Langerhans cell histiocytosis pathophysiology
|
Langerhans cell histiocytosis Microchapters |
|
Differentiating Langerhans cell histiocytosis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Langerhans cell histiocytosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Langerhans cell histiocytosis pathophysiology |
|
Directions to Hospitals Treating Langerhans cell histiocytosis |
|
Risk calculators and risk factors for Langerhans cell histiocytosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Haytham Allaham, M.D. [2]
Overview
Langerhans cell histiocytosis arises from epidermal dendritic cells (Langerhans cells), which are normally involved in the process of antigen presentation to lymphocytic cells. Langerhans cells originally arise from the bone marrow, then the cells migrate to other organs such as the skin, lymph nodes, and lungs. The exact pathogenesis of Langerhans cell histiocytosis is not fully understood. It is thought that Langerhans cell histiocytosis is the result of either a true neoplastic process or a reactive immune condition. Genes commonly involved in the pathogenesis of Langerhans cell histiocytosis include BRAF gene and MAP2K1 gene. On gross pathology, scaly erythema, red papules, and extensive eruptions located on the scalp are characteristic finding of Langerhans cell histiocytosis. Characteristic findings of Langerhans cell histiocytosis on light microscopy may include clusters of dendritic cells with kidney-shaped nucleus and abundant foamy cytoplasm. On electron microscopy Langerhans cell histiocytosis is characterized by Birbeck granules, which are electron dense, cytoplasmic, tennis racket-like bodies. On immunohistochemistry Langerhans cell histiocytosis is characterized by positivity to CD1a, S100, and CD207 (langerin).[1][2][3][4][5][6]
Pathogenesis
- Langerhans cell histiocytosis arises from epidermal dendritic cells, which are normally involved in the process of antigen presentation to lymphocytic cells.[7][8][9]
Origin of Langerhans Cells
- Langerhans cells originally arise from the bone marrow, then the cells migrate to other organs such as:[10][11][12]
Organ Involvement in Langerhans Cell Histiocytosis
- Organ involvement is variable among patients with Langerhans cell histiocytosis. The disease process may range from an isolated cutaneous or bone involvement to a life-threatening multi-system condition.
- The skeletal distribution of Langerhans cell histiocytosis involves the following sites:[13][14][15]
Disregulation of Immune Response
- The exact pathogenesis of Langerhans cell histiocytosis is not fully understood. It is thought that Langerhans cell histiocytosis is the result of either a true neoplastic process or a reactive immune condition.
- Facts consistent with the neoplastic process hypothesis include the following:
- The infiltration of organs by monoclonal population of pathologic cells
- The presence of specific recurrent cytogenetic and genomic abnormalities
- The successful treatment of a subset of disseminated Langerhans cell histiocytosis using chemotherapeutic regimens
- Facts consistent with the reactive immune condition hypothesis include the following:
- The evidence of spontaneous remissions that may occur among certain cases of Langerhans cell histiocytosis
- The extensive secretion of multiple cytokines by dendritic cells and bystander-cells (a phenomenon known as cytokine storm)
- The favorable prognosis and relatively good survival rate among patients with no organ dysfunction
Non-Specific Inflammatory Response
- The uncontrolled monoclonal proliferation of Langerhans cells will initiate a non-specific inflammatory response, which will lead to the accumulation of various immune system cells such as:[1][2][5][6]
- Eosinophils
- Macrophages
- Lymphocytes
- Multinucleated giant cells
Bone Marrow Failure
- Langerhans cell histiocytosis may result in bone marrow failure due to malignant cell infiltration of the bone marrow. The manifestation of bone marrow failure among patients with Langerhans cell histiocytosis may include:[3][4]
- Anemia
- Recurrent bleeding
- Recurrent infections
Tissue Infiltration
- The infiltration of the hypothalamic-pituitary axis by Langerhans cells will lead to a deficiency in both anterior and posterior pituitary hormones, which may result in:
- Central diabetes insipidus
- Growth retardation
- Delayed puberty
- Langerhans cell histiocytosis may also infiltrate the lymph nodes, spleen, and liver.
Genetics
- Development of Langerhans cell histiocytosis is the result of multiple genetic mutations.[7][8][9]
- Genes commonly involved in the pathogenesis of Langerhans cell histiocytosis include:
- BRAF BRAF V600E gene mutation located on Chromosome 7
- MAP2K1 gene mutation located on Chromosome 15
- Less common genetic mutations involved in the pathogenesis of Langerhans cell histiocytosis include:[16][17]
- ARAF gene mutation located on the X-chromosome
- ERBB3 gene mutation located on chromosome 12
- The aforementioned genetic mutations, which occur among patients of Langerhans cell histiocytosis, will lead to constitutive activation of downstream extracellular signal-related kinase (ERK) and mitogen-activated protein kinase (MEK).
- Induction of ERK activation is a universal feature that is found in most of the cases of Langerhans cell histiocytosis.
- The MAPK/ERK pathway (also known as the Ras-RAF-MEK-ERK pathway) is a cascade of proteins that transmit cellular signal from receptors found on the surface of the cell to the nucleus, this ultimately results in the activation of cellular DNA production.[18]
Associated Conditions
- Langerhans cell histiocytosis is associated with a number of syndromes such as Hashimoto-Pritzker disease.[3]
Gross Pathology
- On gross pathology, scaly erythema, red papules, and extensive eruptions located on the scalp are characteristic finding of Langerhans cell histiocytosis.[3]
- The image below demonstrates the cutaneous scalp lesions observed among Langerhans cell histiocytosis patients:
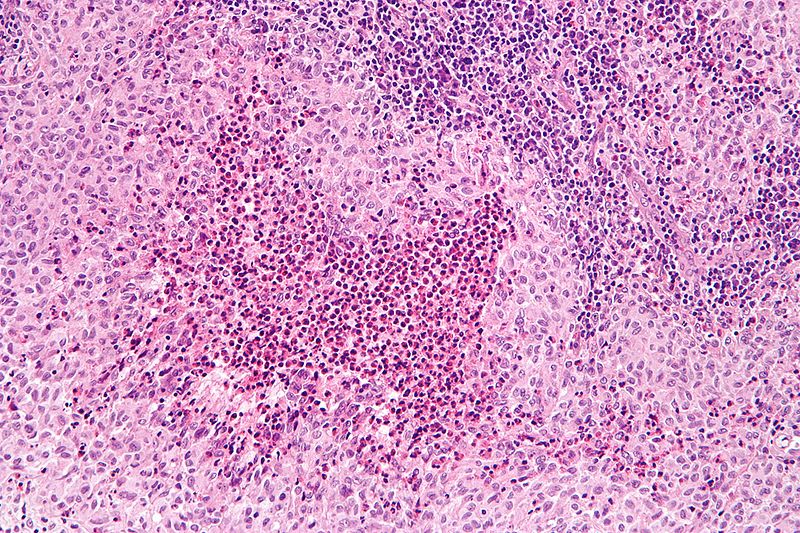
Microscopic Pathology
- Clusters of dendritic cells
- Kidney-shaped nucleus
- Abundant foamy cytoplasm
- Fine, granular chromatin pattern
- Prominent eosinophils
- Fibrosis
- Other inflammatory cells may be present (neutrophils, plasma cells, and multinucleated giant cells)
- On electron microscopy Langerhans cell histiocytosis is characterized by Birbeck granules, which are electron dense, cytoplasmic, tennis racket-like bodies.[1][2][3][4][5][6]
- On immunohistochemistry Langerhans cell histiocytosis is characterized by:
- CD1a +ve
- S100 +ve
- CD207 (langerin) +ve
Gallery
Illustrated below is a series of microscopic images demonstrating Langerhans cell histiocytosis:[6]
References
- ↑ 1.0 1.1 1.2 Collin M, Bigley V, McClain KL, Allen CE (2015). "Cell(s) of Origin of Langerhans Cell Histiocytosis". Hematol Oncol Clin North Am. 29 (5): 825–38. doi:10.1016/j.hoc.2015.06.003. PMC 4699587. PMID 26461145.
- ↑ 2.0 2.1 2.2 Langerhans Cell Histiocytosis Treatment (PDQ®): Health Professional Version. National Cancer Institute (2015) http://www.cancer.gov/types/langerhans/hp/langerhans-treatment-pdq Accessed on February, 3 2016
- ↑ 3.0 3.1 3.2 3.3 3.4 Langerhans cell histiocytosis. Wikipedia (2015) https://en.wikipedia.org/wiki/Langerhans_cell_histiocytosis Accessed on February, 2 2016
- ↑ 4.0 4.1 4.2 Badalian-Very G, Vergilio JA, Fleming M, Rollins BJ (2013). "Pathogenesis of Langerhans cell histiocytosis". Annu Rev Pathol. 8: 1–20. doi:10.1146/annurev-pathol-020712-163959. PMID 22906202.
- ↑ 5.0 5.1 5.2 Langerhans cell histiocytosis. Radiopeadia (2015) http://radiopaedia.org/articles/langerhans-cell-histiocytosis Accessed on February, 3 2016
- ↑ 6.0 6.1 6.2 6.3 Langerhans cell histiocytosis. Libre Pathology (2015) http://librepathology.org/wiki/index.php/Langerhans_cell_histiocytosis#cite_note-10 Accessed on February, 3 2016
- ↑ 7.0 7.1 7.2 DiCaprio MR, Roberts TT (2014). "Diagnosis and Management of Langerhans Cell Histiocytosis". J Am Acad Orthop Surg. 22 (10): 643–652. doi:10.5435/JAAOS-22-10-643. PMID 25281259.
- ↑ 8.0 8.1 8.2 Grana N (2014). "Langerhans cell histiocytosis". Cancer Control. 21 (4): 328–34. PMID 25310214.
- ↑ 9.0 9.1 9.2 Harmon CM, Brown N (2015). "Langerhans Cell Histiocytosis: A Clinicopathologic Review and Molecular Pathogenetic Update". Arch Pathol Lab Med. 139 (10): 1211–4. doi:10.5858/arpa.2015-0199-RA. PMID 26414464.
- ↑ Tamaki K, Stingl G, Katz SI (May 1980). "The origin of Langerhans cells". J. Invest. Dermatol. 74 (5): 309–11. PMID 7391603.
- ↑ Collin M, Milne P (January 2016). "Langerhans cell origin and regulation". Curr. Opin. Hematol. 23 (1): 28–35. doi:10.1097/MOH.0000000000000202. PMC 4685746. PMID 26554892.
- ↑ Jaitley S, Saraswathi T (May 2012). "Pathophysiology of Langerhans cells". J Oral Maxillofac Pathol. 16 (2): 239–44. doi:10.4103/0973-029X.99077. PMID 22923897.
- ↑ Munn S, Chu AC (April 1998). "Langerhans cell histiocytosis of the skin". Hematol. Oncol. Clin. North Am. 12 (2): 269–86. PMID 9561900.
- ↑ Zhang XH, Zhang J, Chen ZH, Sai K, Chen YS, Wang J, Ke C, Guo CC, Chen ZP, Mou YG (April 2017). "Langerhans cell histiocytosis of skull: a retrospective study of 18 cases". Ann Palliat Med. 6 (2): 159–164. doi:10.21037/apm.2016.11.04. PMID 28061539.
- ↑ Khung S, Budzik JF, Amzallag-Bellenger E, Lambilliote A, Soto Ares G, Cotten A, Boutry N (October 2013). "Skeletal involvement in Langerhans cell histiocytosis". Insights Imaging. 4 (5): 569–79. doi:10.1007/s13244-013-0271-7. PMC 3781243. PMID 23907805.
- ↑ ARAF. Wikipedia (2015) https://en.wikipedia.org/wiki/ARAF Accessed on February, 3 2016
- ↑ ERBB3. Wikipedia (2015) https://en.wikipedia.org/wiki/ERBB3 Accessed on February, 3 2016
- ↑ MAPK/ERK pathway. Wikipedia (2015) https://en.wikipedia.org/wiki/MAPK/ERK_pathway Accessed on February, 3 2016