratory syndrome coronavirus infection|MERS]]) epidemic and the ongoing [[COVID-19]] outbreak, multiple mechanisms have been suggested for cardiac damage.<ref name="ClerkinFried2020">{{cite journal|last1=Clerkin|first1=Kevin J.|last2=Fried|first2=Justin A.|last3=Raikhelkar|first3=Jayant|last4=Sayer|first4=Gabriel|last5=Griffin|first5=Jan M.|last6=Masoumi|first6=Amirali|last7=Jain|first7=Sneha S.|last8=Burkhoff|first8=Daniel|last9=Kumaraiah|first9=Deepa|last10=Rabbani|first10=LeRoy|last11=Schwartz|first11=Allan|last12=Uriel|first12=Nir|title=COVID-19 and Cardiovascular Disease|journal=Circulation|volume=141|issue=20|year=2020|pages=1648–1655|issn=0009-7322|doi=10.1161/CIRCULATIONAHA.120.046941}}</ref> | * According to the data based on studies on previous [[Severe acute respiratory syndrome]] ([[Severe acute respiratory syndrome|SARS]]) and the [[Middle East respiratory syndrome coronavirus infection|Middle East respiratory syndrome]] ([[Middle East respiratory syndrome coronavirus infection|MERS]]) epidemic and the ongoing [[COVID-19]] outbreak, multiple mechanisms have been suggested for [[cardiac]] damage.<ref name="ClerkinFried2020">{{cite journal|last1=Clerkin|first1=Kevin J.|last2=Fried|first2=Justin A.|last3=Raikhelkar|first3=Jayant|last4=Sayer|first4=Gabriel|last5=Griffin|first5=Jan M.|last6=Masoumi|first6=Amirali|last7=Jain|first7=Sneha S.|last8=Burkhoff|first8=Daniel|last9=Kumaraiah|first9=Deepa|last10=Rabbani|first10=LeRoy|last11=Schwartz|first11=Allan|last12=Uriel|first12=Nir|title=COVID-19 and Cardiovascular Disease|journal=Circulation|volume=141|issue=20|year=2020|pages=1648–1655|issn=0009-7322|doi=10.1161/CIRCULATIONAHA.120.046941}}</ref> | ||
* Use of [[hydroxychloroquine]] and [[azithromycin]] was associated with [[QT prolongation]] and [[ventricular arrhythmia]] due to [[action potential]] prolongation, inhibition of hERG-K channels, and [[early afterdepolarization]]. | |||
* It is thought that abnormal host immune response is due to over activation of the [[cardiac]] [[sympathetic]] system, [[immune cell-mediated injury]] and inhibition of [[CYP450]] by [[IL6]]. | |||
* Inhibition of [[CYP450]] by [[IL6]] may lead to increased bioavailability of [[QT prolongation]] drugs and [[ventricular arrhythmia]]. | |||
* [[immune cell-mediated injury]] may cause [[inflammatory myocardial scarring]] and [[ventricular arrhythmia]] by the mechanisms of [[electrical imbalance ]] and [[reentry]] | |||
* Overactivity of the [[cardiac]] [[sympathetic system]] is the precursor of [[myocardial ischemia]] and [[cardiac arrhythmia]]. | |||
[[File:COVID-19 arrhythmia1.png|700px|center]] | [[File:COVID-19 arrhythmia1.png|700px|center]] | ||
* [[Acute renal injury]] and [[diarrhea]] may lead to intravascular volume imbalance , [[electrolytes imblance]] resulting [[arrhythmia]]. | |||
* [[Pulmonary hypertension ]] and [[pulmonary embolism]] may cause [[increased]] right sided pressures and [[myocardial injury]] and [[arrhythmia]]. | |||
To browse the pathophysiology of COVID-19, [[COVID-19 pathophysiology|click here]]. | To browse the pathophysiology of COVID-19, [[COVID-19 pathophysiology|click here]]. | ||
==Causes== | ==Causes== | ||
*Potential causes of [[arrhythmia]] in [[covid-19]] include: (doi:10.1016/j.jacep.2020.08.002) | |||
*[[Hypoxia]] | |||
*[[Myocarditis]] | |||
*[[Abnormal host immune response]] | |||
*[[Myocardial ischemia]] | |||
*[[Myocardial strain]] | |||
*[[Electrolytes]] derangement | |||
*[[Intravascular]] volume imbalance | |||
*[[ Drug]] side effects | |||
*Common causes of [[bradyarrhythmia]] in [[covid-19]] [[patients]] include: | |||
*: Use of [[remdesivir]] | |||
*: [[Hypoxia]] | |||
*: [[Viral]] [[myocarditis]] | |||
*: Damage to [[pacemaker cells]] due to [[inflammatory]] [[cytokines]] | |||
==Differentiating COVID-19-associated arrhythmia from other Diseases== | ==Differentiating COVID-19-associated arrhythmia from other Diseases== | ||
[[ | *Differentiation diagnosis of [[arrhythmia]] and conduction disorder related to [[COVID-19]] include the following: | ||
* [[Atrial fibrillation]] | |||
* [[Atrial flutter]] | |||
* [[Supraventricular tachycardia]] | |||
* Nonsustained [[ventricular tachycardia]] | |||
*[[ | * [[Ventricular tachycardia]] | ||
*[[ | * [[Ventricular fibrillation]] | ||
*[[ | * [[Atrioventricular block]] | ||
*[[ | |||
*[[ | |||
*[[ | |||
*[[ | |||
To browse the differential diagnosis of COVID-19, [[COVID-19 differential diagnosis|click here]]. | To browse the differential diagnosis of COVID-19, [[COVID-19 differential diagnosis|click here]]. | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
* | ===Incidence=== | ||
* The [[incidence]] of [[cardiac arrhythmia]] including [[AF]], [[atrial flutter]], [[SVT]], nonsustained [[VT]], [[VT]], [[VF]], marked [[sinus bradycardia]], [[atrioventricular block]], or pauses> 3 seconds was estimated to be 12900 per 100,000 [[covid-19]] [[patients]]. | |||
===Age=== | ===Age=== | ||
The mean age of [[covid-19]] [[patients]] who developed [[arrhythmia]] was 71± 14 years. | |||
===Gender=== | ===Gender=== | ||
[[Arrhythmia]] in [[covid-19]] [[patients]] was more common in [[men]]. | |||
===Race=== | ===Race=== | ||
* | *[[Asian]] individuals with [[COVID-19]] are less likely to develop [[atrial arrhythmia]] compared with other continents (34% versus 81%). However, the [[incidence]] of [[bradyarrhythmia]] and [[atrioventricular block]] were higher in [[asian]] than other continents. | ||
*Distribution of [[ventricular arrhythmia]] was similar to other continents.<ref name="pmid33554620">{{cite journal |vauthors=Coromilas EJ, Kochav S, Goldenthal I, Biviano A, Garan H, Goldbarg S, Kim JH, Yeo I, Tracy C, Ayanian S, Akar J, Singh A, Jain S, Zimerman L, Pimentel M, Osswald S, Twerenbold R, Schaerli N, Crotti L, Fabbri D, Parati G, Li Y, Atienza F, Zatarain E, Tse G, Leung KSK, Guevara-Valdivia ME, Rivera-Santiago CA, Soejima K, De Filippo P, Ferrari P, Malanchini G, Kanagaratnam P, Khawaja S, Mikhail GW, Scanavacca M, Abrahão Hajjar L, Rizerio B, Sacilotto L, Mollazadeh R, Eslami M, Laleh Far V, Mattioli AV, Boriani G, Migliore F, Cipriani A, Donato F, Compagnucci P, Casella M, Dello Russo A, Coromilas J, Aboyme A, O'Brien CG, Rodriguez F, Wang PJ, Naniwadekar A, Moey M, Kow CS, Cheah WK, Auricchio A, Conte G, Hwang J, Han S, Lazzerini PE, Franchi F, Santoro A, Capecchi PL, Joglar JA, Rosenblatt AG, Zardini M, Bricoli S, Bonura R, Echarte-Morales J, Benito-González T, Minguito-Carazo C, Fernández-Vázquez F, Wan EY |title=Worldwide Survey of COVID-19-Associated Arrhythmias |journal=Circ Arrhythm Electrophysiol |volume=14 |issue=3 |pages=e009458 |date=March 2021 |pmid=33554620 |pmc=7982128 |doi=10.1161/CIRCEP.120.009458 |url=}}</ref> | |||
To browse the epidemiology and demographics of COVID-19, [[COVID-19 epidemiology and demographics|click here]]. | To browse the epidemiology and demographics of COVID-19, [[COVID-19 epidemiology and demographics|click here]]. | ||
==Risk Factors== | ==Risk Factors== | ||
* | *Concomitant [[comorbidities]] among [[covid-19]] [[patients]] with [[arrhythmia]] include:<ref name="pmid33554620">{{cite journal |vauthors=Coromilas EJ, Kochav S, Goldenthal I, Biviano A, Garan H, Goldbarg S, Kim JH, Yeo I, Tracy C, Ayanian S, Akar J, Singh A, Jain S, Zimerman L, Pimentel M, Osswald S, Twerenbold R, Schaerli N, Crotti L, Fabbri D, Parati G, Li Y, Atienza F, Zatarain E, Tse G, Leung KSK, Guevara-Valdivia ME, Rivera-Santiago CA, Soejima K, De Filippo P, Ferrari P, Malanchini G, Kanagaratnam P, Khawaja S, Mikhail GW, Scanavacca M, Abrahão Hajjar L, Rizerio B, Sacilotto L, Mollazadeh R, Eslami M, Laleh Far V, Mattioli AV, Boriani G, Migliore F, Cipriani A, Donato F, Compagnucci P, Casella M, Dello Russo A, Coromilas J, Aboyme A, O'Brien CG, Rodriguez F, Wang PJ, Naniwadekar A, Moey M, Kow CS, Cheah WK, Auricchio A, Conte G, Hwang J, Han S, Lazzerini PE, Franchi F, Santoro A, Capecchi PL, Joglar JA, Rosenblatt AG, Zardini M, Bricoli S, Bonura R, Echarte-Morales J, Benito-González T, Minguito-Carazo C, Fernández-Vázquez F, Wan EY |title=Worldwide Survey of COVID-19-Associated Arrhythmias |journal=Circ Arrhythm Electrophysiol |volume=14 |issue=3 |pages=e009458 |date=March 2021 |pmid=33554620 |pmc=7982128 |doi=10.1161/CIRCEP.120.009458 |url=}}</ref> | ||
*:[[Hypertension]] (69%) | |||
*: [[Diabetes mellitus]] (42%) | |||
*: [[Congestive heart failure]] (30%) | |||
*:[[Coronary artery disease]] (24%) | |||
*Independent predictors of [[QTc prolongation]]≥ 500 ms in [[covid-19]] [[patients]] include:<ref name="pmid33478708">{{cite journal |vauthors=O'Connell TF, Bradley CJ, Abbas AE, Williamson BD, Rusia A, Tawney AM, Gaines R, Schott J, Dmitrienko A, Haines DE |title=Hydroxychloroquine/Azithromycin Therapy and QT Prolongation in Hospitalized Patients With COVID-19 |journal=JACC Clin Electrophysiol |volume=7 |issue=1 |pages=16–25 |date=January 2021 |pmid=33478708 |pmc=7406234 |doi=10.1016/j.jacep.2020.07.016 |url=}}</ref> | |||
* [[Older]] age | |||
* Lower [[body mass index]] | |||
* Higher [[creatinine]] level | |||
* Higher peak of [[troponin]] | |||
* [[Congestive heart failure]] | |||
* Use of [[hydroxychloroquine]], [[azithromycin]] | |||
==Screening== | ==Screening== | ||
*There is no established screening method for detecting [[arrhythmia]] related to [[covid-19]]. However, [[QT interval]] measurement is recommended in [[covid-19]] [[patients]] before initiation of treatment with [[hydroxychloroquine]], [[azithromycin]], [[remdesivir]], [[lopinavir]]/[[ritonavir]].<ref name="pmid33478708">{{cite journal |vauthors=O'Connell TF, Bradley CJ, Abbas AE, Williamson BD, Rusia A, Tawney AM, Gaines R, Schott J, Dmitrienko A, Haines DE |title=Hydroxychloroquine/Azithromycin Therapy and QT Prolongation in Hospitalized Patients With COVID-19 |journal=JACC Clin Electrophysiol |volume=7 |issue=1 |pages=16–25 |date=January 2021 |pmid=33478708 |pmc=7406234 |doi=10.1016/j.jacep.2020.07.016 |url=}}</ref> | |||
* | |||
[[ | |||
[[ | |||
== Natural History, Complications and Prognosis== | == Natural History, Complications and Prognosis== | ||
=== | * The majority of [[patients]] with [[covid-19]] who developed [[arrhythmia]]s were intubated.<ref name="WangHu2020">{{cite journal|last1=Wang|first1=Dawei|last2=Hu|first2=Bo|last3=Hu|first3=Chang|last4=Zhu|first4=Fangfang|last5=Liu|first5=Xing|last6=Zhang|first6=Jing|last7=Wang|first7=Binbin|last8=Xiang|first8=Hui|last9=Cheng|first9=Zhenshun|last10=Xiong|first10=Yong|last11=Zhao|first11=Yan|last12=Li|first12=Yirong|last13=Wang|first13=Xinghuan|last14=Peng|first14=Zhiyong|title=Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China|journal=JAMA|volume=323|issue=11|year=2020|pages=1061|issn=0098-7484|doi=10.1001/jama.2020.1585}}</ref> | ||
* [[Atrial fibrillation]] is the most common arrhythmia in [[covid-19]] [[patients]] and is associated with severe [[disease]] and poor [[outcome]]. | |||
* Reported case about new onset [[atrial fibrillation ]] in [[covid-19]] [[patients]] may indicate the [[arrhythmogenicity]] of [[covid-19]] [[infection]]. <ref name="pmid7218462">{{cite journal |vauthors=Kelalis PP, Malek RS |title=Infundibulopelvic stenosis |journal=J Urol |volume=125 |issue=4 |pages=568–71 |date=April 1981 |pmid=7218462 |doi=10.1016/s0022-5347(17)55107-1 |url=}}</ref> | |||
* Early clinical features include deterioration of underlying [[covid-19]] disease, [[ACS]], [[decompensated heart failure]], pre-[[syncope]], [[syncope]]. | |||
* If left untreated, [[patients]] with [[arrhythmia]] may progress to developed decompensated [[heart failure]], [[myocardial ischemia]], [[cardiac arrest]], [[intubation]], [[death]]. | |||
*Common complications of [[arrhythmia]] are [[congestive heart failure]], [[ACS]], [[stroke]], [[sudden cardiac death]]. | |||
* Prognosis is related to the type of [[arrhythmia]] and underlying mechanism of [[arrhythmia]], and survival rate to hospital discharge of [[covid-19]] [[patients]] with [[arrhythmia]] is approximately 51%. | |||
* Among [[covid-19]] [[patients]] with [[ventricular arrhythmia]], [[mortality]] rate (1.4×) and risk of developing to [[ mechanical ventilation]] (1.3×) were higher than other [[arrhythmia]]s, and [[survival rate]] to discharge was approximately 38%.<ref name="pmid33554620">{{cite journal |vauthors=Coromilas EJ, Kochav S, Goldenthal I, Biviano A, Garan H, Goldbarg S, Kim JH, Yeo I, Tracy C, Ayanian S, Akar J, Singh A, Jain S, Zimerman L, Pimentel M, Osswald S, Twerenbold R, Schaerli N, Crotti L, Fabbri D, Parati G, Li Y, Atienza F, Zatarain E, Tse G, Leung KSK, Guevara-Valdivia ME, Rivera-Santiago CA, Soejima K, De Filippo P, Ferrari P, Malanchini G, Kanagaratnam P, Khawaja S, Mikhail GW, Scanavacca M, Abrahão Hajjar L, Rizerio B, Sacilotto L, Mollazadeh R, Eslami M, Laleh Far V, Mattioli AV, Boriani G, Migliore F, Cipriani A, Donato F, Compagnucci P, Casella M, Dello Russo A, Coromilas J, Aboyme A, O'Brien CG, Rodriguez F, Wang PJ, Naniwadekar A, Moey M, Kow CS, Cheah WK, Auricchio A, Conte G, Hwang J, Han S, Lazzerini PE, Franchi F, Santoro A, Capecchi PL, Joglar JA, Rosenblatt AG, Zardini M, Bricoli S, Bonura R, Echarte-Morales J, Benito-González T, Minguito-Carazo C, Fernández-Vázquez F, Wan EY |title=Worldwide Survey of COVID-19-Associated Arrhythmias |journal=Circ Arrhythm Electrophysiol |volume=14 |issue=3 |pages=e009458 |date=March 2021 |pmid=33554620 |pmc=7982128 |doi=10.1161/CIRCEP.120.009458 |url=}}</ref> | |||
* Presence of [[atrial arrhythmia]] in [[covid-19]] [[patients]] was associated with severe [[disease]] and poor [[outcome]].<ref name="pmid33470951">{{cite journal |vauthors=Mulia EPB, Maghfirah I, Rachmi DA, Julario R |title=Atrial arrhythmia and its association with COVID-19 outcome: a pooled analysis |journal=Diagnosis (Berl) |volume= |issue= |pages= |date=January 2021 |pmid=33470951 |doi=10.1515/dx-2020-0155 |url=}}</ref> | |||
* Use of [[remdesivir]] was associated with [[bradycardia]] and [[complete heart block]], especially in [[patients]] with preexisting [[conduction disorder]], older [[patients]] or concomitant use of [[betablocker]].<ref name="pmid34222786">{{cite journal |vauthors=Selvaraj V, Bavishi C, Patel S, Dapaah-Afriyie K |title=Complete heart block associated with Remdesivir in COVID-19: a case report |journal=Eur Heart J Case Rep |volume=5 |issue=7 |pages=ytab200 |date=July 2021 |pmid=34222786 |pmc=8247739 |doi=10.1093/ehjcr/ytab200 |url=}}</ref> | |||
* Use of [[hydroxychloroquine]], [[azithromycin]] were associated with [[QTc prolongation]]. However, the likelihood of [[torsades de pointes]] and [[mortality]] were low.<ref name="pmid33478708">{{cite journal |vauthors=O'Connell TF, Bradley CJ, Abbas AE, Williamson BD, Rusia A, Tawney AM, Gaines R, Schott J, Dmitrienko A, Haines DE |title=Hydroxychloroquine/Azithromycin Therapy and QT Prolongation in Hospitalized Patients With COVID-19 |journal=JACC Clin Electrophysiol |volume=7 |issue=1 |pages=16–25 |date=January 2021 |pmid=33478708 |pmc=7406234 |doi=10.1016/j.jacep.2020.07.016 |url=}}</ref> | |||
* Before prescription of [[hydroxychloroquine]] and [[azithromycin]], potential risk factors of [[QT prolongation]] and [[ECG]] monitoring strategy should be noticed. | |||
* In the presence of [[QTc prolongation]]≥ 500 ms, [[hydroxychloroquine]] and [[azithromycin]] should be withdrawn. | |||
* Reported cases of life-threatening [[arrhythmia]] such as [[high grade atrioventricular block]], [[polymorphic ventricular tachycardia]], [[accelerated ideoventricular rhythm]] and [[atrial fibrillation ]] in [[covid-19]] [[patients]] without severe [[lung]] involvement, showed the need for appropriate [[rhythm]] monitoring, particularly if [[fulminant myocarditis]] is suspected.<ref name="pmid32434385">{{cite journal |vauthors=Kochav SM, Coromilas E, Nalbandian A, Ranard LS, Gupta A, Chung MK, Gopinathannair R, Biviano AB, Garan H, Wan EY |title=Cardiac Arrhythmias in COVID-19 Infection |journal=Circ Arrhythm Electrophysiol |volume=13 |issue=6 |pages=e008719 |date=June 2020 |pmid=32434385 |pmc=7299099 |doi=10.1161/CIRCEP.120.008719 |url=}}</ref> | |||
[[ | *Reported [[ECG]] changes prompting [[arrhythmia]] complication associated medications in [[covid-19]] include: | ||
*[[Remdesivir]]: | |||
: | *:: [[QT prolongation]]<ref name="pmid33240723">{{cite journal |vauthors=Gupta AK, Parker BM, Priyadarshi V, Parker J |title=Cardiac Adverse Events With Remdesivir in COVID-19 Infection |journal=Cureus |volume=12 |issue=10 |pages=e11132 |date=October 2020 |pmid=33240723 |pmc=7682945 |doi=10.7759/cureus.11132 |url=}}</ref> | ||
*:: [[Non specific T waves change]] | |||
: | *:: [[Cardiac arrest]] (1.1%) | ||
: | *:: [[Severe bradycardia]]<ref name="pmid33163977">{{cite journal |vauthors=Gubitosa JC, Kakar P, Gerula C, Nossa H, Finkel D, Wong K, Khatri M, Ali H |title=Marked Sinus Bradycardia Associated With Remdesivir in COVID-19: A Case and Literature Review |journal=JACC Case Rep |volume=2 |issue=14 |pages=2260–2264 |date=November 2020 |pmid=33163977 |pmc=7598346 |doi=10.1016/j.jaccas.2020.08.025 |url=}}</ref><ref name="pmid33903133">{{cite journal |vauthors=Day LB, Abdel-Qadir H, Fralick M |title=Bradycardia associated with remdesivir therapy for COVID-19 in a 59-year-old man |journal=CMAJ |volume=193 |issue=17 |pages=E612–E615 |date=April 2021 |pmid=33903133 |pmc=8101980 |doi=10.1503/cmaj.210300 |url=}}</ref> | ||
*:: Transient [[complete heart block]]<ref name="pmid34222786">{{cite journal |vauthors=Selvaraj V, Bavishi C, Patel S, Dapaah-Afriyie K |title=Complete heart block associated with Remdesivir in COVID-19: a case report |journal=Eur Heart J Case Rep |volume=5 |issue=7 |pages=ytab200 |date=July 2021 |pmid=34222786 |pmc=8247739 |doi=10.1093/ehjcr/ytab200 |url=}}</ref> | |||
*:: [[Atrial fibrillation]] (4%) | |||
* | * [[Azithromycin]] | ||
* | *::[[Bradycardia]], prolonged [[PR interval]], [[QTc prolongation]] with very low risk of [[torsades de pointes]] | ||
*:: Severe interaction with [[amiodarione]], [[disopyramide]], [[dofetilide]], [[flecainide]], [[sotalol]], [[propafenone]] | |||
*:: Moderate interaction with [[betablocker]], [[digoxin]] | |||
*[[Hydroxychloroquine]] | |||
*::[[Bradycardia]], prolonged [[PR interval]], [[QTc prolongation]] with very low risk of [[torsades de pointes]]<ref name="pmid32434385">{{cite journal |vauthors=Kochav SM, Coromilas E, Nalbandian A, Ranard LS, Gupta A, Chung MK, Gopinathannair R, Biviano AB, Garan H, Wan EY |title=Cardiac Arrhythmias in COVID-19 Infection |journal=Circ Arrhythm Electrophysiol |volume=13 |issue=6 |pages=e008719 |date=June 2020 |pmid=32434385 |pmc=7299099 |doi=10.1161/CIRCEP.120.008719 |url=}}</ref> | |||
*:: Severe interaction with [[amiodarone]], [[flecainide]], [[mexiletine]], [[sotalol]], [[dofetilide]] | |||
*::Moderate interaction with [[disopyramide]], [[propafenone]], [[quinidine]], [[digoxin]] | |||
*::Mild interaction with [[metoprolol]], [[nebivolol]], [[propranolol]], [[timolol]], [[verapamil]] | |||
*[[Lopinavir]]/ [[ritonavir]] | |||
*::Prolonged [[PR interval]], [[QTc prolongation]] with very low risk of [[torsades de pointes]] | |||
*:: Severe interaction with [[amiodarone]], [[drondarone]], [[disopyramide]], [[dofetilide]], [[flecainide]], [[sotalol]] | |||
*::Moderate interaction with [[lidocaine]], [[mexiletine]], [[propafenone]], [[quinidine]], [[digoxin]], [[batablocker]], [[calcium channel blocker]]<ref name="pmid32972561">{{cite journal |vauthors=Dherange P, Lang J, Qian P, Oberfeld B, Sauer WH, Koplan B, Tedrow U |title=Arrhythmias and COVID-19: A Review |journal=JACC Clin Electrophysiol |volume=6 |issue=9 |pages=1193–1204 |date=September 2020 |pmid=32972561 |pmc=7417167 |doi=10.1016/j.jacep.2020.08.002 |url=}}</ref> | |||
== Diagnosis == | == Diagnosis == | ||
| Line 187: | Line 173: | ||
=== History and Symptoms === | === History and Symptoms === | ||
[[Cardiac arrhythmia|Arrhythmia]] or [[conduction system disease]] is the nonspecific clinical presentation of [[COVID-19]]. Patients may be [[Tachycardia|tachycardic]] (with or without [[Palpitation|palpitations]]) in the setting of other COVID-19-related symptoms (eg, fever, shortness of breath, pain, etc). | [[Cardiac arrhythmia|Arrhythmia]] or [[conduction system disease]] is the nonspecific clinical presentation of [[COVID-19]]. [[Patients]] may be [[Tachycardia|tachycardic]] (with or without [[Palpitation|palpitations]]) in the setting of other [[COVID-19]]-related symptoms (eg, [[fever]], [[shortness of breath]], [[pain]], etc). | ||
* | *[[Cardiac arrhythmia|Arrhythmia]] presents with the history of: | ||
*[[ | **Slow or irregular [[heartbeat]] or pauses between [[heartbeats]] | ||
*[[ | **Skipping a [[heartbeat]] | ||
*[[ | **[[Heart]] pounding or racing | ||
*[[ | **[[Anxiety]] | ||
**[[Blurred vision]] | |||
**[[Chest pain]] | |||
**[[Dyspnea|Difficulty breathing]] | |||
**[[Syncope|Fainting or nearly fainting]] | |||
**Foggy thinking | |||
**[[Fatigue]] | |||
**[[Perspiration|Sweating]] | |||
**[[Weakness (medical)|Weakness]], [[dizziness]], and [[Lightheadedness and vertigo|light-headedness]]<ref name="urlArrhythmia | NHLBI, NIH">{{cite web |url=https://www.nhlbi.nih.gov/health-topics/arrhythmia |title=Arrhythmia | NHLBI, NIH |format= |work= |accessdate=}}</ref> | |||
=== Physical Examination === | === Physical Examination === | ||
*Patients with COVID-19-associated arrhythmia and [[conduction system disease]] on cardiac auscultation reveal [[tachycardia]] or [[Cardiac arrhythmia|arrhythmias]] (irregular beat). | *[[Patients]] with [[COVID-19]]-associated [[arrhythmia ]] and [[conduction system disease]] on [[cardiac auscultation]] reveal [[tachycardia]] or [[Cardiac arrhythmia|arrhythmias]] (irregular beat). | ||
*[[Sinus tachycardia]], the most common type of [[Cardiac arrhythmia|arrhythmia]] in COVID-19 patients can be due to fever, [[Hypoxemia|hypoxia]], shock due to [[sepsis]], and anxiety. Some pathologic causes of arrhythmias include | *[[Sinus tachycardia]], the most common type of [[Cardiac arrhythmia|arrhythmia]] in [[COVID-19]] [[patients]] can be due to fever, [[Hypoxemia|hypoxia]], [[shock]] due to [[sepsis]], and [[anxiety]]. Some pathologic causes of arrhythmias include [[ventricular arrhythmia]], [[atrial fibrillation]] (pulse rate 100 to 175 bpm) and [[atrial flutter]] (pulse rate 150 bpm).<ref name="GuoFan2020">{{cite journal|last1=Guo|first1=Tao|last2=Fan|first2=Yongzhen|last3=Chen|first3=Ming|last4=Wu|first4=Xiaoyan|last5=Zhang|first5=Lin|last6=He|first6=Tao|last7=Wang|first7=Hairong|last8=Wan|first8=Jing|last9=Wang|first9=Xinghuan|last10=Lu|first10=Zhibing|title=Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19)|journal=JAMA Cardiology|year=2020|issn=2380-6583|doi=10.1001/jamacardio.2020.1017}}</ref> | ||
*To browse the physical examination of COVID-19, [[COVID-19 physical examination|click here]]. | *To browse the physical examination of COVID-19, [[COVID-19 physical examination|click here]]. | ||
| Line 204: | Line 196: | ||
* There are no specific laboratory findings associated with COVID-19-associated arrhythmia. | * There are no specific laboratory findings associated with COVID-19-associated arrhythmia. | ||
* COVID-19 patients with elevated [[troponin T]] experienced higher risk of [[ventricular arrhythmias]] (17.3% in high [[troponin T]] group versus 1.5% in normal [[troponin T]] group, P < 0.001).<ref name="pmid32253318">{{cite journal| author=Duan K, Liu B, Li C, Zhang H, Yu T, Qu J | display-authors=etal| title=Effectiveness of convalescent plasma therapy in severe COVID-19 patients. | journal=Proc Natl Acad Sci U S A | year= 2020 | volume= 117 | issue= 17 | pages= 9490-9496 | pmid=32253318 | doi=10.1073/pnas.2004168117 | pmc=7196837 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32253318 }} </ref> | * COVID-19 patients with elevated [[troponin T]] experienced higher risk of [[ventricular arrhythmias]] (17.3% in high [[troponin T]] group versus 1.5% in normal [[troponin T]] group, P < 0.001).<ref name="pmid32253318">{{cite journal| author=Duan K, Liu B, Li C, Zhang H, Yu T, Qu J | display-authors=etal| title=Effectiveness of convalescent plasma therapy in severe COVID-19 patients. | journal=Proc Natl Acad Sci U S A | year= 2020 | volume= 117 | issue= 17 | pages= 9490-9496 | pmid=32253318 | doi=10.1073/pnas.2004168117 | pmc=7196837 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32253318 }} </ref> | ||
===Electrocardiogram=== | ===Electrocardiogram=== | ||
| Line 262: | Line 252: | ||
*We ought to consider that myocardial injury may bring about atrial or [[Cardiac fibrosis|ventricular fibrosis]], the substrate for resulting [[Cardiac arrhythmia|cardiovascular arrhythmias]]. | *We ought to consider that myocardial injury may bring about atrial or [[Cardiac fibrosis|ventricular fibrosis]], the substrate for resulting [[Cardiac arrhythmia|cardiovascular arrhythmias]]. | ||
*[[COVID-19]] patients with evidence of myocardial injury should undergo cardiac [[Magnetic resonance imaging|magnetic resonance]] to assess the extent of [[Scar tissue|myocardial scar]].<ref name="KochiTagliari2020">{{cite journal|last1=Kochi|first1=Adriano Nunes|last2=Tagliari|first2=Ana Paula|last3=Forleo|first3=Giovanni Battista|last4=Fassini|first4=Gaetano Michele|last5=Tondo|first5=Claudio|title=Cardiac and arrhythmic complications in patients with COVID‐19|journal=Journal of Cardiovascular Electrophysiology|volume=31|issue=5|year=2020|pages=1003–1008|issn=1045-3873|doi=10.1111/jce.14479}}</ref> | *[[COVID-19]] patients with evidence of myocardial injury should undergo cardiac [[Magnetic resonance imaging|magnetic resonance]] to assess the extent of [[Scar tissue|myocardial scar]].<ref name="KochiTagliari2020">{{cite journal|last1=Kochi|first1=Adriano Nunes|last2=Tagliari|first2=Ana Paula|last3=Forleo|first3=Giovanni Battista|last4=Fassini|first4=Gaetano Michele|last5=Tondo|first5=Claudio|title=Cardiac and arrhythmic complications in patients with COVID‐19|journal=Journal of Cardiovascular Electrophysiology|volume=31|issue=5|year=2020|pages=1003–1008|issn=1045-3873|doi=10.1111/jce.14479}}</ref> | ||
===Other Imaging Findings=== | ===Other Imaging Findings=== | ||
*There are no other imaging findings associated with COVID-19-associated arrhythmia. | *There are no other imaging findings associated with [[COVID-19]]-associated [[arrhythmia]]. | ||
=== Other Diagnostic Studies === | === Other Diagnostic Studies === | ||
*[[Cardiac biomarkers|Myocardial biomarkers]] should be assessed in all patients with [[COVID-19|COVID‐19]].<ref name="KochiTagliari2020">{{cite journal|last1=Kochi|first1=Adriano Nunes|last2=Tagliari|first2=Ana Paula|last3=Forleo|first3=Giovanni Battista|last4=Fassini|first4=Gaetano Michele|last5=Tondo|first5=Claudio|title=Cardiac and arrhythmic complications in patients with COVID‐19|journal=Journal of Cardiovascular Electrophysiology|volume=31|issue=5|year=2020|pages=1003–1008|issn=1045-3873|doi=10.1111/jce.14479}}</ref> | *[[Cardiac biomarkers|Myocardial biomarkers]] should be assessed in all patients with [[COVID-19|COVID‐19]].<ref name="KochiTagliari2020">{{cite journal|last1=Kochi|first1=Adriano Nunes|last2=Tagliari|first2=Ana Paula|last3=Forleo|first3=Giovanni Battista|last4=Fassini|first4=Gaetano Michele|last5=Tondo|first5=Claudio|title=Cardiac and arrhythmic complications in patients with COVID‐19|journal=Journal of Cardiovascular Electrophysiology|volume=31|issue=5|year=2020|pages=1003–1008|issn=1045-3873|doi=10.1111/jce.14479}}</ref> | ||
| Line 278: | Line 268: | ||
== Treatment == | == Treatment == | ||
=== Medical Therapy | === Medical Therapy based on 2020 ESC Guidline for management of arrhythmia in [[covid-19]] [[patients]] === | ||
*The mainstay of therapy of [[arrhythmia]] in [[patients]] with [[covid-19]] is limiting exposure and minimizing drug-drug interactions.<ref name="pmid32972561">{{cite journal |vauthors=Dherange P, Lang J, Qian P, Oberfeld B, Sauer WH, Koplan B, Tedrow U |title=Arrhythmias and COVID-19: A Review |journal=JACC Clin Electrophysiol |volume=6 |issue=9 |pages=1193–1204 |date=September 2020 |pmid=32972561 |pmc=7417167 |doi=10.1016/j.jacep.2020.08.002 |url=}}</ref> | |||
*Treatment of [[tachyarrhythmia]] and [[bradyarrhythmia]] in [[patients]] with [[covid-19]] is similar to any patients with [[arrhythmia]] due to [[infection]] and transient [[metabolic disturbance]]. | |||
* In [[patients]] who use [[QTc prolongation]] drugs, or have a history of inherited [[arrhythmia]], specific consideration should be given. | |||
* | |||
* | |||
* | ===[[Bradyarrhythmia]]=== | ||
*Causes of [[bradycardia]] ([[sinus node block]] or [[AV block]]) in [[covid-19]] [[patients]]:<ref name="pmid32972561">{{cite journal |vauthors=Dherange P, Lang J, Qian P, Oberfeld B, Sauer WH, Koplan B, Tedrow U |title=Arrhythmias and COVID-19: A Review |journal=JACC Clin Electrophysiol |volume=6 |issue=9 |pages=1193–1204 |date=September 2020 |pmid=32972561 |pmc=7417167 |doi=10.1016/j.jacep.2020.08.002 |url=}}</ref> | |||
*:Side effects of drugs such as [[hydroxychloroquine]], [[lopinavir]]/[[ritonavir]], [[azithromycin]] | |||
*: [[Myocarditis]]: if conduction system involved | |||
*: Transient [[bradycardia]] during suction of [[secretion]] in [[intubated]] [[patients]] or [[proning position]] leading to increased [[vagal tone]] | |||
# In [[patients]] with persistent [[bradycardia]], before insertion of [[ temporary pacemaker]], [[atropine]] or [[isoprenaline]] are considered. | |||
# [[Temporary pacemaker]] is the first option before making decision for [[permanent pacemaker]] because of the transient nature of [[bradyarrhythmia]], [[critical illness]], risk of [[bacterial superinfection]], risk of device [[infection]]. | |||
# After recovery of [[covid-19]] , reevaluation about [[permanent pacemaker implantation ]] should be considered.<ref name="pmid32350745">{{cite journal |vauthors=Saenz LC, Miranda A, Speranza R, Texeira RA, Rojel U, Enriquez A, Figuereido M |title=Recommendations for the organization of electrophysiology and cardiac pacing services during the COVID-19 pandemic : Latin American Heart Rhythm Society (LAHRS) in collaboration with: Colombian College Of Electrophysiology, Argentinian Society of Cardiac Electrophysiology (SADEC), Brazilian Society Of Cardiac Arrhythmias (SOBRAC), Mexican Society Of Cardiac Electrophysiology (SOMEEC) |journal=J Interv Card Electrophysiol |volume=59 |issue=2 |pages=307–313 |date=November 2020 |pmid=32350745 |pmc=7189002 |doi=10.1007/s10840-020-00747-5 |url=}}</ref> | |||
* If the use of [[remdesivir]] is associated with [[severe bradycardia]], [[remdesivir]] should be discontinued, and [[ECG]] monitoring is recommended.<ref name="pmid33903133">{{cite journal |vauthors=Day LB, Abdel-Qadir H, Fralick M |title=Bradycardia associated with remdesivir therapy for COVID-19 in a 59-year-old man |journal=CMAJ |volume=193 |issue=17 |pages=E612–E615 |date=April 2021 |pmid=33903133 |pmc=8101980 |doi=10.1503/cmaj.210300 |url=}}</ref> | |||
=== | ===[[Atrial tachyarrhythmia]] ([[supraventricular tachycardia]], [[atrial fibrillation]], [[atrial flutter]])=== | ||
*Treatment of underlying causes including [[hypoxia]], [[metabolic imbalance]], [[electrolytes imbalance]], [[proarrhythmic effect of drugs]], [[myocardial ischemia]] | |||
*In the presence of [[supraventricular tachycardia]]: administration of [[adenosine]], [[low threshold shock]] in refractory cases with [[hemodynamic instability]], administration of [[betablocker]] or [[calcium channel blocker]] with concerns about interaction with [[antiviral]] drug or the risk of [[bradycardia]] and [[QTc prolongation]] should be noticed. | |||
*In [[patients]] with [[atrial fibrillation]] or [[atrial flutter]], [[betablockers]] and [[calcium channel blockers]] are preferred to rating control and discontinuation of [[antiarrhythmic]] drug such as [[sotalol]], [[flecainide]], [[amiodarone]] and [[propafenone]] is recommended because of serious drug-drug interaction with [[antiviral]] [[drugs]]. | |||
*[[Rhythm]] control strategy should be reserved only for [[patients]] with [[ unstable hemodynamic]] and [[congestive heart failure]]. | |||
* [[Anticoagulant]] therapy should be considered in [[covid-19]] [[patients]] with [[atrial fibrillation]] due to [[hypercoagulability]] state in such [[condition]]. | |||
*[[Immunosupressant]] therapy is considered for [[patients]] with [[myocarditis]]. | |||
* | ===[[Ventricular arrhythmia]]=== | ||
*Treatment of underlying causes of [[ventricular arrhythmia]] such as [[hypoxia]], [[electrolytes imbalance]], [[proarrhythmic]] effect of [[drug]]s are recommended. | |||
* [[Amiodarone]] , [[lidocaine]] are first choice of [[VT]] storm therapy, especially in the setting of [[myocardial ischemia]]. | |||
* [[Esmolol]], [[sedation]], [[intubation]] are further choices for treatnig [[ventricular arrhythmia]] storm. | |||
*[[Lidocaine]] and [[mexiletine]] are useful in the context of [[prolonged QT]] interval and [[torsades de pointes]] due to slightly shortening of [[QT interval]]. | |||
* In the presence of [[polymorphic ventricular tachycardia]] due to [[QT prolongation]] by [[antiviral therapy]], discontinuation the [[antiviral therapy]] and [[infusion]] of [[magnesium]] and correction of [[hypokalemia]] and infusion of [[isoprenaline]] are recommended. | |||
*In case of recurrent [[torsades de pointes]] and [[bradycardia]], [[arrhythmia]] can be suppressed by overdrive pacing of [[temporary pacemaker]] [[implantation]]. | |||
* [[Echocardiogtaphy]] is needed if there is new onset of malignant [[ventricular arrhythmia]] unrelated to [[prolonged QTc]]. | |||
* | ===[[QT prolongation]] in [[covid-19]] therapy=== | ||
* [[QT prolongation ]] has been found in 12% of [[patients]] recieving [[hydroxychloroquine]], [[azithromycin]], or both. However, there was no [[torsades de pointes]].<ref name="pmid32463348">{{cite journal |vauthors=Ramireddy A, Chugh H, Reinier K, Ebinger J, Park E, Thompson M, Cingolani E, Cheng S, Marban E, Albert CM, Chugh SS |title=Experience With Hydroxychloroquine and Azithromycin in the Coronavirus Disease 2019 Pandemic: Implications for QT Interval Monitoring |journal=J Am Heart Assoc |volume=9 |issue=12 |pages=e017144 |date=June 2020 |pmid=32463348 |pmc=7429030 |doi=10.1161/JAHA.120.017144 |url=}}</ref> | |||
* High dose of [[chloroquine]] (600 mg BD for 10 days compared with 450 mg BD for one day then 450mg daily for 4 days) was associated with increased adverse effects.<ref name="pmid32330277">{{cite journal |vauthors=Borba MGS, Val FFA, Sampaio VS, Alexandre MAA, Melo GC, Brito M, Mourão MPG, Brito-Sousa JD, Baía-da-Silva D, Guerra MVF, Hajjar LA, Pinto RC, Balieiro AAS, Pacheco AGF, Santos JDO, Naveca FG, Xavier MS, Siqueira AM, Schwarzbold A, Croda J, Nogueira ML, Romero GAS, Bassat Q, Fontes CJ, Albuquerque BC, Daniel-Ribeiro CT, Monteiro WM, Lacerda MVG |title=Effect of High vs Low Doses of Chloroquine Diphosphate as Adjunctive Therapy for Patients Hospitalized With Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection: A Randomized Clinical Trial |journal=JAMA Netw Open |volume=3 |issue=4 |pages=e208857 |date=April 2020 |pmid=32330277 |doi=10.1001/jamanetworkopen.2020.8857 |url=}}</ref> | |||
*High risk [[patients]] for [[QT prolongation]] include:<ref name="pmid33521580">{{cite journal |vauthors=Castagna A, Ruotolo G, Manzo C |title=Hydroxychloroquine and QT Prolongation in Older Patients with Rheumatic Diseases: Who is afraid of the Boogeyman? We are not! |journal=Mediterr J Rheumatol |volume=31 |issue=4 |pages=433–435 |date=December 2020 |pmid=33521580 |pmc=7841093 |doi=10.31138/mjr.31.4.433 |url=}}</ref> | |||
*:Age> 68 years | |||
*:[[Female]] sex | |||
*:Use of [[loop diuretic]] | |||
*:Serum [[potassium]] level ≤3.5 mEq/l | |||
*: Baseline QTc≥ 450 ms | |||
*:Acute [[myocardial infarction]] | |||
*:Use of numbers [[QT prolongation]] [[medications]] | |||
*:[[Sepsis]] | |||
*: [[Heart failure]] | |||
* In the presence of baseline QTc≥ 500 ms, or increased greater than 60 ms after 2-3 hours of administration of [[hydroxychloroquine]] or other [[QT prolongation]] [[drugs]], risk of [[torsades de pointes]] should be considered.<ref name="pmid32703574">{{cite journal |vauthors=Cheung CC, Davies B, Gibbs K, Laksman ZW, Krahn AD |title=Multilead QT Screening Is Necessary for QT Measurement: Implications for Management of Patients in the COVID-19 Era |journal=JACC Clin Electrophysiol |volume=6 |issue=7 |pages=878–880 |date=July 2020 |pmid=32703574 |pmc=7141442 |doi=10.1016/j.jacep.2020.04.001 |url=}}</ref> | |||
=== | ===[[Cardiac ]] medications interaction with [[covid-19]] therapy=== | ||
*The level of drug that are metabolized by CP450 isoenzyme such as [[amiodarone]], [[propafenon]], [[flecainide]], [[quinidine]], [[apixaban]], [[rivaroxaban]] can be increased by administration of [[lopinavir]]/[[ritonavir]]. | |||
== Surgery == | |||
[[Electrophysiology]] study in an [[elective procedure]] and should be planned for management of specific [[arrhythmia]]s after recovery of [[covid-19]] [[infection]]. | |||
== | ==Primary Prevention== | ||
* | * Effective measurement for [[primary prevention]] of [[ventricular arrhythmia]] in [[covid-19]] [[patients]] who recieve [[hydroxychloroquine]] and [[azithromycin]] or other [[QTc prolongation]] [[drugs]] is determination baseline [[QTc]] on [[ECG]]. | ||
* If baseline QTc is > 500ms for [[QRS]]< 120 ms, or if QTc is >550 ms for [[QRS]]> 120ms, or QTc prolonged by 60 ms, these medications should be withheld.<ref name="pmid32434385">{{cite journal |vauthors=Kochav SM, Coromilas E, Nalbandian A, Ranard LS, Gupta A, Chung MK, Gopinathannair R, Biviano AB, Garan H, Wan EY |title=Cardiac Arrhythmias in COVID-19 Infection |journal=Circ Arrhythm Electrophysiol |volume=13 |issue=6 |pages=e008719 |date=June 2020 |pmid=32434385 |pmc=7299099 |doi=10.1161/CIRCEP.120.008719 |url=}}</ref> | |||
* [[Primary prevention]] strategy in [[covid-19]] [[patients]] with [[brugada]] pattern type 1 is controlling [[fever]] by [[acetaminophen]] for reducing the risk of [[ventricular arrhythmia]] and [[self isolation]].<ref name="pmid32244059">{{cite journal| author=Wu CI, Postema PG, Arbelo E, Behr ER, Bezzina CR, Napolitano C | display-authors=etal| title=SARS-CoV-2, COVID-19, and inherited arrhythmia syndromes. | journal=Heart Rhythm | year= 2020 | volume= | issue= | pages= | pmid=32244059 | doi=10.1016/j.hrthm.2020.03.024 | pmc=7156157 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32244059 }} </ref> | |||
==Secondary Prevention== | |||
[[Secondary prevention ]] for [[covid-19]] associated with [[arrhythmia]] is implantation of [[ICD]] after recovery of [[covid-19]] in case of [[ventricular arrhythmia]] and low [[LVEF]] based on the guideline. | |||
==References== | ==References== | ||
Latest revision as of 05:51, 21 October 2021
For COVID-19 frequently asked inpatient questions, click here
For COVID-19 frequently asked outpatient questions, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Sara Zand, M.D.[2] Tayyaba Ali, M.D.[3]
Synonyms and keywords:COVID-19-associated dysrhythmia
Overview
Sever acute respiratory syndrome coronavirus-2 (SARS-COV-2) is the virus that causes coronavirus disease 2019 may affect every organ system including the heart. Arrhythmia is a disorder of conduction system including atrial arrhythmia, ventricular arrhythmia, bradyarrhythmia , resulting from direct effect of virus by attaching viral spike protein to ACE2 receptors on myocardium and inducing myocardial injury and conduction damage system or indirect effect of covid-19 such as coexisting hypoxia, electrolytes disarray, and the administration of arrhythmogenic medications (hydroxychloroquine, azithromycin). Reported case about new onset atrial fibrillation in covid-19 infection may indicate the atrial arrhythmogenicity of covid-19 infection. In the presence of covid-19, approperiate approach to life threatening arrhythmia and considering fulminant myocarditis are warranted. High number of out-of hospital cardiac arrest in Italy during the 40 first days of initiation of pandemic, raised the concerns about the risk of arrhythmia in covid-19. Incidence of arrhythmia in ICU admitted covid-19 patients increased to 10 folds. Cardiac arrhythmia was associated with increased mortality and morbidity in hospitalized covid-19 patients.
Historical Perspective
- Diseases of heart and lung are the most common causes of COVID-19-related death.[1]
- Cardiac rhythm problems are increasingly recognized as a clinical manifestation of COVID-19.[2]
- There is anecdotal evidence of sudden cardiac death among COVID-19 patients.[3] According to a study, 51 of 85 fatal cases of COVID-19 from Wuhan developed an arrhythmia, and 2 patients died of malignant arrhythmia.[4]
- In 137 subjects from Hubei province, 10 patients (7.3%) noted palpitations as one of the initial symptoms.[5]
To browse the historical perspective of COVID-19, click here.
Classification
- Arrhythmia related to COVID-19 may be classified into atrial arrhythmia (81.8%), ventricular arrhythmia (21%), bradyarrhythmia (22.6%) as follows:
- Atrial fibrillation
- Atrial flutter
- Supraventricular tachycardia
- Nonsustained ventricular tachycardia
- Ventricular tachycardia
- Ventricular fibrillation
- Atrioventricular block
- Marked sinus bradycardia (heart rate<40 bpm)
Pathophysiology
- Respiratory disease is the chief target of COVID-19.
- Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) utilizes S-spike to bind to angiotensin-converting enzyme 2 (ACE2) receptors to enter the cells.
- Type 1 and type 2 pneumocytes exhibit ACE 2 receptors in the lung.
- Studies report that coronary endothelial cells in the heart and intrarenal endothelial cells and renal tubular epithelial cells in the kidney exhibit ACE2. ACE2 is an inverse regulator of the renin-angiotensin system.[6]
- The interaction between SARS-CoV-2 and ACE2 can bring about changes in ACE2 pathways prompting intense injury to the lung, heart, and endothelial cells.
- Hypoxia and electrolyte abnormalities that are common in the acute phase of severe COVID-19 can potentiate cardiac arrhythmias.
- Binding of SARS-CoV-2 to ACE2 receptors can result in hypokalemia which causes various types of arrhythmia.
- Elevated levels of cytokines as a result of the systemic inflammatory response of the severe Coronavirus disease 2019 (COVID-19) can cause injury to multiple organs, including cardiac myocytes.[7]
- In COVID-19 patients, excessive ranges of circulating cytokines, especially interleukin (IL)-6 is related to in-hospital death.[8]
- As a result of cytokine storm triggered by SARS-CoV-2 that includes IL-6, tumor necrosis factor (TNF) α, and IL-1, duration of ventricular action potential can be prolonged.
- Studies suggest that cytokine storm can modulate the function of cardiomyocyte ion channels such as Na+, K+ and Ca+ channels (inflammatory cardiac channelopathies).[9]
- According to the data based on studies on previous Severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS) epidemic and the ongoing COVID-19 outbreak, multiple mechanisms have been suggested for cardiac damage.[10]
- Use of hydroxychloroquine and azithromycin was associated with QT prolongation and ventricular arrhythmia due to action potential prolongation, inhibition of hERG-K channels, and early afterdepolarization.
- It is thought that abnormal host immune response is due to over activation of the cardiac sympathetic system, immune cell-mediated injury and inhibition of CYP450 by IL6.
- Inhibition of CYP450 by IL6 may lead to increased bioavailability of QT prolongation drugs and ventricular arrhythmia.
- immune cell-mediated injury may cause inflammatory myocardial scarring and ventricular arrhythmia by the mechanisms of electrical imbalance and reentry
- Overactivity of the cardiac sympathetic system is the precursor of myocardial ischemia and cardiac arrhythmia.
- Acute renal injury and diarrhea may lead to intravascular volume imbalance , electrolytes imblance resulting arrhythmia.
- Pulmonary hypertension and pulmonary embolism may cause increased right sided pressures and myocardial injury and arrhythmia.
To browse the pathophysiology of COVID-19, click here.
Causes
- Potential causes of arrhythmia in covid-19 include: (doi:10.1016/j.jacep.2020.08.002)
- Hypoxia
- Myocarditis
- Abnormal host immune response
- Myocardial ischemia
- Myocardial strain
- Electrolytes derangement
- Intravascular volume imbalance
- Drug side effects
- Common causes of bradyarrhythmia in covid-19 patients include:
- Use of remdesivir
- Hypoxia
- Viral myocarditis
- Damage to pacemaker cells due to inflammatory cytokines
Differentiating COVID-19-associated arrhythmia from other Diseases
- Differentiation diagnosis of arrhythmia and conduction disorder related to COVID-19 include the following:
- Atrial fibrillation
- Atrial flutter
- Supraventricular tachycardia
- Nonsustained ventricular tachycardia
- Ventricular tachycardia
- Ventricular fibrillation
- Atrioventricular block
To browse the differential diagnosis of COVID-19, click here.
Epidemiology and Demographics
Incidence
- The incidence of cardiac arrhythmia including AF, atrial flutter, SVT, nonsustained VT, VT, VF, marked sinus bradycardia, atrioventricular block, or pauses> 3 seconds was estimated to be 12900 per 100,000 covid-19 patients.
Age
The mean age of covid-19 patients who developed arrhythmia was 71± 14 years.
Gender
Arrhythmia in covid-19 patients was more common in men.
Race
- Asian individuals with COVID-19 are less likely to develop atrial arrhythmia compared with other continents (34% versus 81%). However, the incidence of bradyarrhythmia and atrioventricular block were higher in asian than other continents.
- Distribution of ventricular arrhythmia was similar to other continents.[11]
To browse the epidemiology and demographics of COVID-19, click here.
Risk Factors
- Concomitant comorbidities among covid-19 patients with arrhythmia include:[11]
- Hypertension (69%)
- Diabetes mellitus (42%)
- Congestive heart failure (30%)
- Coronary artery disease (24%)
- Independent predictors of QTc prolongation≥ 500 ms in covid-19 patients include:[12]
- Older age
- Lower body mass index
- Higher creatinine level
- Higher peak of troponin
- Congestive heart failure
- Use of hydroxychloroquine, azithromycin
Screening
- There is no established screening method for detecting arrhythmia related to covid-19. However, QT interval measurement is recommended in covid-19 patients before initiation of treatment with hydroxychloroquine, azithromycin, remdesivir, lopinavir/ritonavir.[12]
Natural History, Complications and Prognosis
- The majority of patients with covid-19 who developed arrhythmias were intubated.[13]
- Atrial fibrillation is the most common arrhythmia in covid-19 patients and is associated with severe disease and poor outcome.
- Reported case about new onset atrial fibrillation in covid-19 patients may indicate the arrhythmogenicity of covid-19 infection. [14]
- Early clinical features include deterioration of underlying covid-19 disease, ACS, decompensated heart failure, pre-syncope, syncope.
- If left untreated, patients with arrhythmia may progress to developed decompensated heart failure, myocardial ischemia, cardiac arrest, intubation, death.
- Common complications of arrhythmia are congestive heart failure, ACS, stroke, sudden cardiac death.
- Prognosis is related to the type of arrhythmia and underlying mechanism of arrhythmia, and survival rate to hospital discharge of covid-19 patients with arrhythmia is approximately 51%.
- Among covid-19 patients with ventricular arrhythmia, mortality rate (1.4×) and risk of developing to mechanical ventilation (1.3×) were higher than other arrhythmias, and survival rate to discharge was approximately 38%.[11]
- Presence of atrial arrhythmia in covid-19 patients was associated with severe disease and poor outcome.[15]
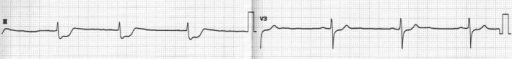
- Use of remdesivir was associated with bradycardia and complete heart block, especially in patients with preexisting conduction disorder, older patients or concomitant use of betablocker.[16]
- Use of hydroxychloroquine, azithromycin were associated with QTc prolongation. However, the likelihood of torsades de pointes and mortality were low.[12]
- Before prescription of hydroxychloroquine and azithromycin, potential risk factors of QT prolongation and ECG monitoring strategy should be noticed.
- In the presence of QTc prolongation≥ 500 ms, hydroxychloroquine and azithromycin should be withdrawn.
- Reported cases of life-threatening arrhythmia such as high grade atrioventricular block, polymorphic ventricular tachycardia, accelerated ideoventricular rhythm and atrial fibrillation in covid-19 patients without severe lung involvement, showed the need for appropriate rhythm monitoring, particularly if fulminant myocarditis is suspected.[17]
- Reported ECG changes prompting arrhythmia complication associated medications in covid-19 include:
- Remdesivir:
- Azithromycin
- Bradycardia, prolonged PR interval, QTc prolongation with very low risk of torsades de pointes
- Severe interaction with amiodarione, disopyramide, dofetilide, flecainide, sotalol, propafenone
- Moderate interaction with betablocker, digoxin
- Hydroxychloroquine
- Bradycardia, prolonged PR interval, QTc prolongation with very low risk of torsades de pointes[17]
- Severe interaction with amiodarone, flecainide, mexiletine, sotalol, dofetilide
- Moderate interaction with disopyramide, propafenone, quinidine, digoxin
- Mild interaction with metoprolol, nebivolol, propranolol, timolol, verapamil
- Lopinavir/ ritonavir
- Prolonged PR interval, QTc prolongation with very low risk of torsades de pointes
- Severe interaction with amiodarone, drondarone, disopyramide, dofetilide, flecainide, sotalol
- Moderate interaction with lidocaine, mexiletine, propafenone, quinidine, digoxin, batablocker, calcium channel blocker[21]
Diagnosis
Diagnostic Study of Choice
- ECG:
- Most patients with the severe COVID-19, and especially patients who receive QT-prolonging medications, should have a baseline electrocardiogram (ECG) performed at the time of admission to the hospital.
- The best technique to get the QT interval is with a 12-lead electrocardiogram (ECG). However, to scale back exposure to hospital workers, this could not perpetually be possible.
- A single-lead ECG might underestimate the QT interval, and there ought to be an effort to use a multiple-lead telemetry system to observe the QT interval.[22][23]
- Transthoracic echocardiography:
- Transthoracic echocardiography is recommended for an inpatient with heart failure, arrhythmia, ECG changes, or newly diagnosed cardiomegaly on chest x-ray or CT-chest.[24]
To browse the diagnostic study of choice of COVID-19, click here.
History and Symptoms
Arrhythmia or conduction system disease is the nonspecific clinical presentation of COVID-19. Patients may be tachycardic (with or without palpitations) in the setting of other COVID-19-related symptoms (eg, fever, shortness of breath, pain, etc).
- Arrhythmia presents with the history of:
- Slow or irregular heartbeat or pauses between heartbeats
- Skipping a heartbeat
- Heart pounding or racing
- Anxiety
- Blurred vision
- Chest pain
- Difficulty breathing
- Fainting or nearly fainting
- Foggy thinking
- Fatigue
- Sweating
- Weakness, dizziness, and light-headedness[25]
Physical Examination
- Patients with COVID-19-associated arrhythmia and conduction system disease on cardiac auscultation reveal tachycardia or arrhythmias (irregular beat).
- Sinus tachycardia, the most common type of arrhythmia in COVID-19 patients can be due to fever, hypoxia, shock due to sepsis, and anxiety. Some pathologic causes of arrhythmias include ventricular arrhythmia, atrial fibrillation (pulse rate 100 to 175 bpm) and atrial flutter (pulse rate 150 bpm).[26]
- To browse the physical examination of COVID-19, click here.
Laboratory Findings
- There are no specific laboratory findings associated with COVID-19-associated arrhythmia.
- COVID-19 patients with elevated troponin T experienced higher risk of ventricular arrhythmias (17.3% in high troponin T group versus 1.5% in normal troponin T group, P < 0.001).[27]
Electrocardiogram
COVID-19-associated arrhythmia findings include:
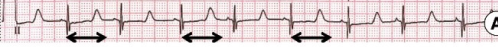
- Prolong QT Interval:
- According to a multicenter study done in New York that involved 4250 COVID-19 patients, 260 patients (6.1%) had corrected QT interval (QTc) >500 milliseconds at the time of admittance.
- However, in another study that involved 84 patients who got hydroxychloroquine and azithromycin, the baseline QTc interval was 435 milliseconds before receiving these medications.[28][29]
- Atrial Arrhythmia:
- According to a study, among 393 patients with COVID-19, atrial arrhythmias were more common among patients requiring invasive mechanical ventilation than noninvasive mechanical ventilation (17.7% versus 1.9%).[30]

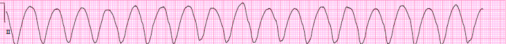
- Ventricular Arrhythmia:
- According to a study done in Wuhan, China. among 187 hospitalized patients with COVID-19, 11 patients (5.9%) developed ventricular tachyarrhythmias.[31]
- Cardiac Arrest:
- According to a Lombardia Cardiac Arrest Registry (Lombardia CARe) in the region of Lombardy, Italy.
- Out of 9806 cases of COVID-19, 362 cases of out-of-hospital cardiac arrest were reported during the study time frame in 2020.
- During a similar period in 2019, 229 cases of out-of-hospital cardiac arrest were reported, which means an increment of 58% was observed in 2020 among COVID-19 patients.
- According to the records from a tertiary care hospital in Wuhan. Out of 761 patients with severe COVID-19, 151 patients developed in-hospital cardiac arrest.
- 136 patients received resuscitation. Out of 136 patients, 119 patients had a respiratory cause.
- 10 patients had a cardiac cause. 7 patients had other causes.
- Ventricular fibrillation or pulseless ventricular tachycardia was observed in 8 patients (5.9%), Pulseless electrical activity in 6 patients (4.4%), and asystole in 122 COVID-19 patients (89.7%).[32][33]
- According to a Lombardia Cardiac Arrest Registry (Lombardia CARe) in the region of Lombardy, Italy.
- To browse the electrocardiogram findings of COVID-19, click here.
X-Ray
- To browse the X-ray finding of COVID-19, click here.
Echocardiography/Ultrasound
- There are no specific echocardiography/ultrasound findings associated with coronavirus infection.
- Non specific echocardiographic findings can include:[34][35]
- Left ventricular systolic dysfunction
- Pericardial effusion
- Myocardial edema
- Increased wall thickness with diffuse biventricular hypokinesis
CT Scan
- To browse the CT-Scan findings of COVID-19, click here.
MRI
- We ought to consider that myocardial injury may bring about atrial or ventricular fibrosis, the substrate for resulting cardiovascular arrhythmias.
- COVID-19 patients with evidence of myocardial injury should undergo cardiac magnetic resonance to assess the extent of myocardial scar.[36]
Other Imaging Findings
- There are no other imaging findings associated with COVID-19-associated arrhythmia.
Other Diagnostic Studies
- Myocardial biomarkers should be assessed in all patients with COVID‐19.[36]
- American Heart Association (AHA) recommends the following tests to diagnose arrhythmia:
Treatment
Medical Therapy based on 2020 ESC Guidline for management of arrhythmia in covid-19 patients
- The mainstay of therapy of arrhythmia in patients with covid-19 is limiting exposure and minimizing drug-drug interactions.[21]
- Treatment of tachyarrhythmia and bradyarrhythmia in patients with covid-19 is similar to any patients with arrhythmia due to infection and transient metabolic disturbance.
- In patients who use QTc prolongation drugs, or have a history of inherited arrhythmia, specific consideration should be given.
Bradyarrhythmia
- Causes of bradycardia (sinus node block or AV block) in covid-19 patients:[21]
- Side effects of drugs such as hydroxychloroquine, lopinavir/ritonavir, azithromycin
- Myocarditis: if conduction system involved
- Transient bradycardia during suction of secretion in intubated patients or proning position leading to increased vagal tone
- In patients with persistent bradycardia, before insertion of temporary pacemaker, atropine or isoprenaline are considered.
- Temporary pacemaker is the first option before making decision for permanent pacemaker because of the transient nature of bradyarrhythmia, critical illness, risk of bacterial superinfection, risk of device infection.
- After recovery of covid-19 , reevaluation about permanent pacemaker implantation should be considered.[37]
- If the use of remdesivir is associated with severe bradycardia, remdesivir should be discontinued, and ECG monitoring is recommended.[20]
Atrial tachyarrhythmia (supraventricular tachycardia, atrial fibrillation, atrial flutter)
- Treatment of underlying causes including hypoxia, metabolic imbalance, electrolytes imbalance, proarrhythmic effect of drugs, myocardial ischemia
- In the presence of supraventricular tachycardia: administration of adenosine, low threshold shock in refractory cases with hemodynamic instability, administration of betablocker or calcium channel blocker with concerns about interaction with antiviral drug or the risk of bradycardia and QTc prolongation should be noticed.
- In patients with atrial fibrillation or atrial flutter, betablockers and calcium channel blockers are preferred to rating control and discontinuation of antiarrhythmic drug such as sotalol, flecainide, amiodarone and propafenone is recommended because of serious drug-drug interaction with antiviral drugs.
- Rhythm control strategy should be reserved only for patients with unstable hemodynamic and congestive heart failure.
- Anticoagulant therapy should be considered in covid-19 patients with atrial fibrillation due to hypercoagulability state in such condition.
- Immunosupressant therapy is considered for patients with myocarditis.
Ventricular arrhythmia
- Treatment of underlying causes of ventricular arrhythmia such as hypoxia, electrolytes imbalance, proarrhythmic effect of drugs are recommended.
- Amiodarone , lidocaine are first choice of VT storm therapy, especially in the setting of myocardial ischemia.
- Esmolol, sedation, intubation are further choices for treatnig ventricular arrhythmia storm.
- Lidocaine and mexiletine are useful in the context of prolonged QT interval and torsades de pointes due to slightly shortening of QT interval.
- In the presence of polymorphic ventricular tachycardia due to QT prolongation by antiviral therapy, discontinuation the antiviral therapy and infusion of magnesium and correction of hypokalemia and infusion of isoprenaline are recommended.
- In case of recurrent torsades de pointes and bradycardia, arrhythmia can be suppressed by overdrive pacing of temporary pacemaker implantation.
- Echocardiogtaphy is needed if there is new onset of malignant ventricular arrhythmia unrelated to prolonged QTc.
QT prolongation in covid-19 therapy
- QT prolongation has been found in 12% of patients recieving hydroxychloroquine, azithromycin, or both. However, there was no torsades de pointes.[38]
- High dose of chloroquine (600 mg BD for 10 days compared with 450 mg BD for one day then 450mg daily for 4 days) was associated with increased adverse effects.[39]
- High risk patients for QT prolongation include:[40]
- Age> 68 years
- Female sex
- Use of loop diuretic
- Serum potassium level ≤3.5 mEq/l
- Baseline QTc≥ 450 ms
- Acute myocardial infarction
- Use of numbers QT prolongation medications
- Sepsis
- Heart failure
- In the presence of baseline QTc≥ 500 ms, or increased greater than 60 ms after 2-3 hours of administration of hydroxychloroquine or other QT prolongation drugs, risk of torsades de pointes should be considered.[41]
Cardiac medications interaction with covid-19 therapy
- The level of drug that are metabolized by CP450 isoenzyme such as amiodarone, propafenon, flecainide, quinidine, apixaban, rivaroxaban can be increased by administration of lopinavir/ritonavir.
Surgery
Electrophysiology study in an elective procedure and should be planned for management of specific arrhythmias after recovery of covid-19 infection.
Primary Prevention
- Effective measurement for primary prevention of ventricular arrhythmia in covid-19 patients who recieve hydroxychloroquine and azithromycin or other QTc prolongation drugs is determination baseline QTc on ECG.
- If baseline QTc is > 500ms for QRS< 120 ms, or if QTc is >550 ms for QRS> 120ms, or QTc prolonged by 60 ms, these medications should be withheld.[17]
- Primary prevention strategy in covid-19 patients with brugada pattern type 1 is controlling fever by acetaminophen for reducing the risk of ventricular arrhythmia and self isolation.[42]
Secondary Prevention
Secondary prevention for covid-19 associated with arrhythmia is implantation of ICD after recovery of covid-19 in case of ventricular arrhythmia and low LVEF based on the guideline.
References
- ↑ Ruan Q, Yang K, Wang W, Jiang L, Song J (2020). "Correction to: Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China". Intensive Care Med. 46 (6): 1294–1297. doi:10.1007/s00134-020-06028-z. PMC 7131986 Check
|pmc=value (help). PMID 32253449 Check|pmid=value (help). - ↑ Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J; et al. (2020). "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China". JAMA. doi:10.1001/jama.2020.1585. PMC 7042881 Check
|pmc=value (help). PMID 32031570 Check|pmid=value (help). - ↑ Lakkireddy DR, Chung MK, Gopinathannair R, Patton KK, Gluckman TJ, Turagam M; et al. (2020). "Guidance for Cardiac Electrophysiology During the COVID-19 Pandemic from the Heart Rhythm Society COVID-19 Task Force; Electrophysiology Section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association". Circulation. 141 (21): e823–e831. doi:10.1161/CIRCULATIONAHA.120.047063. PMC 7243667 Check
|pmc=value (help). PMID 32228309 Check|pmid=value (help). - ↑ Du Y, Tu L, Zhu P, Mu M, Wang R, Yang P; et al. (2020). "Clinical Features of 85 Fatal Cases of COVID-19 from Wuhan. A Retrospective Observational Study". Am J Respir Crit Care Med. 201 (11): 1372–1379. doi:10.1164/rccm.202003-0543OC. PMC 7258652 Check
|pmc=value (help). PMID 32242738 Check|pmid=value (help). - ↑ Liu K, Fang YY, Deng Y, Liu W, Wang MF, Ma JP; et al. (2020). "Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province". Chin Med J (Engl). 133 (9): 1025–1031. doi:10.1097/CM9.0000000000000744. PMC 7147277 Check
|pmc=value (help). PMID 32044814 Check|pmid=value (help). - ↑ Xu, Zhe; Shi, Lei; Wang, Yijin; Zhang, Jiyuan; Huang, Lei; Zhang, Chao; Liu, Shuhong; Zhao, Peng; Liu, Hongxia; Zhu, Li; Tai, Yanhong; Bai, Changqing; Gao, Tingting; Song, Jinwen; Xia, Peng; Dong, Jinghui; Zhao, Jingmin; Wang, Fu-Sheng (2020). "Pathological findings of COVID-19 associated with acute respiratory distress syndrome". The Lancet Respiratory Medicine. 8 (4): 420–422. doi:10.1016/S2213-2600(20)30076-X. ISSN 2213-2600.
- ↑ Chen, Mao; Prendergast, Bernard; Redwood, Simon; Xiong, Tian-Yuan (2020). "Coronaviruses and the cardiovascular system: acute and long-term implications". European Heart Journal. 41 (19): 1798–1800. doi:10.1093/eurheartj/ehaa231. ISSN 0195-668X.
- ↑ Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G; et al. (2020). "Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic". J Am Coll Cardiol. 75 (18): 2352–2371. doi:10.1016/j.jacc.2020.03.031. PMC 7198856 Check
|pmc=value (help). PMID 32201335 Check|pmid=value (help). - ↑ Lazzerini PE, Laghi-Pasini F, Boutjdir M, Capecchi PL (2019). "Cardioimmunology of arrhythmias: the role of autoimmune and inflammatory cardiac channelopathies". Nat Rev Immunol. 19 (1): 63–64. doi:10.1038/s41577-018-0098-z. PMID 30552387.
- ↑ Clerkin, Kevin J.; Fried, Justin A.; Raikhelkar, Jayant; Sayer, Gabriel; Griffin, Jan M.; Masoumi, Amirali; Jain, Sneha S.; Burkhoff, Daniel; Kumaraiah, Deepa; Rabbani, LeRoy; Schwartz, Allan; Uriel, Nir (2020). "COVID-19 and Cardiovascular Disease". Circulation. 141 (20): 1648–1655. doi:10.1161/CIRCULATIONAHA.120.046941. ISSN 0009-7322.
- ↑ 11.0 11.1 11.2 Coromilas EJ, Kochav S, Goldenthal I, Biviano A, Garan H, Goldbarg S, Kim JH, Yeo I, Tracy C, Ayanian S, Akar J, Singh A, Jain S, Zimerman L, Pimentel M, Osswald S, Twerenbold R, Schaerli N, Crotti L, Fabbri D, Parati G, Li Y, Atienza F, Zatarain E, Tse G, Leung K, Guevara-Valdivia ME, Rivera-Santiago CA, Soejima K, De Filippo P, Ferrari P, Malanchini G, Kanagaratnam P, Khawaja S, Mikhail GW, Scanavacca M, Abrahão Hajjar L, Rizerio B, Sacilotto L, Mollazadeh R, Eslami M, Laleh Far V, Mattioli AV, Boriani G, Migliore F, Cipriani A, Donato F, Compagnucci P, Casella M, Dello Russo A, Coromilas J, Aboyme A, O'Brien CG, Rodriguez F, Wang PJ, Naniwadekar A, Moey M, Kow CS, Cheah WK, Auricchio A, Conte G, Hwang J, Han S, Lazzerini PE, Franchi F, Santoro A, Capecchi PL, Joglar JA, Rosenblatt AG, Zardini M, Bricoli S, Bonura R, Echarte-Morales J, Benito-González T, Minguito-Carazo C, Fernández-Vázquez F, Wan EY (March 2021). "Worldwide Survey of COVID-19-Associated Arrhythmias". Circ Arrhythm Electrophysiol. 14 (3): e009458. doi:10.1161/CIRCEP.120.009458. PMC 7982128 Check
|pmc=value (help). PMID 33554620 Check|pmid=value (help). Vancouver style error: initials (help) - ↑ 12.0 12.1 12.2 O'Connell TF, Bradley CJ, Abbas AE, Williamson BD, Rusia A, Tawney AM, Gaines R, Schott J, Dmitrienko A, Haines DE (January 2021). "Hydroxychloroquine/Azithromycin Therapy and QT Prolongation in Hospitalized Patients With COVID-19". JACC Clin Electrophysiol. 7 (1): 16–25. doi:10.1016/j.jacep.2020.07.016. PMC 7406234 Check
|pmc=value (help). PMID 33478708 Check|pmid=value (help). - ↑ Wang, Dawei; Hu, Bo; Hu, Chang; Zhu, Fangfang; Liu, Xing; Zhang, Jing; Wang, Binbin; Xiang, Hui; Cheng, Zhenshun; Xiong, Yong; Zhao, Yan; Li, Yirong; Wang, Xinghuan; Peng, Zhiyong (2020). "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China". JAMA. 323 (11): 1061. doi:10.1001/jama.2020.1585. ISSN 0098-7484.
- ↑ Kelalis PP, Malek RS (April 1981). "Infundibulopelvic stenosis". J Urol. 125 (4): 568–71. doi:10.1016/s0022-5347(17)55107-1. PMID 7218462.
- ↑ Mulia E, Maghfirah I, Rachmi DA, Julario R (January 2021). "Atrial arrhythmia and its association with COVID-19 outcome: a pooled analysis". Diagnosis (Berl). doi:10.1515/dx-2020-0155. PMID 33470951 Check
|pmid=value (help). Vancouver style error: initials (help) - ↑ 16.0 16.1 Selvaraj V, Bavishi C, Patel S, Dapaah-Afriyie K (July 2021). "Complete heart block associated with Remdesivir in COVID-19: a case report". Eur Heart J Case Rep. 5 (7): ytab200. doi:10.1093/ehjcr/ytab200. PMC 8247739 Check
|pmc=value (help). PMID 34222786 Check|pmid=value (help). - ↑ 17.0 17.1 17.2 Kochav SM, Coromilas E, Nalbandian A, Ranard LS, Gupta A, Chung MK, Gopinathannair R, Biviano AB, Garan H, Wan EY (June 2020). "Cardiac Arrhythmias in COVID-19 Infection". Circ Arrhythm Electrophysiol. 13 (6): e008719. doi:10.1161/CIRCEP.120.008719. PMC 7299099 Check
|pmc=value (help). PMID 32434385 Check|pmid=value (help). - ↑ Gupta AK, Parker BM, Priyadarshi V, Parker J (October 2020). "Cardiac Adverse Events With Remdesivir in COVID-19 Infection". Cureus. 12 (10): e11132. doi:10.7759/cureus.11132. PMC 7682945 Check
|pmc=value (help). PMID 33240723 Check|pmid=value (help). - ↑ Gubitosa JC, Kakar P, Gerula C, Nossa H, Finkel D, Wong K, Khatri M, Ali H (November 2020). "Marked Sinus Bradycardia Associated With Remdesivir in COVID-19: A Case and Literature Review". JACC Case Rep. 2 (14): 2260–2264. doi:10.1016/j.jaccas.2020.08.025. PMC 7598346 Check
|pmc=value (help). PMID 33163977 Check|pmid=value (help). - ↑ 20.0 20.1 Day LB, Abdel-Qadir H, Fralick M (April 2021). "Bradycardia associated with remdesivir therapy for COVID-19 in a 59-year-old man". CMAJ. 193 (17): E612–E615. doi:10.1503/cmaj.210300. PMC 8101980 Check
|pmc=value (help). PMID 33903133 Check|pmid=value (help). - ↑ 21.0 21.1 21.2 Dherange P, Lang J, Qian P, Oberfeld B, Sauer WH, Koplan B, Tedrow U (September 2020). "Arrhythmias and COVID-19: A Review". JACC Clin Electrophysiol. 6 (9): 1193–1204. doi:10.1016/j.jacep.2020.08.002. PMC 7417167 Check
|pmc=value (help). PMID 32972561 Check|pmid=value (help). - ↑ Gandhi, Rajesh T.; Solomon, Caren G.; Lynch, John B.; del Rio, Carlos (2020). "Mild or Moderate Covid-19". New England Journal of Medicine. doi:10.1056/NEJMcp2009249. ISSN 0028-4793.
- ↑ Chang, David; Saleh, Moussa; Gabriels, James; Ismail, Haisam; Goldner, Bruce; Willner, Jonathan; Beldner, Stuart; Mitra, Raman; John, Roy; Epstein, Laurence M. (2020). "Inpatient Use of Ambulatory Telemetry Monitors for COVID-19 Patients Treated With Hydroxychloroquine and/or Azithromycin". Journal of the American College of Cardiology. 75 (23): 2992–2993. doi:10.1016/j.jacc.2020.04.032. ISSN 0735-1097.
- ↑ Inciardi, Riccardo M.; Lupi, Laura; Zaccone, Gregorio; Italia, Leonardo; Raffo, Michela; Tomasoni, Daniela; Cani, Dario S.; Cerini, Manuel; Farina, Davide; Gavazzi, Emanuele; Maroldi, Roberto; Adamo, Marianna; Ammirati, Enrico; Sinagra, Gianfranco; Lombardi, Carlo M.; Metra, Marco (2020). "Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiology. doi:10.1001/jamacardio.2020.1096. ISSN 2380-6583.
- ↑ "Arrhythmia | NHLBI, NIH".
- ↑ Guo, Tao; Fan, Yongzhen; Chen, Ming; Wu, Xiaoyan; Zhang, Lin; He, Tao; Wang, Hairong; Wan, Jing; Wang, Xinghuan; Lu, Zhibing (2020). "Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiology. doi:10.1001/jamacardio.2020.1017. ISSN 2380-6583.
- ↑ Duan K, Liu B, Li C, Zhang H, Yu T, Qu J; et al. (2020). "Effectiveness of convalescent plasma therapy in severe COVID-19 patients". Proc Natl Acad Sci U S A. 117 (17): 9490–9496. doi:10.1073/pnas.2004168117. PMC 7196837 Check
|pmc=value (help). PMID 32253318 Check|pmid=value (help). - ↑ Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW; et al. (2020). "Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area". JAMA. doi:10.1001/jama.2020.6775. PMC 7177629 Check
|pmc=value (help). PMID 32320003 Check|pmid=value (help). - ↑ Giudicessi, John R.; Noseworthy, Peter A.; Friedman, Paul A.; Ackerman, Michael J. (2020). "Urgent Guidance for Navigating and Circumventing the QTc-Prolonging and Torsadogenic Potential of Possible Pharmacotherapies for Coronavirus Disease 19 (COVID-19)". Mayo Clinic Proceedings. 95 (6): 1213–1221. doi:10.1016/j.mayocp.2020.03.024. ISSN 0025-6196.
- ↑ Goyal, Parag; Choi, Justin J.; Pinheiro, Laura C.; Schenck, Edward J.; Chen, Ruijun; Jabri, Assem; Satlin, Michael J.; Campion, Thomas R.; Nahid, Musarrat; Ringel, Joanna B.; Hoffman, Katherine L.; Alshak, Mark N.; Li, Han A.; Wehmeyer, Graham T.; Rajan, Mangala; Reshetnyak, Evgeniya; Hupert, Nathaniel; Horn, Evelyn M.; Martinez, Fernando J.; Gulick, Roy M.; Safford, Monika M. (2020). "Clinical Characteristics of Covid-19 in New York City". New England Journal of Medicine. 382 (24): 2372–2374. doi:10.1056/NEJMc2010419. ISSN 0028-4793.
- ↑ Guo T, Fan Y, Chen M, Wu X, Zhang L, He T; et al. (2020). "Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiol. doi:10.1001/jamacardio.2020.1017. PMC 7101506 Check
|pmc=value (help). PMID 32219356 Check|pmid=value (help). - ↑ Baldi, Enrico; Sechi, Giuseppe M.; Mare, Claudio; Canevari, Fabrizio; Brancaglione, Antonella; Primi, Roberto; Klersy, Catherine; Palo, Alessandra; Contri, Enrico; Ronchi, Vincenza; Beretta, Giorgio; Reali, Francesca; Parogni, Pierpaolo; Facchin, Fabio; Bua, Davide; Rizzi, Ugo; Bussi, Daniele; Ruggeri, Simone; Oltrona Visconti, Luigi; Savastano, Simone (2020). "Out-of-Hospital Cardiac Arrest during the Covid-19 Outbreak in Italy". New England Journal of Medicine. doi:10.1056/NEJMc2010418. ISSN 0028-4793.
- ↑ Shao, Fei; Xu, Shuang; Ma, Xuedi; Xu, Zhouming; Lyu, Jiayou; Ng, Michael; Cui, Hao; Yu, Changxiao; Zhang, Qing; Sun, Peng; Tang, Ziren (2020). "In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, China". Resuscitation. 151: 18–23. doi:10.1016/j.resuscitation.2020.04.005. ISSN 0300-9572.
- ↑ Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M (March 2020). "Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19)". JAMA Cardiol. doi:10.1001/jamacardio.2020.1096. PMID 32219357 Check
|pmid=value (help). - ↑ Alhogbani T (2016). "Acute myocarditis associated with novel Middle east respiratory syndrome coronavirus". Ann Saudi Med. 36 (1): 78–80. doi:10.5144/0256-4947.2016.78. PMC 6074274. PMID 26922692.
- ↑ 36.0 36.1 Kochi, Adriano Nunes; Tagliari, Ana Paula; Forleo, Giovanni Battista; Fassini, Gaetano Michele; Tondo, Claudio (2020). "Cardiac and arrhythmic complications in patients with COVID‐19". Journal of Cardiovascular Electrophysiology. 31 (5): 1003–1008. doi:10.1111/jce.14479. ISSN 1045-3873.
- ↑ Saenz LC, Miranda A, Speranza R, Texeira RA, Rojel U, Enriquez A, Figuereido M (November 2020). "Recommendations for the organization of electrophysiology and cardiac pacing services during the COVID-19 pandemic : Latin American Heart Rhythm Society (LAHRS) in collaboration with: Colombian College Of Electrophysiology, Argentinian Society of Cardiac Electrophysiology (SADEC), Brazilian Society Of Cardiac Arrhythmias (SOBRAC), Mexican Society Of Cardiac Electrophysiology (SOMEEC)". J Interv Card Electrophysiol. 59 (2): 307–313. doi:10.1007/s10840-020-00747-5. PMC 7189002 Check
|pmc=value (help). PMID 32350745 Check|pmid=value (help). - ↑ Ramireddy A, Chugh H, Reinier K, Ebinger J, Park E, Thompson M, Cingolani E, Cheng S, Marban E, Albert CM, Chugh SS (June 2020). "Experience With Hydroxychloroquine and Azithromycin in the Coronavirus Disease 2019 Pandemic: Implications for QT Interval Monitoring". J Am Heart Assoc. 9 (12): e017144. doi:10.1161/JAHA.120.017144. PMC 7429030 Check
|pmc=value (help). PMID 32463348 Check|pmid=value (help). - ↑ Borba M, Val F, Sampaio VS, Alexandre M, Melo GC, Brito M, Mourão M, Brito-Sousa JD, Baía-da-Silva D, Guerra M, Hajjar LA, Pinto RC, Balieiro A, Pacheco A, Santos J, Naveca FG, Xavier MS, Siqueira AM, Schwarzbold A, Croda J, Nogueira ML, Romero G, Bassat Q, Fontes CJ, Albuquerque BC, Daniel-Ribeiro CT, Monteiro WM, Lacerda M (April 2020). "Effect of High vs Low Doses of Chloroquine Diphosphate as Adjunctive Therapy for Patients Hospitalized With Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection: A Randomized Clinical Trial". JAMA Netw Open. 3 (4): e208857. doi:10.1001/jamanetworkopen.2020.8857. PMID 32330277 Check
|pmid=value (help). Vancouver style error: initials (help) - ↑ Castagna A, Ruotolo G, Manzo C (December 2020). "Hydroxychloroquine and QT Prolongation in Older Patients with Rheumatic Diseases: Who is afraid of the Boogeyman? We are not!". Mediterr J Rheumatol. 31 (4): 433–435. doi:10.31138/mjr.31.4.433. PMC 7841093 Check
|pmc=value (help). PMID 33521580 Check|pmid=value (help). - ↑ Cheung CC, Davies B, Gibbs K, Laksman ZW, Krahn AD (July 2020). "Multilead QT Screening Is Necessary for QT Measurement: Implications for Management of Patients in the COVID-19 Era". JACC Clin Electrophysiol. 6 (7): 878–880. doi:10.1016/j.jacep.2020.04.001. PMC 7141442 Check
|pmc=value (help). PMID 32703574 Check|pmid=value (help). - ↑ Wu CI, Postema PG, Arbelo E, Behr ER, Bezzina CR, Napolitano C; et al. (2020). "SARS-CoV-2, COVID-19, and inherited arrhythmia syndromes". Heart Rhythm. doi:10.1016/j.hrthm.2020.03.024. PMC 7156157 Check
|pmc=value (help). PMID 32244059 Check|pmid=value (help).