Tension pneumothorax resident survival guide: Difference between revisions
No edit summary |
Hamid Qazi (talk | contribs) No edit summary |
||
| (140 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div style="width: 80%;"> | <div style="width: 80%;"> | ||
__NOTOC__ | __NOTOC__ | ||
{{CMG}}; {{AE}} {{MM}} | {{CMG}}; {{AE}} {{HQ}}, {{MM}}, {{TS}}, {{Rim}} | ||
{{ | |||
{| class="infobox" style="margin: 0 0 0 0; border: 0; float: right; width: 100px; background: #A8A8A8; position: fixed; top: 250px; right: 21px; border-radius: 0 0 10px 10px;" cellpadding="0" cellspacing="0"; | {| class="infobox" style="margin: 0 0 0 0; border: 0; float: right; width: 100px; background: #A8A8A8; position: fixed; top: 250px; right: 21px; border-radius: 0 0 10px 10px;" cellpadding="0" cellspacing="0"; | ||
| Line 13: | Line 11: | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Tension pneumothorax resident survival guide#Causes|Causes]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Tension pneumothorax resident survival guide#Causes|Causes]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Tension pneumothorax resident survival guide# | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left |[[Tension pneumothorax resident survival guide#FIRE: Focused Initial Rapid Evaluation|FIRE]] | ||
|- | |||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left |[[Tension pneumothorax resident survival guide#Complete Diagnostic Approach|Diagnosis]] | |||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Tension pneumothorax resident survival guide#Treatment|Treatment]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Tension pneumothorax resident survival guide#Treatment|Treatment]] | ||
| Line 22: | Line 22: | ||
|} | |} | ||
=Overview= | |||
Tension pneumothorax is a | Tension pneumothorax is a life threatening condition that results from the accumulation of air in the [[pleural cavity]]. Air enters the [[intrapleural space]] through an injured [[parietal pleura]], [[visceral pleura]] or [[tracheobronchial tree]] that forms a one way valve. The one way valve allows the air to enter in the pleural cavity (during inspiration) but prevents its escape (during expiration). Subsequently, the intrapleural pressure rises and results in respiratory and cardiovascular failure. [[Tension pneumothorax]] can occur as a result of [[trauma]], [[ventilation]] or [[resuscitation]].<ref name="pmid20696690">{{cite journal| author=MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group| title=Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. | journal=Thorax | year= 2010 | volume= 65 Suppl 2 | issue= | pages= ii18-31 | pmid=20696690 | doi=10.1136/thx.2010.136986 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20696690 }} </ref> The cardinal symptoms and signs of [[tension pneumothorax]] are severe [[dyspnea]], [[chest pain]], [[hypotension]], [[hypoxia]], [[tachycardia]] and [[jugular vein distention]]. [[Tension pneumothorax]] should be managed immediately with emergency needle decompression followed by insertion of a [[chest tube]]. | ||
==Causes== | ==Causes== | ||
| Line 31: | Line 31: | ||
===Common Causes=== | ===Common Causes=== | ||
* [[Asthma]] | |||
* [[ | |||
* [[Central venous catheter]] | * [[Central venous catheter]] | ||
* [[Cardiopulmonary resuscitation]] | * [[Cardiopulmonary resuscitation]] | ||
* [[Chronic obstructive pulmonary disease]] | |||
* [[Emphysema]] | * [[Emphysema]] | ||
* [[ | * [[Mechanical ventilation]] | ||
* [[ | * [[Trauma]]<ref name="pmid20696690">{{cite journal| author=MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group| title=Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. | journal=Thorax | year= 2010 | volume= 65 Suppl 2 | issue= | pages= ii18-31 | pmid=20696690 | doi=10.1136/thx.2010.136986 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20696690 }} </ref> | ||
Click '''[[Pneumothorax causes|here]]''' for the complete list of causes. | |||
==FIRE: Focused Initial Rapid Evaluation== | |||
A Focused Initial Rapid Evaluation (FIRE) as shown below should be performed to identify patients in need of immediate intervention. | |||
<span style="font-size:85%">Boxes in red signify that an urgent management is needed.</span> | |||
{{Family tree/start}} | |||
{{familytree | | | A01 | | | A01=<div style="text-align: left; width: 22em"> '''Identify cardinal findings that increase the pretest probability of tension pneumothorax:'''</div> <div style="text-align: left; width: 22em"> ❑ [[Chest pain]] <br>❑ [[Dyspnea]]<br>❑ [[Hypoxia]] <br>❑ [[Hypotension]]<br>❑ [[Tachycardia]] <br> ❑ [[Jugular venous distension]]<br> | |||
❑ Absent [[breath sounds]] on the affected side <br> | |||
❑ [[Percussion#Hypperresonance|Hyperresonance]] on the affected side <br> | |||
❑ Hyperexpansion of the the affected side <br> | |||
❑ [[Tracheal deviation]] towards the unaffected side<ref name="pmid20696690">{{cite journal| author=MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group| title=Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. | journal=Thorax | year= 2010 | volume= 65 Suppl 2 | issue= | pages= ii18-31 | pmid=20696690 | doi=10.1136/thx.2010.136986 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20696690 }} </ref></div>}} | |||
{{familytree | | | |!| | | }} | |||
{{familytree | | | A02 | | A02= <div style="text-align: left; width: 22em">Does the patient have high probability of tension pneumothorax?</div>}} | |||
{{familytree | |,|-|^|-|.| | | | |}} | |||
{{familytree | B01 | | B02 | | | | B01=<div style=" width: 22em"> <div style="background: #FA8072"> {{fontcolor|#F8F8FF|'''Yes'''}} </div> </div>| B02=<div style=" width: 25em">'''No'''</div>}} | |||
{{familytree | |!| | | |!| | | | | | | }} | |||
{{familytree | B03 | | B04 | | | | | |B03=<div style="float: left; text-align: left; width: 20em; background: #FA8072; padding:1em;"> {{fontcolor|#F8F8FF| '''❑ Immediately [[Tension pneumothorax resident survival guide#Treatment|<span style="color:white;">insert a 14-16 Gauge needle </span>]] in the 2nd [[intercostal space|<span style="color:white;">intercostal space</span>]] at the [[midclavicular line|<span style="color:white;">midclavicular line</span>]] of the affected hemithorax'''}} </div> |B04=<div style="float: left; text-align: left; width: 22em; padding:1em;">❑ '''[[Tension pneumothorax resident survival guide#Complete Diagnostic Approach of tension pneumothorax|Continue with the complete diagnostic approach below]]''' </div>}} | |||
{{familytree | |!| | | | | | | | | | | | | }} | |||
{{familytree | B06 | | | | | | | | | | | |B06=<div style=" width: 22em"> <div style="background: #FA8072"> {{fontcolor|#F8F8FF|'''❑ Insert chest drain immediately after needle decompression'''}} </div> </div>}} | |||
{{Family tree/end}} | |||
<br> | |||
== | ==Complete Diagnostic Approach== | ||
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.<ref name="pmid20696690">{{cite journal| author=MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group| title=Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. | journal=Thorax | year= 2010 | volume= 65 Suppl 2 | issue= | pages= ii18-31 | pmid=20696690 | doi=10.1136/thx.2010.136986 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20696690 }} </ref><br> | |||
{{familytree/start |summary=Diagnostic approach}} | {{familytree/start |summary=Diagnostic approach}} | ||
{{familytree | | | |A01 | | | | |A01= <div style="float: Left; text-align: left; width: 40em; padding:1em;">'''Characterize the symptoms:'''<br> | {{familytree | | | |A01 | | | | |A01= <div style="float: Left; text-align: left; width: 40em; padding:1em;">'''Characterize the symptoms:'''<br> | ||
| Line 54: | Line 75: | ||
❑ [[Anxiety]]<BR> | ❑ [[Anxiety]]<BR> | ||
❑ [[Fatigue]]<BR> | ❑ [[Fatigue]]<BR> | ||
❑ | ❑ [[Altered mental status]] (in late stages)<br> | ||
</div>}} | </div>}} | ||
{{familytree | | | | |!| | | | | | | | | }} | {{familytree | | | | |!| | | | | | | | | }} | ||
| Line 60: | Line 81: | ||
❑ Recent invasive procedures<br> | ❑ Recent invasive procedures<br> | ||
:❑ [[Thoracentesis]]<br> | :❑ [[Thoracentesis]]<br> | ||
:❑ [[Central venous catheter]] | :❑ [[Central venous catheter]] <br> | ||
:❑ [[Bronchoscopy]]<br> | :❑ [[Bronchoscopy]]<br> | ||
:❑ [[Biopsy|Pleural biopsy]]<br> | :❑ [[Biopsy|Pleural biopsy]]<br> | ||
| Line 66: | Line 87: | ||
❑ [[Cardiopulmonary resuscitation]]<br> | ❑ [[Cardiopulmonary resuscitation]]<br> | ||
❑ Presence of [[Drain (surgery)|chest drains]]<br> | ❑ Presence of [[Drain (surgery)|chest drains]]<br> | ||
❑ [[Hyperbaric oxygen]] | ❑ [[Hyperbaric oxygen|Hyperbaric oxygen treatment]]<br> | ||
❑ [[Trauma|Chest wall trauma]] </div>}} | ❑ [[Trauma|Chest wall trauma]] </div>}} | ||
| Line 72: | Line 93: | ||
{{familytree | | | | B01 | | | | |B01= <div style="float: Left; text-align: left; width: 30em; padding:1em;">'''Examine the patient:'''<BR> | {{familytree | | | | B01 | | | | |B01= <div style="float: Left; text-align: left; width: 30em; padding:1em;">'''Examine the patient:'''<BR> | ||
'''Appearance of the patient'''<br> | '''Appearance of the patient'''<br> | ||
❑ | ❑ [[Distress|Severe distress]] and [[labored respiration]] | ||
'''Vital signs'''<BR> | '''Vital signs'''<BR> | ||
❑ [[Tachycardia]]<BR> | |||
❑ [[Hypotension]] <BR> | |||
❑ [[Tachypnea]]<BR> | |||
❑ [[Pulsus paradoxus]] | |||
❑ [[ | |||
'''Skin'''<br> | '''Skin'''<br> | ||
| Line 96: | Line 110: | ||
❑ [[Jugular venous distension]] (absent in severe [[hypotension]])<BR> | ❑ [[Jugular venous distension]] (absent in severe [[hypotension]])<BR> | ||
'''Respiratory examination | '''Respiratory examination'''<BR> | ||
'''Inspection'''<BR> | '''''Inspection'''''<BR> | ||
❑ | ❑ Enlargement of the involved side of the chest <BR> | ||
❑ [[Intercostal space]] widening on the affected | ❑ [[Intercostal space]] widening on the affected side<br> | ||
'''Palpation'''<BR> | '''''Palpation'''''<BR> | ||
❑ Reduced | ❑ Reduced lung expansion on the affected side <BR> | ||
❑ [[ | ❑ [[Tracheal deviation]] to the contralateral side<BR> | ||
❑ Decreased [[vocal fremitus]] over the affected | ❑ Decreased [[vocal fremitus]] over the affected side<BR> | ||
❑ Displacement of the [[apex beat]]<BR> | ❑ Displacement of the [[apex beat]]<BR> | ||
'''Percussion'''<BR> | '''''Percussion'''''<BR> | ||
❑ [[Percussion|Hyperresonance]] over the affected | ❑ [[Percussion|Hyperresonance]] over the affected side<BR> | ||
'''Auscultation'''<BR> | '''''Auscultation'''''<BR> | ||
❑ Diminished [[breath sounds]] on the affected side<BR> | ❑ Diminished [[breath sounds]] on the affected side<BR> | ||
'''Additional findings in ventilated patients | '''Additional findings in ventilated patients'''<br> | ||
❑ Decreased [[oxygen saturation]]<br> | ❑ Decreased [[oxygen saturation]]<br> | ||
❑ Increase in inflation pressure <br> | ❑ Increase in inflation pressure <br> | ||
❑ Increase in [[peak airway pressure]]<br> | ❑ Increase in [[Mechanical ventilation initial ventilator settings|peak airway pressure]]<br> | ||
❑ Airway pressure alarm <br></div>}} | ❑ Airway pressure alarm in [[mechanical ventilation|mechanically ventilated]] patients<br></div>}} | ||
{{familytree | | | | |!| | | | | | | | | }} | {{familytree | | | | |!| | | | | | | | | }} | ||
{{familytree | | | | E01 | | | | | E01=<div style="float: Left; text-align: left; width: 40em; padding:1em;"> ''' | {{familytree | | | | E01 | | | | | E01=<div style="float: Left; text-align: left; width: 40em; padding:1em;"> '''Consider alternative diagnosis:'''<br> | ||
❑ [[Acute myocardial infarction]] <br> | ❑ [[Acute myocardial infarction]] <br> | ||
:❑ Substernal chest discomfort or chest | :❑ Substernal [[chest discomfort]], [[chest pain|pain]] or tightness | ||
❑ [[Pericardial tamponade]] <br> | :❑ Radiation of [[chest pain]] to the left arm or jaw | ||
:❑ | ❑ [[Cardiac tamponade resident survival guide|Pericardial tamponade]] <br> | ||
:❑ [[Hypotension]] | |||
:❑ [[Tachycardia]] | |||
:❑ [[Muffled heart sounds]] | |||
:❑ [[Jugular vein distention]] | |||
:❑ [[Pulsus paradoxus]] | :❑ [[Pulsus paradoxus]] | ||
❑ [[Pulmonary embolism]]<br> | ❑ [[Pulmonary embolism]]<br> | ||
:❑ Presence of [[Pulmonary embolism risk factors|risk factors for pulmonary embolism]]<br> | :❑ Presence of [[Pulmonary embolism risk factors|risk factors for pulmonary embolism]]<br> | ||
:❑ | :❑ Localized warmth, [[tenderness]], [[edema]] and [[erythema]] in the leg suggestive of [[DVT|deep vein thrombosis]]</div>}} | ||
{{familytree | | | | | | {{familytree | | |,|-|^|-|.| | }} | ||
{{familytree | {{familytree | | J01 | | J02 | |J01=❑ '''High probability of tension pneumothorax''' |J02= ❑ '''Low probability of tension pneumothorax and patient is hemodynamically stable''' }} | ||
❑ Proceed with | {{familytree | | |!| | | |!| | | | | }} | ||
''' | {{familytree |boxstyle=background: #FA8072; color: #F8F8FF;| | M01 | | |!| | M01=❑ Proceed with '''immediate''' [[Tension pneumothorax resident survival guide#Treatment|<span style="color:white;">needle decompression </span>]]}} | ||
<span style="color: | {{familytree | | | | | | M02 | M02= <div style="float: Left; text-align: left; width: 40em; padding:1em;"> '''Order imaging studies:'''<BR> | ||
❑ Order [[chest X-ray]] looking for:<BR> | |||
:❑ Air in the [[pleural cavity]]<BR> | :❑ Air in the [[pleural cavity]]<BR> | ||
:❑ Contralateral deviation of | :❑ Contralateral [[deviation of trachea]]<BR> | ||
:❑ Increased thoracic volume<BR> | :❑ Increased thoracic volume<BR> | ||
:❑ Ipsilateral flattening of heart border<BR> | :❑ Ipsilateral flattening of heart border<BR> | ||
:❑ Mid diaphragmatic depression<BR> | :❑ Mid diaphragmatic depression<BR> | ||
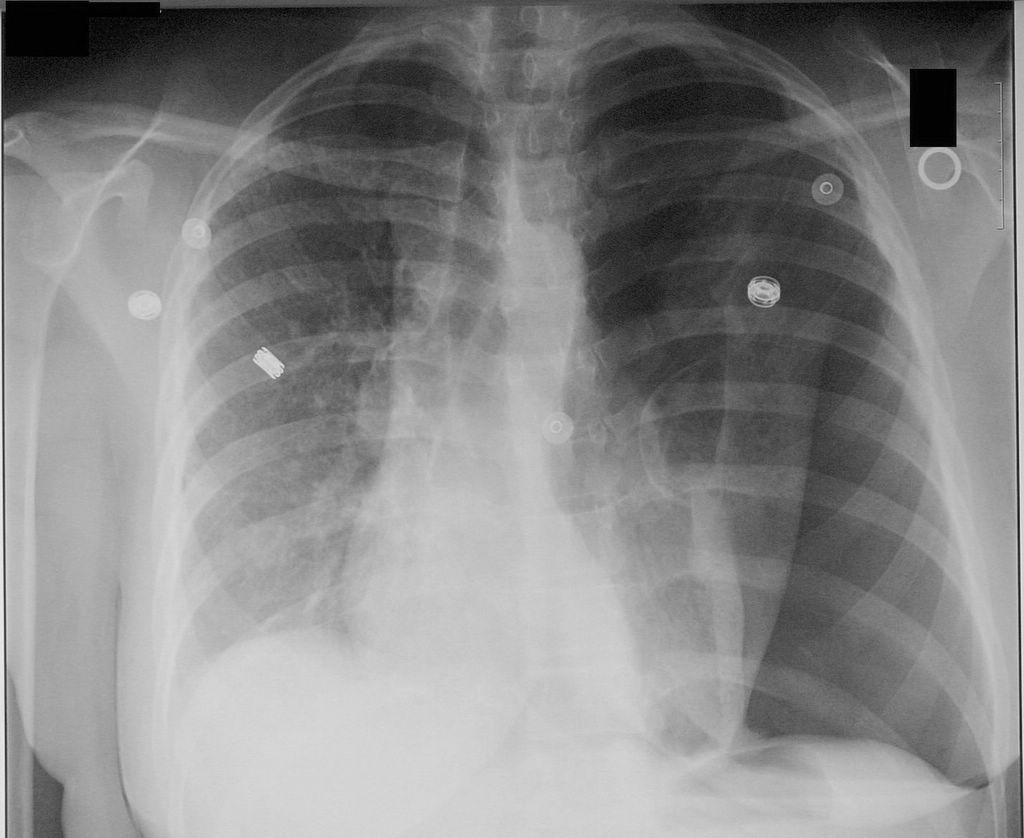
❑ | <SMALL>Shown below is an image of a chest X-ray depicting tension pneumothorax in the left lung.</SMALL><br> | ||
[[File:Pneumothorax CXR.jpg|250px]]<BR> | |||
❑ Perform serial chest X-ray every 6 hours to rule out [[pneumothorax]] in cases of [[trauma]]<ref name="pmid19561940">{{cite journal| author=Sharma A, Jindal P| title=Principles of diagnosis and management of traumatic pneumothorax. | journal=J Emerg Trauma Shock | year= 2008 | volume= 1 | issue= 1 | pages= 34-41 | pmid=19561940 | doi=10.4103/0974-2700.41789 | pmc=PMC2700561 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19561940 }} </ref><BR> | |||
❑ Order chest [[CT scan]] for uncertain or complex cases <br> | |||
<SMALL>Shown below is an image of CT scan depicting left-sided pneumothorax. A chest tube is in place, the lumen (black) can be seen adjacent to the pleural cavity (black) and ribs (white).</SMALL><br> | |||
[[File:Pneumothorax CT.jpg|250px]]<BR> | [[File:Pneumothorax CT.jpg|250px]]<BR> | ||
<BR> | |||
❑ Order [[ultrasonography]] in supine trauma patients among whom a [[chest X-ray]] can not be performed <BR></div> }} | |||
❑ [[ | |||
{{familytree/end}} | {{familytree/end}} | ||
==Treatment== | ==Treatment== | ||
{{familytree/start}} | |||
{{familytree | | | | E01 | | | | | | | | | | | | | | E01= <div style="float: Left; text-align: left; width: 40em; padding:1em;">'''Perform emergency needle decompression:'''<ref name="pmid20696690">{{cite journal| author=MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group| title=Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. | journal=Thorax | year= 2010 | volume= 65 Suppl 2 | issue= | pages= ii18-31 | pmid=20696690 | doi=10.1136/thx.2010.136986 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20696690 }} </ref><br> | |||
❑ Wear a gown, face mask and eye shield <br> | |||
❑ Ensure aseptic preparation<BR> | |||
❑ Determine the site of insertion of the [[needle]] | |||
:❑ '''2nd [[intercostal space]] at the [[midclavicular line]]''' of affected hemithorax, OR <BR> | |||
:❑ 4th or 5th [[intercostal space]] on mid or anterior axillary line, if the initial decompression failed because of a thick [[chest wall]]<ref name="pmid20696690">{{cite journal| author=MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group| title=Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. | journal=Thorax | year= 2010 | volume= 65 Suppl 2 | issue= | pages= ii18-31 | pmid=20696690 | doi=10.1136/thx.2010.136986 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20696690 }} </ref> | |||
❑ | ❑ Insert a 14-16 gauge [[needle]] with a [[catheter]] at a 90° angle<BR> | ||
❑ Remove the [[needle]] and leave the [[catheter]] in place<br> | |||
❑ Secure the [[catheter]] in place while preparing for [[tube thoracostomy]] (chest drain) <br> | |||
❑ | ❑ Confirm the diagnosis by observing instantaneous escape of air as the needle is inserted<br> | ||
❑ Check for any improvement of the patient's status<br> | |||
<span style="color:red">Don't remove the catheter, until a chest drain is inserted and is functioning properly.</span><br> | |||
<br> | |||
:❑ 2nd [[intercostal space]] | ''Shown below is a video depicting the steps for needle decompression'' <br> | ||
:❑ 4th or 5th [[intercostal space]] on mid or anterior axillary line, if initial decompression | {{#ev:youtube|UvHJ4pjNh2Q|400|How to do a needle decompression}} | ||
❑ | |||
< | |||
<span style=" | |||
<SMALL>''Video adapted from Youtube.com''</SMALL> | <SMALL>''Video adapted from Youtube.com''</SMALL> | ||
</div>}} | </div>}} | ||
{{familytree | | | | |!| | | | | | | }} | {{familytree | | | | |!| | | | | | | }} | ||
{{familytree | | | | H02 | | | | | | | | | |H02= <div style="float: Left; text-align: left; width: 40em; padding:1em;"> ''' Insert chest | {{familytree | | | | H02 | | | | | | | | | |H02= <div style="float: Left; text-align: left; width: 40em; padding:1em;"> ''' Insert a chest tube (tube thoracostomy) immediately after needle decompression:'''<BR> | ||
❑ Make sure that the following equipments are available: | |||
:❑ 1% [[lidocaine]] | |||
: | |||
❑ Make sure that following equipments are available: | |||
:❑ 1% [[ | |||
:❑ [[Iodine]] or [[chlorhexidine]] solution in [[alcohol]] | :❑ [[Iodine]] or [[chlorhexidine]] solution in [[alcohol]] | ||
:❑ Sterile drapes, gown, gloves | :❑ Sterile drapes, gown, gloves | ||
:❑ Needles, syringes, gauze | :❑ [[Needles]], [[syringes]], gauze [[swab]]s | ||
:❑ Scalpel, suture (0 or 1-0 silk) | :❑ [[Scalpel]], [[suture]] (0 or 1-0 silk) | ||
:❑ [[Chest tube]] kit | :❑ [[Chest tube]] kit | ||
:❑ Closed system drain (including water) and tubing | :❑ Closed system drain (including water) and tubing | ||
:❑ Dressing | :❑ [[Dressing (medical)|Dressing]] | ||
:❑ Clamp | :❑ Clamp | ||
❑ | ❑ Administer adequate analgesics <BR> | ||
❑ Determine the insertion site at the '''anterior axillary line over the 4th or 5th rib''' <br> | |||
❑ Insert the chest drain <br> | |||
❑ Remove the catheter inserted during needle decompression after the confirmation that the chest drain is functioning properly <BR> | |||
❑ Check chest tubes frequently, as they can become plugged or malpositioned <BR> | |||
❑ Remove the chest tube after re-expansion of the affected lung is confirmed by a [[chest X-ray]]<br></div>}} | |||
❑ | |||
❑ Remove the | |||
❑ Check chest tubes frequently, as they can become plugged or malpositioned <BR></div>}} | |||
{{familytree | | | | |!| | | | | | }} | {{familytree | | | | |!| | | | | | }} | ||
{{familytree | | | | I01 | | | | | | | | | | | | | | I01=<div style="float: Left; text-align: left; width: 40em; padding:1em;"> ''' | {{familytree | | | | I01 | | | | | | | | | | | | | | I01=<div style="float: Left; text-align: left; width: 40em; padding:1em;"> '''Follow up:'''<BR> | ||
❑ | ❑ Refer the patient to a respiratory physician if pneumothorax does not respond within 48 hours<BR> | ||
❑ Advise to return to hospital if increasing breathlessness develops<BR> | ❑ Advise to return to the hospital if increasing breathlessness develops<BR> | ||
❑ Advise to avoid air travel<BR> | ❑ Advise to avoid air travel until the full resolution of the pneumothorax is confirmed by a chest X-ray<BR> | ||
❑ Advise to avoid diving <BR> | ❑ Advise to avoid diving permanently unless the patient is treated with [[Pneumothorax surgery|surgical pleurectomy]]<BR> | ||
</div>}} | </div>}} | ||
{{familytree/end}} | {{familytree/end}} | ||
==Do's== | ==Do's== | ||
*[[ | * Suspect [[tension pneumothorax]] in the case of blunt and penetrating trauma to the chest. | ||
* | * Immediately cover penetrating chest wounds with an occlusive or pressure bandage in trauma patients with suspected [[tension pneumothorax]]. | ||
* | * Suspect [[tension pneumothorax]] among patients on mechanical ventilation who develop a rapid onset of hemodynamic instability or [[cardiac arrest]] and require an increase in the peak inspiratory pressure. | ||
* Order serial chest radiographs every 6 hours on the first day following chest [[trauma]] to rule out [[pneumothorax]].<ref name="pmid19561940">{{cite journal| author=Sharma A, Jindal P| title=Principles of diagnosis and management of traumatic pneumothorax. | journal=J Emerg Trauma Shock | year= 2008 | volume= 1 | issue= 1 | pages= 34-41 | pmid=19561940 | doi=10.4103/0974-2700.41789 | pmc=PMC2700561 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19561940 }} </ref> | |||
* Refer the patient to a respiratory specialist within 24 hours of admission. | |||
* | * Order a [[chest X-ray]] before chest tube removal to confirm the re-expansion of the affected lung. | ||
==Don'ts== | ==Don'ts== | ||
*Don | *Don't remove the catheter from the 2nd [[intercostal space]] unless a chest tube is appropriately placed. | ||
*Don | *Don't use large bore chest tubes.<ref name="pmid20696690">{{cite journal| author=MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group| title=Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. | journal=Thorax | year= 2010 | volume= 65 Suppl 2 | issue= | pages= ii18-31 | pmid=20696690 | doi=10.1136/thx.2010.136986 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20696690 }}</ref> | ||
*Don | *Don't leave the chest tube more than 7 days, as it will increase the risk of infection. | ||
==References== | ==References== | ||
| Line 240: | Line 233: | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Medicine]] | [[Category:Medicine]] | ||
[[Category:Resident survival guide]] | [[Category:Resident survival guide]] | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
</div> | </div> | ||
<headertabs /> | |||
Latest revision as of 20:02, 18 February 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Hamid Qazi, MD, BSc [2], Mohamed Moubarak, M.D. [3], Twinkle Singh, M.B.B.S. [4], Rim Halaby, M.D. [5]
| Tension Pneumothorax Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| FIRE |
| Diagnosis |
| Treatment |
| Do's |
| Don'ts |
Overview
Tension pneumothorax is a life threatening condition that results from the accumulation of air in the pleural cavity. Air enters the intrapleural space through an injured parietal pleura, visceral pleura or tracheobronchial tree that forms a one way valve. The one way valve allows the air to enter in the pleural cavity (during inspiration) but prevents its escape (during expiration). Subsequently, the intrapleural pressure rises and results in respiratory and cardiovascular failure. Tension pneumothorax can occur as a result of trauma, ventilation or resuscitation.[1] The cardinal symptoms and signs of tension pneumothorax are severe dyspnea, chest pain, hypotension, hypoxia, tachycardia and jugular vein distention. Tension pneumothorax should be managed immediately with emergency needle decompression followed by insertion of a chest tube.
Causes
Life Threatening Causes
Tension pneumothorax is a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
- Asthma
- Central venous catheter
- Cardiopulmonary resuscitation
- Chronic obstructive pulmonary disease
- Emphysema
- Mechanical ventilation
- Trauma[1]
Click here for the complete list of causes.
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) as shown below should be performed to identify patients in need of immediate intervention.
Boxes in red signify that an urgent management is needed.
Identify cardinal findings that increase the pretest probability of tension pneumothorax: ❑ Chest pain ❑ Dyspnea ❑ Hypoxia ❑ Hypotension ❑ Tachycardia ❑ Jugular venous distension ❑ Absent breath sounds on the affected side | |||||||||||||||||||||||||||||
Does the patient have high probability of tension pneumothorax? | |||||||||||||||||||||||||||||
Yes | No | ||||||||||||||||||||||||||||
❑ Immediately insert a 14-16 Gauge needle in the 2nd intercostal space at the midclavicular line of the affected hemithorax | |||||||||||||||||||||||||||||
❑ Insert chest drain immediately after needle decompression | |||||||||||||||||||||||||||||
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[1]
Characterize the symptoms: ❑ Dyspnea | |||||||||||||||||||||||||||
Identify the precipitating factors: ❑ Recent invasive procedures ❑ Mechanical ventilation | |||||||||||||||||||||||||||
Examine the patient: Appearance of the patient Vital signs ❑ Tachycardia Skin ❑ Cyanosis Neck ❑ Jugular venous distension (absent in severe hypotension) Respiratory examination Inspection Additional findings in ventilated patients ❑ Decreased oxygen saturation | |||||||||||||||||||||||||||
Consider alternative diagnosis:
| |||||||||||||||||||||||||||
| ❑ High probability of tension pneumothorax | ❑ Low probability of tension pneumothorax and patient is hemodynamically stable | ||||||||||||||||||||||||||
| ❑ Proceed with immediate needle decompression | |||||||||||||||||||||||||||
Order imaging studies: ❑ Order chest X-ray looking for:
Shown below is an image of a chest X-ray depicting tension pneumothorax in the left lung. | |||||||||||||||||||||||||||
Treatment
Perform emergency needle decompression:[1] ❑ Wear a gown, face mask and eye shield
❑ Insert a 14-16 gauge needle with a catheter at a 90° angle | |||||||||||||||||||||||||||||||||||||
Insert a chest tube (tube thoracostomy) immediately after needle decompression: ❑ Make sure that the following equipments are available:
❑ Administer adequate analgesics | |||||||||||||||||||||||||||||||||||||
Follow up: ❑ Refer the patient to a respiratory physician if pneumothorax does not respond within 48 hours | |||||||||||||||||||||||||||||||||||||
Do's
- Suspect tension pneumothorax in the case of blunt and penetrating trauma to the chest.
- Immediately cover penetrating chest wounds with an occlusive or pressure bandage in trauma patients with suspected tension pneumothorax.
- Suspect tension pneumothorax among patients on mechanical ventilation who develop a rapid onset of hemodynamic instability or cardiac arrest and require an increase in the peak inspiratory pressure.
- Order serial chest radiographs every 6 hours on the first day following chest trauma to rule out pneumothorax.[2]
- Refer the patient to a respiratory specialist within 24 hours of admission.
- Order a chest X-ray before chest tube removal to confirm the re-expansion of the affected lung.
Don'ts
- Don't remove the catheter from the 2nd intercostal space unless a chest tube is appropriately placed.
- Don't use large bore chest tubes.[1]
- Don't leave the chest tube more than 7 days, as it will increase the risk of infection.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group (2010). "Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010". Thorax. 65 Suppl 2: ii18–31. doi:10.1136/thx.2010.136986. PMID 20696690.
- ↑ 2.0 2.1 Sharma A, Jindal P (2008). "Principles of diagnosis and management of traumatic pneumothorax". J Emerg Trauma Shock. 1 (1): 34–41. doi:10.4103/0974-2700.41789. PMC 2700561. PMID 19561940.
<headertabs />