Nasopharyngeal carcinoma MRI: Difference between revisions
Jump to navigation
Jump to search
Homa Najafi (talk | contribs) (→MRI) |
m (Bot: Removing from Primary care) |
||
| (18 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}} {{AE}}{{Homa}}{{Faizan}} | {{CMG}} {{AE}}{{Homa}}{{Faizan}} | ||
==Overview== | ==Overview== | ||
Head and neck [[MRI]] may be helpful in the diagnosis of nasopharyngeal carcinoma. It is especially used for the assessment of [[tumor]] invasion in the [[skull]] [[base]], parapharyngeal spcae, [[paranasal sinus]], [[middle ear]] and [[cervical]] [[lymph node]]<nowiki/>s. | |||
==MRI== | ==MRI== | ||
[[MRI]] may be | [[MRI]] may be helpful in the [[diagnosis]] of Nasopharyngeal carcinoma. | ||
* Findings on [[MRI]] scan suggestive of nasopharyngeal carcinoma include:<ref>{{cite book | last = Hermans | first = R | title = Head and neck cancer imaging | publisher = Springer | location = Berlin New York | year = 2012 | isbn = 9783642178689 }}</ref> | |||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 600px" align="center" | {| style="border: 0px; font-size: 90%; margin: 3px; width: 600px" align="center" | ||
| valign="top" | | | valign="top" | | ||
| Line 47: | Line 18: | ||
:T1 | :T1 | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Typically isointense to muscle | *Typically [[isointense]] to [[muscle]] signal | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | | style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | ||
:T1 C+ (Gd) | :T1 C+ (Gd) | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Fat saturation in post contrast | *Fat saturation in post contrast sequences | ||
*Notable [[heterogeneous]] enhancement is typical | *Notable [[heterogeneous]] enhancement is typical | ||
*Perineural extension should be sought | *Perineural extension should be sought | ||
| Line 59: | Line 30: | ||
:T2 | :T2 | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Isointense to hyperintense to muscle | *Isointense to hyperintense to [[muscle]] signal | ||
*Fat saturation | *Fat saturation | ||
*Fluid in the middle ear can be helpful | *Fluid in the [[middle ear]] can be helpful | ||
|} | |} | ||
* The [[Protocol (natural sciences)|protocol]] for routine [[MRI]] of a nasopharyngeal [[mass]] includes:<ref name="Glastonbury2007">{{cite journal|last1=Glastonbury|first1=Christine M.|title=Nasopharyngeal Carcinoma|journal=Topics in Magnetic Resonance Imaging|volume=18|issue=4|year=2007|pages=225–235|issn=0899-3459|doi=10.1097/RMR.0b013e3181572b3a}}</ref><ref name="DubrulleSouillard2007">{{cite journal|last1=Dubrulle|first1=F.|last2=Souillard|first2=R.|last3=Hermans|first3=R.|title=Extension patterns of nasopharyngeal carcinoma|journal=European Radiology|volume=17|issue=10|year=2007|pages=2622–2630|issn=0938-7994|doi=10.1007/s00330-007-0616-z}}</ref><ref name="ChinFatterpekar2003">{{cite journal|last1=Chin|first1=Shy-Chyi|last2=Fatterpekar|first2=Girish|last3=Chen|first3=Cheng-Yu|last4=Som|first4=Peter M.|title=MR Imaging of Diverse Manifestations of Nasopharyngeal Carcinomas|journal=American Journal of Roentgenology|volume=180|issue=6|year=2003|pages=1715–1722|issn=0361-803X|doi=10.2214/ajr.180.6.1801715}}</ref><ref>{{Cite journal | |||
| author = [[Alfred L. Weber]], [[Sharif al-Arayedh]] & [[Asma Rashid]] | |||
| title = Nasopharynx: clinical, pathologic, and radiologic assessment | |||
| journal = [[Neuroimaging clinics of North America]] | |||
| volume = 13 | |||
| issue = 3 | |||
| pages = 465–483 | |||
| year = 2003 | |||
| month = August | |||
| pmid = 14631685 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Julian Goh]] & [[Keith Lim]] | |||
| title = Imaging of nasopharyngeal carcinoma | |||
| journal = [[Annals of the Academy of Medicine, Singapore]] | |||
| volume = 38 | |||
| issue = 9 | |||
| pages = 809–816 | |||
| year = 2009 | |||
| month = September | |||
| pmid = 19816641 | |||
}}</ref> | |||
** Unenhanced T1- weighted [[axial]] and [[sagittal plane]] [[images]] for: | |||
*** Detection of [[skull]] base invasion | |||
** T2-weighted fast spin-echo sequence in [[axial plane]] [[images]] for: | |||
*** Evaluation of early parapharyngeal [[tumor]] spread | |||
*** Invasion to the [[paranasal sinus]] | |||
*** Effusions of the [[middle ear]] | |||
*** Detection of [[cervical]] [[Lymph node|lymph nodes]]. | |||
** Contrast-enhanced T1-weighted [[axial]] and [[coronal plane]]<nowiki/>s [[images]] (with and without fat suppression) for: | |||
** Evaluation of [[tumor]] extension to the perineural and intracranial space. | |||
* Additional [[MRI]] component:<ref name="NgChan2009">{{cite journal|last1=Ng|first1=Shu-Hang|last2=Chan|first2=Sheng-Chieh|last3=Yen|first3=Tzu-Chen|last4=Chang|first4=Joseph Tung-Chieh|last5=Liao|first5=Chun-Ta|last6=Ko|first6=Sheung-Fat|last7=Wang|first7=Hung-Ming|last8=Wai|first8=Yau-Yau|last9=Wang|first9=Jiun-Jie|last10=Chen|first10=Min-Chi|title=Pretreatment evaluation of distant-site status in patients with nasopharyngeal carcinoma: accuracy of whole-body MRI at 3-Tesla and FDG-PET-CT|journal=European Radiology|volume=19|issue=12|year=2009|pages=2965–2976|issn=0938-7994|doi=10.1007/s00330-009-1504-5}}</ref><ref name="FongBhatia2010">{{cite journal|last1=Fong|first1=Devin|last2=Bhatia|first2=Kunwar S.S.|last3=Yeung|first3=David|last4=King|first4=Ann D.|title=Diagnostic accuracy of diffusion-weighted MR imaging for nasopharyngeal carcinoma, head and neck lymphoma and squamous cell carcinoma at the primary site|journal=Oral Oncology|volume=46|issue=8|year=2010|pages=603–606|issn=13688375|doi=10.1016/j.oraloncology.2010.05.004}}</ref><ref>{{Cite journal | |||
| author = [[Ann D. King]], [[David K. W. Yeung]], [[Anil T. Ahuja]], [[S. F. Leung]], [[Gary M. K. Tse]] & [[Andrew C. van Hasselt]] | |||
| title = In vivo proton MR spectroscopy of primary and nodal nasopharyngeal carcinoma | |||
| journal = [[AJNR. American journal of neuroradiology]] | |||
| volume = 25 | |||
| issue = 3 | |||
| pages = 484–490 | |||
| year = 2004 | |||
| month = March | |||
| pmid = 15037477 | |||
}}</ref> | |||
** Diffusion-weighted imaging for: | |||
*** Differentiating NPC from [[lymphoma]] | |||
*** Characterizing of [[cervical]] [[lymphadenopathy]] | |||
** [[Magnetic resonance imaging|MRI]] [[spectroscopy]] for: | |||
*** Differentiating of the NPC and [[metastatic]] nodes from normal [[neck]] [[muscle]]. | |||
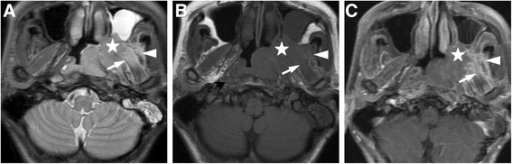
[[File:PMC4582819 13014 2015 513 Fig1 HTML (1).png|500px|none|thumb|source:https://openi.nlm.nih.gov/detailedresult?img=PMC4582819_13014_2015_513_Fig1_HTML&query=nasopharyngeal%20carcinoma&it=xg&req=4&npos=27]] | |||
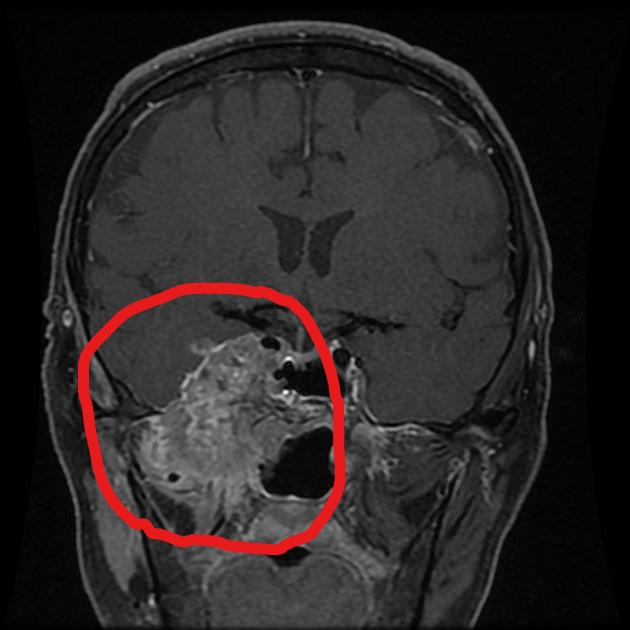
[[File:Nasopharyngeal carcinoma-Axial T1 MRI.jpg|500px|none|thumb|source:https://radiopaedia.org/cases/nasopharyngeal-carcinoma-8?lang=us]] | |||
[[File:Nasopharyngeal carcinoma MRI.jpg|500px|none|thumb|source:https://radiopaedia.org/cases/nasopharyngeal-carcinoma-8?lang=us]] | |||
MRI | |||
==References== | ==References== | ||
| Line 80: | Line 90: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[Category: | [[Category:Up-To-Date]] | ||
[[Category:Medicine]] | |||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Otolaryngology]] | [[Category:Otolaryngology]] | ||
[[Category:Radiology]] | |||
Latest revision as of 22:54, 29 July 2020
|
Nasopharyngeal carcinoma Microchapters |
|
Differentiating Nasopharyngeal carcinoma from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Nasopharyngeal carcinoma MRI On the Web |
|
American Roentgen Ray Society Images of Nasopharyngeal carcinoma MRI |
|
Risk calculators and risk factors for Nasopharyngeal carcinoma MRI |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Homa Najafi, M.D.[2]Faizan Sheraz, M.D. [3]
Overview
Head and neck MRI may be helpful in the diagnosis of nasopharyngeal carcinoma. It is especially used for the assessment of tumor invasion in the skull base, parapharyngeal spcae, paranasal sinus, middle ear and cervical lymph nodes.
MRI
MRI may be helpful in the diagnosis of Nasopharyngeal carcinoma.
| MRI Component | Features |
|---|---|
|
|
|
|
|
|
- The protocol for routine MRI of a nasopharyngeal mass includes:[2][3][4][5][6]
- Unenhanced T1- weighted axial and sagittal plane images for:
- Detection of skull base invasion
- T2-weighted fast spin-echo sequence in axial plane images for:
- Evaluation of early parapharyngeal tumor spread
- Invasion to the paranasal sinus
- Effusions of the middle ear
- Detection of cervical lymph nodes.
- Contrast-enhanced T1-weighted axial and coronal planes images (with and without fat suppression) for:
- Evaluation of tumor extension to the perineural and intracranial space.
- Unenhanced T1- weighted axial and sagittal plane images for:
- Additional MRI component:[7][8][9]
- Diffusion-weighted imaging for:
- Differentiating NPC from lymphoma
- Characterizing of cervical lymphadenopathy
- MRI spectroscopy for:
- Differentiating of the NPC and metastatic nodes from normal neck muscle.
- Diffusion-weighted imaging for:

References
- ↑ Hermans, R (2012). Head and neck cancer imaging. Berlin New York: Springer. ISBN 9783642178689.
- ↑ Glastonbury, Christine M. (2007). "Nasopharyngeal Carcinoma". Topics in Magnetic Resonance Imaging. 18 (4): 225–235. doi:10.1097/RMR.0b013e3181572b3a. ISSN 0899-3459.
- ↑ Dubrulle, F.; Souillard, R.; Hermans, R. (2007). "Extension patterns of nasopharyngeal carcinoma". European Radiology. 17 (10): 2622–2630. doi:10.1007/s00330-007-0616-z. ISSN 0938-7994.
- ↑ Chin, Shy-Chyi; Fatterpekar, Girish; Chen, Cheng-Yu; Som, Peter M. (2003). "MR Imaging of Diverse Manifestations of Nasopharyngeal Carcinomas". American Journal of Roentgenology. 180 (6): 1715–1722. doi:10.2214/ajr.180.6.1801715. ISSN 0361-803X.
- ↑ Alfred L. Weber, Sharif al-Arayedh & Asma Rashid (2003). "Nasopharynx: clinical, pathologic, and radiologic assessment". Neuroimaging clinics of North America. 13 (3): 465–483. PMID 14631685. Unknown parameter
|month=ignored (help) - ↑ Julian Goh & Keith Lim (2009). "Imaging of nasopharyngeal carcinoma". Annals of the Academy of Medicine, Singapore. 38 (9): 809–816. PMID 19816641. Unknown parameter
|month=ignored (help) - ↑ Ng, Shu-Hang; Chan, Sheng-Chieh; Yen, Tzu-Chen; Chang, Joseph Tung-Chieh; Liao, Chun-Ta; Ko, Sheung-Fat; Wang, Hung-Ming; Wai, Yau-Yau; Wang, Jiun-Jie; Chen, Min-Chi (2009). "Pretreatment evaluation of distant-site status in patients with nasopharyngeal carcinoma: accuracy of whole-body MRI at 3-Tesla and FDG-PET-CT". European Radiology. 19 (12): 2965–2976. doi:10.1007/s00330-009-1504-5. ISSN 0938-7994.
- ↑ Fong, Devin; Bhatia, Kunwar S.S.; Yeung, David; King, Ann D. (2010). "Diagnostic accuracy of diffusion-weighted MR imaging for nasopharyngeal carcinoma, head and neck lymphoma and squamous cell carcinoma at the primary site". Oral Oncology. 46 (8): 603–606. doi:10.1016/j.oraloncology.2010.05.004. ISSN 1368-8375.
- ↑ Ann D. King, David K. W. Yeung, Anil T. Ahuja, S. F. Leung, Gary M. K. Tse & Andrew C. van Hasselt (2004). "In vivo proton MR spectroscopy of primary and nodal nasopharyngeal carcinoma". AJNR. American journal of neuroradiology. 25 (3): 484–490. PMID 15037477. Unknown parameter
|month=ignored (help)