Tension pneumothorax resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohamed Moubarak, M.D. [2]
Synonyms and keywords: Collapsed lung; air around the lung; air outside the lung
| Tension Pneumothorax Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| Diagnosis |
| Treatment |
| Do's |
| Don'ts |
Overview
Tension pneumothorax is a medical emergency caused by accumulation of air in the pleural cavity. Air enter the intrapleural space through the lung parenchyma, or through a traumatic communication from the chest wall. It tends to occur in clinical situations such as ventilation, resuscitation, trauma, or in patients with lung disease.[1] The aim of tension pneumothorax management is to relieve the pressure from thorax.
Causes
Life Threatening Causes
Tension pneumothorax is a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
Tension pneumothorax can be a complication of primary, or secondary pneumothorax. The most common causes of tension pneumothorax are:
- Mechanical ventilation
- Trauma
- Central venous catheter
- Cardiopulmonary resuscitation
- Emphysema
- Chronic obstructive pulmonary disease
- Asthma
Diagnosis
Shown below is an algorithm depicting the diagnostic approach of tension pneumothorax based on the British Thoracic Society Pleural Disease Guideline 2010.[1]
Characterize the symptoms:[1] Tension pneumothorax requires immediate intervention,and diagnosis should be made based on the history and physical examination findings ❑ Breathlessness | |||||||||||||||||||||||||||
Consider risk factors: ❑ Recent invasive procedures ❑ Cigarette smoking
| |||||||||||||||||||||||||||
Examine the patient: Vital signs ❑ Pulse:
Focused chest examination:[1] Inspection ❑ Reduced lung expansion on the affected side Palpation ❑ Trachea shifted to the opposite side Percussion Auscultation ❑ Diminished breath sounds on the affected side | |||||||||||||||||||||||||||
Consider alternative diagnoses:
❑ Asthma
| |||||||||||||||||||||||||||
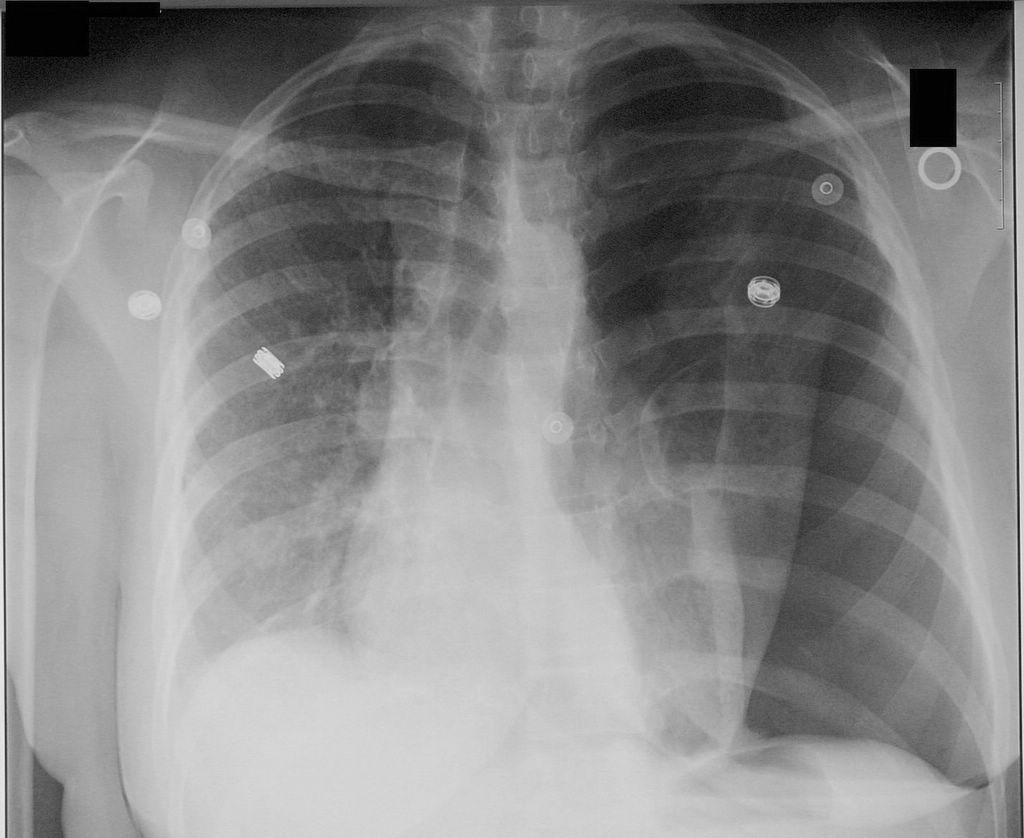
Imaging studies: Immediately proceed to needle decompression in clinically diagnosed hemodynamically unstable patients
Picture courtesy of Wikidoc.org
❑ Chest CT scanning
Picture courtesy of Wikidoc.org | |||||||||||||||||||||||||||
Treatment
Manage the patient with a multidisciplinary team: ❑ Consult a thoracic surgeon ❑ Consult a cardiologist | |||||||||||||||||||||||||||||||||||||
Emergency needle decompression
❑ Aseptic preparation
❑ Use 14-16 G intravenous cannula
❑ Listen for gush of air ❑ Watch how to do a needle decompression {{#ev:youtube|UvHJ4pjNh2Q|400|How to do a needle decompression}} Video adapted from Youtube.com Antibiotic therapy | |||||||||||||||||||||||||||||||||||||
| Admit the patient ❑ Refer the patient to respiratory specialist within 24h of admission | |||||||||||||||||||||||||||||||||||||
Insert chest drain ❑ Timing of procedures:
❑ Image guidance
❑ Ensure aseptic technique
❑ Requirments
❑ Equipment required
Avoid complications:
❑ Intrapleural infection
❑ Wound infection
❑ Drain dislodgement and blockage
❑ Visceral injury
| |||||||||||||||||||||||||||||||||||||
Discharge and follow up ❑ All patients should be followed up by respiratory physicians | |||||||||||||||||||||||||||||||||||||
Do`s
- Tension pneumothorax diagnosis should be made based on the history and physical examination findings.
- Serial chest radiographs every 6 hrs on the first day after injury to rule out pneumothorax is ideal.[4]
- Leave the cannula in place until bubbling is confirmed in the chest drain underwater seal system
- Suspect tension pneumothorax with blunt and penetrating trauma to the chest
- Differentiate tension pneumothorax from pericardial tamponade, and myocardial infarction.
- Suspect tension pneumothorax in patients on mechanical ventilations, who have a rapid onset of hemodynamic instability or cardiac arrest, and require increasing peak inspiratory pressures.
- Check chest tubes, as they can become plugged or malpositioned and stop functioning.
- Give adequate analgesia to patients before chest tube insertion, as the procedure is extremely painful.
- Refer the patient to respiratory specialist within 24h of admission.
Dont`s
- Don`t start using chest radiograph or CT scan unless in doubt regarding the diagnosis and when the patient's clinical condition is sufficiently stable.
- Don`t use large bore chest drains.[1]
- Don`t repeat needle aspiration unless there were technical difficulties.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group (2010). "Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010". Thorax. 65 Suppl 2: ii18–31. doi:10.1136/thx.2010.136986. PMID 20696690.
- ↑ Abolnik IZ, Lossos IS, Gillis D, Breuer R (1993). "Primary spontaneous pneumothorax in men". Am J Med Sci. 305 (5): 297–303. PMID 8484388.
- ↑ Flume PA, Strange C, Ye X, Ebeling M, Hulsey T, Clark LL (2005). "Pneumothorax in cystic fibrosis". Chest. 128 (2): 720–8. doi:10.1378/chest.128.2.720. PMID 16100160.
- ↑ 4.0 4.1 4.2 Sharma A, Jindal P (2008). "Principles of diagnosis and management of traumatic pneumothorax". J Emerg Trauma Shock. 1 (1): 34–41. doi:10.4103/0974-2700.41789. PMC 2700561. PMID 19561940.