Ketorolac tromethamine (nasal)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aparna Vuppala, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Ketorolac tromethamine (nasal) is a analgesic that is FDA approved for the treatment of severe pain that requires analgesia at the opioid level. Common adverse reactions include edema, hypertension, pruritus, rash, sweating, abdominal pain, constipation, diarrhea, flatulence, heartburn, indigestion, nausea, stomatitis, vomiting, anemia, purpura, dizziness, headache, somnolence, iritis.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- SPRIX is indicated in adult patients for the short term (up to 5 days) management of moderate to moderately severe pain that requires analgesia at the opioid level.
Dosage
- Limitations of Use
- The total duration of use of SPRIX alone or sequentially with other formulations of ketorolac (IM/IV or oral) must not exceed 5 days because of the potential for increasing the frequency and severity of adverse reactions associated with the recommended doses. Treat patients for the shortest duration possible, and do not exceed 5 days of therapy with SPRIX.
- Do not use SPRIX concomitantly with other formulations of ketorolac or other NSAIDs .
- SPRIX has not been shown to be safe and effective in pediatric patients 17 years of age and younger.
- Administration
- SPRIX is not an inhaled product. Do not inhale when administering this product.
- Instruct patients to administer as follows:
- First hold the finger flange with fingers, and remove the clear plastic cover with opposite hand; then remove the blue plastic safety clip. Keep the clear plastic cover; and throw away the blue plastic safety clip.
- Before using the bottle for the FIRST time, activate the pump. To activate the pump, hold the bottle at arm’s length away from the body with index finger and middle finger resting on the top of the finger flange and thumb supporting the base.
- Press down evenly and release the pump 5 times. Patient may not see a spray the first few times he/she presses down.
- The bottle is now ready to use. There is no need to activate the pump again if more doses are used from the bottle.
- It’s important to get the medication to the correct place in the nose so it will be most effective.
- Blow nose gently to clear nostrils.
- Sit up straight or stand. Tilt head slightly forward.
- Insert the tip of the container into your right nostril.
- Point the container away from the center of your nose
- Hold your breath and spray once into your right nostril, pressing down evenly on both sides
- Immediately after administration, resume breathing through mouth to reduce expelling the product. Also pinch the nose to help retain the spray if it starts to drip.
- Blow nose gently to clear nostrils.
- If only one spray per dose is prescribed, administration is complete; skip to Step 5 below.
- If a dose of 2 sprays is prescribed, repeat the process in Step 3 for the left nostril. Again, be sure to point the spray away from the center of nose. Spray once into the left nostril.
- Replace the clear plastic cover and place the bottle in a cool, dry location out of direct sunlight, such as inside a medication cabinet. Keep out of reach of children.
- Adult Patients < 65 Years of Age
- The recommended dose is 31.5 mg SPRIX (one 15.75 mg spray in each nostril) every 6 to 8 hours. The maximum daily dose is 126 mg (four doses).
- Reduced Doses for Special Populations
- For patients ≥ 65 years of age, renally impaired patients, and adult patients less than 50 kg (110 lbs), the recommended dose is 15.75 mg SPRIX (one 15.75 mg spray in only one nostril) every 6 to 8 hours. The maximum daily dose is 63 mg (four doses).
- Discard Used SPRIX Bottle after 24 Hours
- Do not use any single SPRIX bottle for more than one day as it will not deliver the intended dose after 24 hours. Therefore, the bottle must be discarded no more than 24 hours after taking the first dose, even if the bottle still contains some liquid.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Ketorolac tromethamine (nasal) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Ketorolac tromethamine (nasal) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Ketorolac tromethamine (nasal) in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Ketorolac tromethamine (nasal) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Ketorolac tromethamine (nasal) in pediatric patients.
Contraindications
- Known hypersensitivity to ketorolac tromethamine
- Use in patients with active peptic ulcer disease, in patients with recent gastrointestinal bleeding or perforation, and in patients with a history of peptic ulcer disease or gastrointestinal bleeding
- Use in patients with a history of asthma, urticaria, or other allergic-type reactions after taking aspirin or other NSAIDs
- Use as a prophylactic analgesic before any major surgery
- Use during the perioperative period in the setting of coronary artery bypass graft (CABG) surgery
- Use in patients with advanced renal disease or patients at risk for renal failure due to volume depletion
- Use in labor and delivery. Through its prostaglandin synthesis inhibitory effect, ketorolac may adversely affect fetal circulation and inhibit uterine contractions, thus increasing the risk of uterine hemorrhage
- Use in patients with suspected or confirmed cerebrovascular bleeding, hemorrhagic diathesis, incomplete hemostasis, or those for whom hemostasis is critical
- Known hypersensitivity to aspirin or to other NSAIDs Known hypersensitivity to ethylenediamine tetraacetic acid (EDTA)
- Concomitant use with probenecid
- Concomitant use with pentoxifylline
Warnings
- Limitations of Use
- The total duration of use of SPRIX alone or sequentially with other forms of ketorolac is not to exceed 5 days. SPRIX must not be used concomitantly with other forms of ketorolac or other NSAIDs
- Gastrointestinal (GI) Effects - Risk of Ulceration, Bleeding, and Perforation
- SPRIX is contraindicated in patients with previously documented peptic ulcers and/or GI bleeding . Ketorolac tromethamine can cause serious GI adverse events including bleeding, ulceration, and perforation of the stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with ketorolac.
- Only one in five patients who develop a serious upper GI adverse event on NSAID therapy is symptomatic. Minor upper GI problems, such as dyspepsia, are common and may also occur at any time during NSAID therapy. The incidence and severity of GI complications increases with increasing dose of, and duration of treatment with, ketorolac. Even short-term therapy is not without risk. In addition to past history of ulcer disease, other factors that increase the risk for GI bleeding in patients treated with NSAIDs include concomitant use of oral corticosteroids or anticoagulants, longer duration of NSAID therapy, smoking, use of alcohol, older age, and poor general health status. Most spontaneous reports of fatal GI events are in elderly or debilitated patients, and therefore, special care should be taken in treating this population.
- To minimize the potential risk for an adverse GI event, the lowest effective dose should be used for the shortest possible duration. Remain alert for signs and symptoms of GI ulceration and bleeding during NSAID therapy, and promptly initiate additional evaluation and treatment if a serious GI adverse event is suspected. This should include discontinuation of SPRIX until a serious GI adverse event is ruled out. For high risk patients, consider alternate therapies that do not involve NSAIDs. Use great care when giving SPRIX to patients with a history of inflammatory bowel disease (ulcerative colitis, Crohn's disease) as their condition may be exacerbated.
- Hematological Effects
- Because prostaglandins play an important role in hemostasis and NSAIDs affect platelet aggregation as well, use caution with use of ketorolac tromethamine in patients who have coagulation disorders, and monitor these patients carefully. The effects of NSAIDs other than aspirin on platelet function are reversible. Patients on therapeutic doses of anticoagulants (e.g., heparin or dicumarol derivatives) have an increased risk of bleeding complications if given ketorolac tromethamine concurrently; therefore, administer such concomitant therapy only with extreme caution. The concurrent use of ketorolac tromethamine and therapy that affects hemostasis, including prophylactic low dose heparin (2500 to 5000 units q12h), warfarin and dextrans, has not been studied extensively, but may also be associated with an increased risk of bleeding. Until data from such studies are available, carefully weigh the benefits against the risks and use such concomitant therapy in these patients only with extreme caution. Monitor patients receiving therapy that affects hemostasis closely.
- In clinical trials, serious adverse events related to bleeding were more common in patients treated with SPRIX than placebo. In clinical trials and in postmarketing experience with ketorolac IV and IM dosing, postoperative hematomas and other signs of wound bleeding have been reported in association with peri-operative use. Therefore, use SPRIX with caution in the postoperative setting when hemostasis is critical.
- Anemia is sometimes seen in patients receiving NSAIDs. This may be due to fluid retention, occult or gross GI blood loss, or an incompletely described effect upon erythropoiesis. Do not use SPRIX in patients for whom hemostasis is critical
- Renal Effects
- Ketorolac and its metabolites are eliminated primarily by the kidneys. Patients with reduced creatinine clearance will have diminished clearance of the drug . SPRIX is contraindicated in patients with advanced renal impairment
- In patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion, administration of an NSAID may cause a dose-dependent reduction in prostaglandin formation and renal blood flow, which may precipitate overt renal decompensation. Decreased intravascular volume such as when oral intake is poor increases the risks of renal toxicity with NSAIDs. Therefore, patients treated with SPRIX should be adequately hydrated. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
- Use SPRIX with caution in patients with impaired renal function, heart failure, liver dysfunction, those taking diuretics or ACE inhibitors, and the elderly. Assess the risks and benefits prior to giving SPRIX to these patients, and follow these patients closely during SPRIX therapy. Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury such as interstitial nephritis and nephrotic syndrome.
- Anaphylactoid Reactions
- As with other NSAIDs, anaphylactoid reactions may occur in patients with or without a history of allergic reactions to aspirin or NSAIDs and in patients without known prior exposure to ketorolac. SPRIX should be discontinued immediately in patients with allergic reactions. SPRIX should not be given to patients with the aspirin triad. This symptom complex typically occurs in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit severe, potentially fatal bronchospasm after taking aspirin or other NSAIDs. Emergency help should be sought in cases where an anaphylactoid reaction occurs.
- Cardiovascular Effects
- Cardiovascular (CV) Thrombotic Events
- Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious CV thrombotic events, myocardial infarction and stroke, which can be fatal. All NSAIDs, both COX-2 selective and nonselective, may have a similar risk. Patients with known CV disease or risk factors for CV disease may be at greater risk. To minimize the potential risk for an adverse CV event in patients treated with an NSAID, the lowest effective dose should be used for the shortest duration possible. Physicians and patients should remain alert for the development of such events, even in the absence of previous CV symptoms. Patients should be informed about the signs and/or symptoms of serious CV events and the steps to take if they occur. There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID increases the risk of serious GI events. Two large, controlled clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10-14 days following CABG surgery found an increased incidence of myocardial infarction and stroke
- Hypertension
- Congestive Heart Failure and Edema
- Fluid retention, edema, retention of NaCl, oliguria, and elevations of serum urea nitrogen and creatinine have been reported in clinical trials with ketorolac. Therefore, only use SPRIX very cautiously in patients with cardiac decompensation or similar conditions.
- Skin Reactions
- NSAIDs, including ketorolac, can cause serious skin adverse events such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Inform patients about the signs and symptoms of serious skin manifestations, and discontinue use of the drug at the first appearance of skin rash or any other sign of hypersensitivity .
- Pregnancy
- Starting at 30 weeks gestation, SPRIX can cause fetal harm when administered to a pregnant woman due to an increased risk of premature closure of the ductus arteriosus. If SPRIX is used at or after 30 weeks gestation, the patient should be apprised of the potential hazard to a fetus
- Hepatic Effects
- Use SPRIX with caution in patients with impaired hepatic function or a history of liver disease. Borderline elevations of one or more liver tests may occur in up to 15% of patients taking NSAIDs, including ketorolac. These laboratory abnormalities may progress, may remain unchanged, or may be transient with continuing therapy. Notable elevations of ALT or AST (approximately three or more times the upper limit of normal) have been reported in approximately 1% of patients in clinical trials with NSAIDs. In addition, rare cases of severe hepatic reactions, including jaundice, fulminant hepatitis, liver necrosis, and hepatic failure, some of them with fatal outcomes, have been reported
- Evaluate patients with symptoms and/or signs suggesting liver dysfunction, or in whom an abnormal liver test has occurred, for evidence of the development of a more severe hepatic reaction while on therapy with SPRIX. If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), discontinue SPRIX.
- Inflammation and Fever
- The pharmacological activity of SPRIX in reducing inflammation and fever may diminish the utility of these diagnostic signs in detecting infections.
- Preexisting Asthma
- Patients with asthma may have aspirin-sensitive asthma. The use of aspirin in patients with aspirin-sensitive asthma has been associated with severe bronchospasm which can be fatal. Since cross reactivity, including bronchospasm, between aspirin and other NSAIDs has been reported in such aspirin-sensitive patients, do not administer SPRIX to patients with this form of aspirin sensitivity, and use with caution in patients with preexisting asthma
- Eye Exposure
- Avoid contact of SPRIX with the eyes. If eye contact occurs, wash out the eye with water or saline, and consult a physician if irritation persists for more than an hour.
Adverse Reactions
Clinical Trials Experience
- The following serious adverse reactions are discussed elsewhere in the labeling:
- Gastrointestinal effects
- Hemorrhage
- Renal effects
- Anaphylactoid reactions
- Cardiovascular thrombotic events
- Hypertension
- Congestive heart failure and edema
- Serious skin reactions
- Hepatic effects
- The most frequently reported adverse reactions were related to local symptoms, i.e., nasal discomfort or irritation. These reactions were generally mild and transient in nature.
- The most common drug-related adverse events leading to premature discontinuation were nasal discomfort or nasal pain (rhinalgia).
Experience from SPRIX Clinical Studies
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The data described below reflect exposure to SPRIX in patients enrolled in placebo-controlled efficacy studies of acute pain following major surgery. The studies enrolled 828 patients (183 men, 645 women) ranging from 18 years to over 75 years of age.
- The patients in the postoperative pain studies had undergone major abdominal, orthopedic, gynecologic, or other surgery; 455 patients received SPRIX (31.5 mg) three or four times a day for up to 5 days, and 245 patients received placebo. Most patients were receiving concomitant opioids, primarily PCA morphine.
- In controlled clinical trials in major surgery, primarily knee and hip replacements and abdominal hysterectomies, seven patients (N=455, 1.5%) treated with SPRIX experienced serious adverse events of bleeding (4 patients) or hematoma (3 patients) at the operative site versus one patient (N=245, 0.4%) treated with placebo (hematoma). Six of the seven patients treated with SPRIX underwent a surgical procedure and/or blood transfusion and the placebo patient subsequently required a blood transfusion.
- Adverse Reactions Reported in Clinical Trials with Other Dosage Forms of Ketorolac or Other NSAIDs
- Adverse reaction rates increase with higher doses of ketorolac. It is necessary to remain alert for the severe complications of treatment with ketorolac, such as GI ulceration, bleeding, and perforation, postoperative bleeding, acute renal failure, anaphylactic and anaphylactoid reactions, and liver failure. These complications can be serious in certain patients for whom ketorolac is indicated, especially when the drug is used inappropriately.
- In patients taking ketorolac or other NSAIDs in clinical trials, the most frequently reported adverse experiences in approximately 1% to 10% of patients are:
- Gastrointestinal (GI) experiences including:
- Additional adverse experiences reported occasionally (<1% in patients taking ketorolac or other NSAIDs in clinical trials) include:
- Body as a Whole: fever, infection, sepsis
- Cardiovascular System: congestive heart failure, palpitation, pallor, tachycardia, syncope
- Digestive System: anorexia, dry mouth, eructation, esophagitis, excessive thirst, gastritis, glossitis, hematemesis, hepatitis, increased appetite, jaundice, melena, rectal bleeding
- Hemic and Lymphatic: ecchymosis, eosinophilia, epistaxis, leukopenia, thrombocytopenia
- Metabolic and Nutritional: weight change
- Nervous System: abnormal dreams, abnormal thinking, anxiety, asthenia, confusion, depression, euphoria, extrapyramidal symptoms, hallucinations, hyperkinesis, inability to concentrate, insomnia, nervousness, paresthesia, somnolence, stupor, tremors, vertigo, malaise
- Respiratory: asthma, dyspnea, pulmonary edema, rhinitis
- Special Senses: abnormal taste, abnormal vision, blurred vision, hearing loss
Postmarketing Experience
- Adverse Reactions from Postmarketing Experience with Other Dosage Forms of Ketorolac or Other NSAIDs
- Other observed reactions (reported from postmarketing experience in patients taking ketorolac or other NSAIDs) are:
- Body as a Whole: angioedema, death, hypersensitivity reactions such as anaphylaxis, anaphylactoid reaction, laryngeal edema, tongue edema, myalgia
- Cardiovascular: arrhythmia, bradycardia, chest pain, flushing, hypotension, myocardial infarction, vasculitis
- Dermatologic: exfoliative dermatitis, erythema multiforme, Lyell's syndrome, bullous reactions including Stevens-Johnson syndrome and toxic epidermal necrolysis
- Gastrointestinal: acute pancreatitis, liver failure, ulcerative stomatitis, exacerbation of inflammatory bowel disease (ulcerative colitis, Crohn's disease)
- Hemic and Lymphatic: agranulocytosis, aplastic anemia, hemolytic anemia, lymphadenopathy, pancytopenia, postoperative wound hemorrhage (rarely requiring blood transfusion)
- Metabolic and Nutritional: hyperglycemia, hyperkalemia, hyponatremia
- Nervous System: aseptic meningitis, convulsions, coma, psychosis
- Respiratory: bronchospasm, respiratory depression, pneumonia
- Special Senses: conjunctivitis
- Urogenital: flank pain with or without hematuria and/or azotemia, hemolytic uremic syndrome
Drug Interactions
- Ketorolac is highly bound to human plasma protein (mean 99.2%). There is no evidence in animal or human studies that ketorolac induces or inhibits hepatic enzymes capable of metabolizing itself or other drugs.
- Warfarin, Digoxin, Salicylate, and Heparin
- The in vitro binding of warfarin to plasma proteins is only slightly reduced by ketorolac (99.5% control vs. 99.3%) when ketorolac plasma concentrations reach 5 to 10 mcg/mL. Ketorolac does not alter digoxin protein binding. In vitro studies indicate that, at therapeutic concentrations of salicylate (300 mcg/mL), the binding of ketorolac was reduced from approximately 99.2% to 97.5%, representing a potential twofold increase in unbound ketorolac plasma levels. Therapeutic concentrations of digoxin, warfarin, ibuprofen, naproxen, piroxicam, acetaminophen, phenytoin, and tolbutamide did not alter ketorolac protein binding.
- The effects of warfarin and NSAIDs, in general, on GI bleeding are synergistic, such that the users of both drugs together have a risk of serious GI bleeding higher than the users of either drug alone.
- Aspirin
- When ketorolac is administered with aspirin, its protein binding is reduced, although the clearance of free ketorolac is not altered. The clinical significance of this interaction is not known; however, as with other NSAIDs, concomitant administration of SPRIX and aspirin is not generally recommended because of the potential of increased adverse effects
- Diuretics
- Clinical studies, as well as postmarketing observations, have shown that ketorolac can reduce the natriuretic effect of furosemide and thiazides in some patients. This response has been attributed to inhibition of renal prostaglandin synthesis. During concomitant therapy with SPRIX, observe the patient closely for signs of renal failure as well as to assure diuretic efficacy.
- Probenecid
- Concomitant administration of oral ketorolac and probenecid resulted in decreased clearance and volume of distribution of ketorolac and significant increases in ketorolac plasma levels (total AUC increased approximately threefold from 5.4 to 17.8 mcg/h/mL), and terminal half-life increased approximately twofold from 6.6 to 15.1 hours. Therefore, concomitant use of SPRIX and probenecid is contraindicated.
- Lithium
- NSAIDs have produced an elevation of plasma lithium levels and a reduction in renal lithium clearance. The mean minimum lithium concentration increased 15%, and the renal clearance was decreased by approximately 20%. These effects have been attributed to inhibition of renal prostaglandin synthesis by the NSAID. Thus, when SPRIX and lithium are administered concurrently, observe patients carefully for signs of lithium toxicity.
- Methotrexate
- NSAIDs have been reported to competitively inhibit methotrexate accumulation in rabbit kidney slices. This may indicate that they could enhance the toxicity of methotrexate. Use caution when SPRIX is administered concomitantly with methotrexate.
- ACE Inhibitors/Angiotensin II Receptor Antagonists
- Concomitant use of ACE inhibitors and/or angiotensin II receptor antagonists may increase the risk of renal impairment, particularly in volume-depleted patients. Reports suggest that NSAIDs may diminish the antihypertensive effect of ACE inhibitors and/or angiotensin II receptor antagonists. Consider this interaction in patients taking SPRIX concomitantly with ACE inhibitors and/or angiotensin II receptor antagonists .
- Antiepileptic Drugs
- Sporadic cases of seizures have been reported during concomitant use of ketorolac and antiepileptic drugs (phenytoin, carbamazepine).
- Psychoactive Drugs
- Hallucinations have been reported when ketorolac was used in patients taking psychoactive drugs (fluoxetine, thiothixene, alprazolam).
- Pentoxifylline
- When ketorolac is administered concurrently with pentoxifylline, there is an increased tendency to bleeding. Therefore, concomitant use of SPRIX and Pentoxifylline is contraindicated
- Nondepolarizing Muscle Relaxants
- In postmarketing experience there have been reports of a possible interaction between ketorolac and nondepolarizing muscle relaxants that resulted in apnea. The concurrent use of ketorolac with muscle relaxants has not been formally studied.
- Selective Serotonin Reuptake Inhibitors (SSRIs)
- There is an increased risk of gastrointestinal bleeding when selective serotonin reuptake inhibitors (SSRIs) are combined with NSAIDs. Use caution when SPRIX is administered concomitantly with SSRIs.
- Fluticasone
- The rate and extent of absorption of ketorolac from SPRIX administration (31.5 mg dose) were assessed in subjects with allergic rhinitis before and after the administration of a single daily dose of 200 mcg (as 2 x 50 mcg in each nostril) of fluticasone propionate nasal spray for 7 consecutive days. There was no effect on the pharmacokinetic characteristics of SPRIX that can be considered clinically significant.
- Oxymetazoline
- The rate and extent of absorption of ketorolac from SPRIX administration were assessed in subjects with allergic rhinitis before and 30 min after a single dose (3 sprays in each nostril) of oxymetazoline hydrochloride nasal spray. There was no effect on the pharmacokinetic characteristics of SPRIX that can be considered clinically significant
Use in Specific Populations
Pregnancy
- Teratogenic Effects: Pregnancy Category C prior to 30 weeks gestation; Category D starting at 30 weeks gestation.
- SPRIX can cause fetal harm when administered to a pregnant woman. Human data demonstrate that use of NSAIDs at or after 30 weeks gestation increases the risk of premature closure of the ductus arteriosus. If SPRIX is used at or after 30 weeks gestation, the patient should be apprised of the potential hazard to a fetus. There are no adequate, well-controlled studies in pregnant women. Prior to 30 weeks gestation, SPRIX should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Reproduction studies have been performed during organogenesis using daily oral doses of ketorolac tromethamine at 3.6 mg/kg (0.6 times the human systemic exposure at the recommended maximum IN dose of 31.5 mg qid, based on area-under-the-plasma-concentration curve [AUC]) in rabbits and at 10 mg/kg (1.7 times the human AUC) in rats. These studies did not reveal evidence of teratogenicity or other adverse developmental outcomes. However, because animal dosing was limited by maternal toxicity, these studies do not adequately assess ketorolac's potential to cause adverse developmental outcomes in humans.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Ketorolac tromethamine (nasal) in women who are pregnant.
Labor and Delivery
- The effects of SPRIX on labor and delivery in pregnant women are unknown. In rat studies, maternal exposure to NSAIDs, as with other drugs known to inhibit prostaglandin synthesis, increased the incidence of dystocia and delayed parturition, and decreased pup survival.
Nursing Mothers
- Ketorolac is excreted in human milk. Limited data from one published study involving ten nursing mothers 2-6 days postpartum showed low levels of ketorolac in breast milk. Levels were undetectable (less than 5 ng/mL) in 4 of the patients. After a single administration of 10 mg ketorolac, the maximum milk concentration observed was 7.3 ng/mL, and the maximum milk to plasma ratio was 0.037. After 1 day of dosing (10 mg every 6 hours), the maximum milk concentration was 7.9 ng/mL, and the maximum milk-to-plasma ratio was 0.025. Assuming a daily intake of 400-1000 mL of human milk per day and a maternal body weight of 60 kg, the calculated maximum daily infant exposure was 0.00263 mg/kg/day, which is 0.4% of the maternal weight adjusted dose. Exercise caution when administering SPRIX to a nursing woman. Available information has not shown any specific adverse events in nursing infants; however, instruct patients to contact their infant's health care provider if they note any adverse events.
Pediatric Use
- The safety and effectiveness of ketorolac in pediatric patients 17 years of age and younger have not been established.
Geriatic Use
- Exercise caution when treating the elderly (65 years and older) with SPRIX. Carefully consider the potential benefits and risks of SPRIX and other treatment options before deciding to use SPRIX. Use the lowest effective dose for the shortest duration consistent with individual patient treatment goals[see Dosage and Administration (2.4), Warnings and Precautions (5.2), Clinical Pharmacology (12.4)]. After observing the response to initial therapy with SPRIX, then adjust the dose and frequency to suit an individual patient's needs.
Gender
There is no FDA guidance on the use of Ketorolac tromethamine (nasal) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Ketorolac tromethamine (nasal) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Ketorolac tromethamine (nasal) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Ketorolac tromethamine (nasal) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Ketorolac tromethamine (nasal) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Ketorolac tromethamine (nasal) in patients who are immunocompromised.
Administration and Monitoring
Administration
- Nasal
Monitoring
There is limited information regarding Monitoring of Ketorolac tromethamine (nasal) in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Ketorolac tromethamine (nasal) in the drug label.
Overdosage
- There has been no experience with overdosage of SPRIX. In controlled overdosage studies with IM ketorolac injection, daily doses of 360 mg given for five days (approximately 3 times the maximum daily dose of SPRIX) caused abdominal pain and peptic ulcers, which healed after discontinuation of dosing. Single overdoses of ketorolac tromethamine have been variously associated with abdominal pain, nausea, vomiting, hyperventilation, peptic ulcers and/or erosive gastritis, and renal dysfunction.
- Symptoms and Signs
- Symptoms following acute NSAID overdose are usually limited to lethargy, drowsiness, nausea, vomiting, and epigastric pain, which are generally reversible with supportive care. Gastrointestinal bleeding can occur. Hypertension, acute renal failure, respiratory depression, and coma may occur, but are rare.
- Treatment
- Manage patients using symptomatic and supportive care following an NSAID overdose. There are no specific antidotes. Activated charcoal (60 g to 100 g in adults, 1 g/kg to 2 g/kg in children) may be indicated in patients seen within 4 hours of ingestion with symptoms or following a large oral overdose (5 to 10 times the usual dose). Forced diuresis, alkalization of urine, hemodialysis, or hemoperfusion may not be useful due to high protein binding.
Pharmacology
Mechanism of Action
- SPRIX contains ketorolac tromethamine, a nonsteroidal anti-inflammatory drug (NSAID). Ketorolac is an analgesic that inhibits the enzyme cyclooxygenase (COX), an early component of the arachidonic acid cascade, resulting in the reduced synthesis of prostaglandins, thromboxanes, and prostacyclin.
- Ketorolac does not bind to the opiate receptor subtypes (mu, kappa, delta), but a 30 mg dose of ketorolac tromethamine IM has demonstrated an overall analgesic effect between that obtained with morphine 6 mg and 12 mg. Ketorolac possesses no sedative or anxiolytic properties, and has no effect on gut motility.
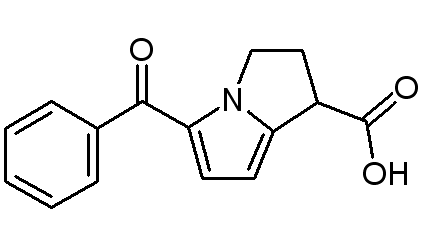
Structure
- Ketorolac tromethamine is a member of the pyrrolo-pyrrole group of nonsteroidal anti-inflammatory drugs (NSAIDs). The chemical name for ketorolac tromethamine is (±)-5-benzoyl-2,3-dihydro-1H-pyrrolizine-1-carboxylic acid, compound with 2-amino-2-(hydroxymethyl)-1,3-propanediol (1:1), and the structural formula is:
- The molecular weight of ketorolac tromethamine is 376.41. Ketorolac tromethamine is highly water-soluble, allowing its formulation in an aqueous nasal spray product at pH 7.2.
- SPRIX is a clear, colorless to yellow solution packaged in a glass vial with a snap on spray pump for use as an intranasal spray product. It contains the active ingredient (ketorolac tromethamine) and the excipients edetate disodium (EDTA), monobasic potassium phosphate, sodium hydroxide, and water for injection.
Pharmacodynamics
- Ketorolac tromethamine is a racemic mixture of [-]S and [+]R-enantiomeric forms, with the S-form having analgesic activity. Ketorolac, the active component of SPRIX, has anti-inflammatory, analgesic, and anti-pyretic effects. Studies directly comparing the analgesic effects of SPRIX and opioids have not been conducted.
Pharmacokinetics
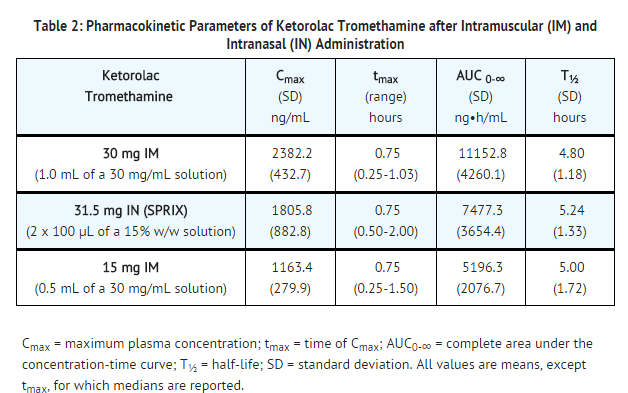
- The half-lives of ketorolac by the IN and IM routes were similar. The bioavailability of ketorolac by the IN route of administration of a 31.5 mg dose was approximately 60% compared to IM administration. (See Table 2.)
- Absorption: In a study in which SPRIX (31.5 mg) was administered to healthy volunteers four times daily for 5 days, the Cmax, tmax, and AUC values following the final dose were comparable to those obtained in the single-dose study. Accumulation of ketorolac has not been studied in special populations, geriatric, pediatric, renal failure or hepatic disease patients.
- Distribution: Scintigraphic assessment of drug disposition of ketorolac following SPRIX intranasal dosing demonstrated that most of the ketorolac was deposited in the nasal cavity and pharynx, with less than 20% deposited in the esophagus and stomach, and zero or negligible deposition in the lungs (<0.5%).
- The mean apparent volume (Vβ) of ketorolac tromethamine following complete distribution was approximately 13 liters. This parameter was determined from single-dose data. The ketorolac tromethamine racemate has been shown to be highly protein bound (99%). Nevertheless, plasma concentrations as high as 10 mcg/mL will only occupy approximately 5% of the albumin binding sites. Thus, the unbound fraction for each enantiomer will be constant over the therapeutic range. A decrease in serum albumin, however, will result in increased free drug concentrations. Ketorolac tromethamine is excreted in human milk.
- Metabolism: Ketorolac tromethamine is largely metabolized in the liver. The metabolic products are hydroxylated and conjugated forms of the parent drug. The products of metabolism, and some unchanged drug, are excreted in the urine.
- Excretion: The principal route of elimination of ketorolac and its metabolites is renal. About 92% of a given dose is found in the urine, approximately 40% as metabolites and 60% as unchanged ketorolac. Approximately 6% of a dose is excreted in the feces. A single-dose study with 10 mg ketorolac tromethamine (n=9) demonstrated that the S-enantiomer is cleared approximately two times faster than the R-enantiomer and that the clearance was independent of the route of administration. This means that the ratio of S/R plasma concentrations decreases with time after each dose. There is little or no inversion of the R- to S- form in humans.
- The half-life of the ketorolac tromethamine S-enantiomer was approximately 2.5 hours (SD ± 0.4) compared with 5 hours (SD ± 1.7) for the R-enantiomer. In other studies, the half-life for the racemate has been reported to lie within the range of 5 to 6 hours.
- Special Populations
- Drug Interactions: A study was conducted in subjects with symptomatic allergic rhinitis to assess the effects of the commonly used nasal spray products oxymetazoline hydrochloride and fluticasone propionate on the pharmacokinetics of SPRIX. Subjects received a single dose of oxymetazoline nasal spray followed by a single dose (31.5 mg) of SPRIX 30 min later. Subjects also received fluticasone nasal spray (200 mcg as 2 x 50 mcg in each nostril) for seven days, with a single dose (31.5 mg) of SPRIX on the 7th day. Administration of these common IN products had no effect of clinical significance on the rate or extent of ketorolac absorption. In addition, comparison of the pharmacokinetics of SPRIX in subjects with allergic rhinitis to data from a previous study in healthy subjects showed no differences that would be of clinical consequence for the efficacy or safety of SPRIX.
- Geriatric Patients: A single-dose study was conducted to compare the pharmacokinetics of SPRIX (31.5 mg) in subjects ≥ age 65 to the pharmacokinetics in subjects < age 65. Exposure to ketorolac was increased by 23% for the ≥ 65 population as compared to subjects < 65. Peak concentrations of 2028 and 1840 ng/mL were observed for the elderly and nonelderly adult populations, respectively, at 0.75 h after dosing. In the elderly population a longer terminal half-life was observed as compared to the nonelderly adults (4.5 h vs. 3.3 h, respectively).
- Renal Insufficiency: Based on single-dose data only, the mean half-life of ketorolac tromethamine in renally impaired patients is between 6 and 19 hours, and is dependent on the extent of the impairment. There is poor correlation between creatinine clearance and total ketorolac tromethamine clearance in the elderly and populations with renal impairment (r = 0.5).
- In patients with renal disease, the AUC∞ of each enantiomer increased by approximately 100% compared with healthy volunteers. The volume of distribution doubles for the S-enantiomer and increases by 1/5th for the R-enantiomer. The increase in volume of distribution of ketorolac tromethamine implies an increase in unbound fraction. The AUC∞-ratio of the ketorolac tromethamine enantiomers in healthy subjects and patients remained similar, indicating there was no selective excretion of either enantiomer in patients compared to healthy subjects.
- Hepatic Insufficiency: There was no significant difference in estimates of half-life, AUC∞ and Cmax in 7 patients with liver disease compared to healthy volunteers.
- Race: Pharmacokinetic differences due to race have not been identified.
Nonclinical Toxicology
- Carcinogenesis, Mutagenesis, and Impairment of Fertility
- Carcinogenesis: An 18-month study in mice with oral doses of ketorolac at 2 mg/kg/day (approximately 1.5 times the human systemic exposure at the recommended maximum IN dose of 31.5 mg qid, based on area-under-the-plasma-concentration curve [AUC]), and a 24-month study in rats at 5 mg/kg/day (approximately 0.8 times the human AUC) showed no evidence of tumorigenicity.
- Mutagenesis: Ketorolac was not mutagenic in the Ames test, unscheduled DNA synthesis and repair, or in forward mutation assays. Ketorolac did not cause chromosome breakage in the in vivo mouse micronucleus assay. At 1590 μg/mL and at higher concentrations, ketorolac increased the incidence of chromosomal aberrations in Chinese hamster ovarian cells.
- Impairment of fertility: Impairment of fertility did not occur in male or female rats at oral doses of 9 mg/kg (approximately 1.5 times the human AUC) and 16 mg/kg (approximately 2.7 times the human AUC) of ketorolac, respectively.
Clinical Studies
- Postoperative Pain
- The effect of SPRIX on acute pain was evaluated in two multi-center, randomized, double-blind, placebo-controlled studies.
- In a study of adults who had undergone elective abdominal or orthopedic surgery, 300 patients were randomized and treated with SPRIX or placebo administered every 8 hours and morphine administered via patient controlled analgesia on an as needed basis. Efficacy was demonstrated as a statistically significant greater reduction in the summed pain intensity difference over 48 hours in patients who received SPRIX as compared to those receiving placebo. The clinical relevance of this is reflected in the finding that patients treated with SPRIX required 36% less morphine over 48 hours than patients treated with placebo.
- In a study of adults who had undergone elective abdominal surgery, 321 patients were randomized and treated with SPRIX or placebo administered every 6 hours and morphine administered via patient controlled analgesia on an as needed basis. Efficacy was demonstrated as a statistically significant greater reduction in the summed pain intensity difference over 48 hours in patients who received SPRIX as compared to those receiving placebo. The clinical relevance of this is reflected in the finding that patients treated with SPRIX required 26% less morphine over 48 hours than patients treated with placebo.
How Supplied
- Preservative-free SPRIX Nasal Spray is supplied in boxes containing 5 single-day nasal spray bottles (NDC 0517-8880-05) or 1 single-day nasal spray bottle (NDC 0517-8880-01).
- Each single-day nasal spray bottle contains a sufficient quantity of solution to deliver 8 sprays for a total of 126 mg of ketorolac tromethamine. Each spray delivers 15.75 mg of ketorolac tromethamine. The delivery system is designed to administer precisely metered doses of 100 μL per spray.
Storage
- Protect from light and freezing. Store unopened SPRIX between 36°F and 46°F (2°C and 8°C). During use, keep containers of SPRIX Nasal Spray at controlled room temperature, between 59°F and 86°F (15°C and 30°C), out of direct sunlight. Bottles of SPRIX should be discarded within 24 hours of priming.
Images
Drug Images
{{#ask: Page Name::Ketorolac tromethamine (nasal) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Ketorolac tromethamine (nasal) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Instruct patients to read the NSAID Medication Guide that accompanies each prescription dispensed. Inform patients of the following information before initiating therapy with SPRIX.
- Instruct all patients to read and closely follow the FDA-approved SPRIX Patient Instructions to ensure proper administration of SPRIX. When prescribing SPRIX, inform patients or their caregivers of the potential risks of ketorolac treatment, instruct patients to seek medical advice if they develop treatment-related adverse events, advise patients not to give SPRIX to other family members, and advise patients to discard any unused drug.
- Limitations of Use
- Instruct patients not to use SPRIX for more than 5 days. Use of SPRIX alone or in combination with any other ketorolac product for more than 5 days increases the risk for serious complications including GI bleeding and renal injury.
- Gastrointestinal Effects
- Ketorolac is a potent NSAID and, like other NSAIDs, may cause serious side effects, such as gastrointestinal bleeding, which may result in hospitalization and even fatal outcome. Although serious GI tract ulcerations and bleeding can occur without warning symptoms, instruct patients to be alert for the signs and symptoms of ulcerations and bleeding, and to ask for medical advice when observing any indicative sign or symptom, including epigastric pain, dyspepsia, melena, and hematemesis. Instruct patients of the importance of this follow-up
- Renal Effects
- SPRIX is eliminated by the kidneys. Advise patients to maintain adequate fluid intake and request medical advice if urine output decreases significantly
- Cardiovascular Effects
- Ketorolac, like other NSAIDs, may cause serious CV events, such as MI or stroke, which may result in hospitalization and even death. Although serious CV events can occur without warning symptoms, advise patients to be alert for the signs and symptoms of chest pain, shortness of breath, weakness, slurring of speech, and that they should ask for medical advice when observing any indicative sign or symptoms. Inform patients of the importance of this follow-up
- Adverse Skin Reactions
- Ketorolac, like other NSAIDs, can cause serious skin side effects such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which may result in hospitalization and even death. Although serious skin reactions may occur without warning, instruct patients to be alert for the signs and symptoms of skin rash and blisters, fever, or other signs of hypersensitivity such as itching, and should ask for medical advice when observing any indicative signs or symptoms. Advise patients to stop the drug immediately if they develop any type of rash, and contact their physicians as soon as possible
- Weight Gain and Edema
- Instruct patients to promptly report signs or symptoms of unexplained weight gain or edema to their physicians .
- Hepatotoxicity
- Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). If these occur, instruct patients to stop therapy and seek immediate medical therapy
- Anaphylactoid Reactions
- Inform patients of the signs of an anaphylactoid reaction (e.g., difficulty breathing, swelling of the face or throat). If these occur, instruct patients to seek immediate emergency help
- Effects During Pregnancy
- Avoid the use of SPRIX at or beyond 30 weeks gestation as ketorolac can cause premature closure of the ductus arteriosus .
- Single Day Container
- Instruct patients not to use any single bottle of SPRIX for more than one day
- Nasal Discomfort
- Advise patients that they may experience transient, mild to moderate nasal irritation or discomfort upon dosing.
Precautions with Alcohol
- Alcohol-Ketorolac tromethamine (nasal) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Ketorolac tromethamine (nasal) Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Ketorolac tromethamine (nasal) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Ketorolac tromethamine (nasal) |Label Name=Ketorolac tromethamine (nasal)06.png
}}
{{#subobject:
|Label Page=Ketorolac tromethamine (nasal) |Label Name=Ketorolac tromethamine (nasal)07.png
}}