Deep vein thrombosis history and symptoms: Difference between revisions
Rim Halaby (talk | contribs) |
|||
| (25 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
'''Editor(s)-In-Chief:''' {{ATI}}, [[C. Michael Gibson, M.S., M.D.]] [mailto:charlesmichaelgibson@gmail.com]; | {| class="infobox" style="float:right;" | ||
|- | |||
| [[File:Siren.gif|30px|link=Deep vein thrombosis resident survival guide]]|| <br> || <br> | |||
| [[Deep vein thrombosis resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] | |||
|} | |||
'''Editor(s)-In-Chief:''' {{ATI}}, [[C. Michael Gibson, M.S., M.D.]] [mailto:charlesmichaelgibson@gmail.com]; {{AE}} {{CZ}} ; [[User:Kashish Goel|Kashish Goel, M.D.]]; [[User:Justine Cadet|Justine Cadet]]; {{Rim}} | |||
{{Deep vein thrombosis}} | {{Deep vein thrombosis}} | ||
==Overview== | ==Overview== | ||
A proper history and physical exam is very important for establishing an accurate diagnosis of deep vein thrombosis (DVT | A proper history and physical exam is very important for establishing an accurate diagnosis of deep vein thrombosis (DVT). DVT can be either asymptomatic or associated with tenderness and swelling of the calf or [[thigh]]. One of the first steps in the management of DVT is the determination of the [[Pretest probability of DVT#Wells score|Wells score for DVT]], whose criteria can be ascertained solely on the basis of history and physical exam. A high index of suspicion is also necessary to diagnose [[DVT]]. DVT can be complicated by [[pulmonary embolism]] (PE); therefore, it is important to inquire about the symptoms of [[PE]] among patients suspected to have DVT. | ||
==History== | ==History and Symptoms== | ||
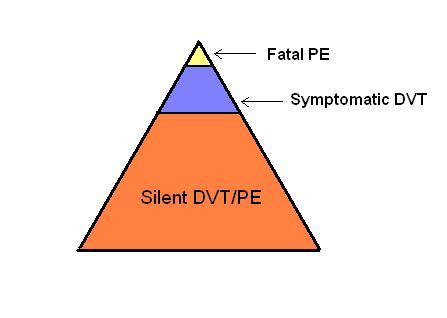
As depicted in the image below, the majority of patients with venous thromboembolism (VTE), that is [[DVT]], [[PE]], or both, are asymptomatic. | |||
[[File:Challenge of Assessing VTE.JPG|300x400px|The challenge in diagnosis of VTE]] | [[File:Challenge of Assessing VTE.JPG|300x400px|The challenge in diagnosis of VTE]] | ||
===Common Symptoms of DVT=== | |||
The classical symptoms of DVT include: | |||
* [[Pain and nociception|Pain]] in the affected area | |||
* [[Swelling]] of the affected area | |||
* [[Erythema]] around the affected area | |||
* [[Dilation]] of the surface veins and [[erythema]] of the overlying area | |||
However, sometimes there may be no symptoms referable to the location of the DVT. | |||
Shown below is a picture depicting unilateral swelling and redness in a leg affected with DVT. | |||
[[image:Deep vein thrombosis Unilateral leg swelling and redness.jpg|left|thumb|250px|Unilateral swelling and redness in a leg affected with DVT By James Heilman, MD - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=9444797]] | |||
<br style="clear:left" /> | |||
===Less Common Symptoms of DVT=== | |||
* In [[phlegmasia alba dolens]], the leg is pale and cold with a diminished arterial [[pulse]]. | |||
* In [[phlegmasia cerulea dolens]], there is an acute and near-total venous occlusion of the entire extremity outflow, including the [[iliac vein|iliac]] and [[femoral vein]]s. The leg is usually painful, [[cyanosis|cyanosed]] and [[edema|edematous]]. | |||
=== | ===Symptoms of PE=== | ||
Since VTE involves both DVT and [[PE]], the patient can present with complaints of either of the diseases. Therefore it is important to inquire about the symptoms of both diseases. Symptoms of PE include: | |||
* [[Dyspnea]] (78–81%)<ref name="pmid24182642">{{cite journal| author=Cohen AT, Dobromirski M, Gurwith MM| title=Managing pulmonary embolism from presentation to extended treatment. | journal=Thromb Res | year= 2014 | volume= 133 | issue= 2 | pages= 139-48 | pmid=24182642 | doi=10.1016/j.thromres.2013.09.040 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24182642 }} </ref> <br> | |||
* [[Pleuritic chest pain]] (39–56%)<ref name="pmid24182642">{{cite journal| author=Cohen AT, Dobromirski M, Gurwith MM| title=Managing pulmonary embolism from presentation to extended treatment. | journal=Thromb Res | year= 2014 | volume= 133 | issue= 2 | pages= 139-48 | pmid=24182642 | doi=10.1016/j.thromres.2013.09.040 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24182642 }} </ref> <br> | |||
* [[Fainting]] (22–26%)<ref name="pmid24182642">{{cite journal| author=Cohen AT, Dobromirski M, Gurwith MM| title=Managing pulmonary embolism from presentation to extended treatment. | journal=Thromb Res | year= 2014 | volume= 133 | issue= 2 | pages= 139-48 | pmid=24182642 | doi=10.1016/j.thromres.2013.09.040 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24182642 }} </ref> <br> | |||
* [[Cough]] (20%)<ref name="pmid18757870">{{cite journal| author=Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P et al.| title=Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). | journal=Eur Heart J | year= 2008 | volume= 29 | issue= 18 | pages= 2276-315 | pmid=18757870 | doi=10.1093/eurheartj/ehn310 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18757870 }} </ref><br> | |||
* [[Substernal chest pain]] (12%)<ref name="pmid18757870">{{cite journal| author=Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P et al.| title=Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). | journal=Eur Heart J | year= 2008 | volume= 29 | issue= 18 | pages= 2276-315 | pmid=18757870 | doi=10.1093/eurheartj/ehn310 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18757870 }} </ref><br> | |||
* [[Hemoptysis]] (11%)<ref name="pmid18757870">{{cite journal| author=Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P et al.| title=Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). | journal=Eur Heart J | year= 2008 | volume= 29 | issue= 18 | pages= 2276-315 | pmid=18757870 | doi=10.1093/eurheartj/ehn310 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18757870 }} </ref><br> | |||
* [[Wheezing]] <br> | |||
* [[Cyanosis]] (11%)<ref name="pmid24182642">{{cite journal| author=Cohen AT, Dobromirski M, Gurwith MM| title=Managing pulmonary embolism from presentation to extended treatment. | journal=Thromb Res | year= 2014 | volume= 133 | issue= 2 | pages= 139-48 | pmid=24182642 | doi=10.1016/j.thromres.2013.09.040 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24182642 }} </ref> <br> | |||
* [[Fever]] (7%)<ref name="pmid24182642">{{cite journal| author=Cohen AT, Dobromirski M, Gurwith MM| title=Managing pulmonary embolism from presentation to extended treatment. | journal=Thromb Res | year= 2014 | volume= 133 | issue= 2 | pages= 139-48 | pmid=24182642 | doi=10.1016/j.thromres.2013.09.040 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24182642 }} </ref> <br> | |||
* Symptoms suggestive of [[shock]] (in case of massive PE) | |||
** [[Altered mental status]] | |||
** [[Cold extremities]] | |||
** [[Cyanosis]] | |||
** [[Oliguria]] | |||
===Complete History=== | |||
If VTE is suspected or diagnosed, a complete history should be elicited, including the following: | |||
* '''Risk factors'''<ref name="pmid12814980">{{cite journal| author=Anderson FA, Spencer FA| title=Risk factors for venous thromboembolism. | journal=Circulation | year= 2003 | volume= 107 | issue= 23 Suppl 1 | pages= I9-16 | pmid=12814980 | doi=10.1161/01.CIR.0000078469.07362.E6 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12814980 }} </ref><ref name="pmid18757870">{{cite journal| author=Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P et al.| title=Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). | journal=Eur Heart J | year= 2008 | volume= 29 | issue= 18 | pages= 2276-315 | pmid=18757870 | doi=10.1093/eurheartj/ehn310 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18757870 }} </ref> | |||
** [[Chemotherapy]]<br> | |||
** [[Chronic heart failure]]<br> | |||
** [[Respiratory failure]]<br> | |||
** [[Hormone replacement therapy]]<br> | |||
** [[Cancer]]<br> | |||
** [[Oral contraceptive pills]] <br> | |||
** [[Stroke]] <br> | |||
** [[Pregnancy]] <br> | |||
** [[Postpartum]] <br> | |||
** Prior history of [[VTE]] <br> | |||
** [[Thrombophilia]] <br> | |||
** Advanced [[age]] <br> | |||
** [[Laparoscopic surgery]] <br> | |||
** Prepartum <br> | |||
** [[Obesity]] <br> | |||
** [[Varicose veins]] | |||
* '''Triggers'''<ref name="pmid12814980">{{cite journal| author=Anderson FA, Spencer FA| title=Risk factors for venous thromboembolism. | journal=Circulation | year= 2003 | volume= 107 | issue= 23 Suppl 1 | pages= I9-16 | pmid=12814980 | doi=10.1161/01.CIR.0000078469.07362.E6 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12814980 }} </ref><ref name="pmid18757870">{{cite journal| author=Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P et al.| title=Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). | journal=Eur Heart J | year= 2008 | volume= 29 | issue= 18 | pages= 2276-315 | pmid=18757870 | doi=10.1093/eurheartj/ehn310 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18757870 }} </ref> | |||
** [[Bone fracture]] ([[hip]] or [[leg]]) <br> | |||
** [[Hip replacement surgery]]<br> | |||
** Knee replacement surgery<br> | |||
** [[General surgery|Major general surgery]]<br> | |||
** [[Trauma|Significant trauma]]<br> | |||
** [[Spinal cord injury]]<br> | |||
** Athroscopic knee surgery<br> | |||
** [[Central venous line]]s<br> | |||
** [[Chemotherapy]]<br> | |||
** Bed rest for more than 3 days <br> | |||
** Prolonged car or air travel <br> | |||
** [[Laparoscopic surgery]] <br> | |||
** Prepartum <br> | |||
* '''Previous episode of [[VTE]]''' | |||
** Age | |||
** Location | |||
* '''Past medical history of diseases associated with hyperviscosity''' | |||
** [[Atherosclerosis]] | |||
** [[Collagen vascular disease]] | |||
** [[Heart failure]] | |||
** [[Myeloproliferative disease]] | |||
** [[Nephrotic syndrome]] | |||
** [[Autoimmune diseases]] | |||
**[[Polycythemia vera]] | |||
** [[Hyperhomocysteinemia]] | |||
** [[Paroxysmal nocturnal hemoglobinuria]] | |||
** [[Waldenstrom macroglobulinemia]] | |||
** [[Multiple myeloma]] | |||
* '''History of [[thrombophilia]]''' | |||
** [[Factor V Leiden mutation]] | |||
** [[Prothrombin gene mutation G20210A]] | |||
** [[Protein C]] or [[Protein S]] deficiency | |||
** [[Antithrombin]] (AT) deficiency | |||
** [[Antiphospholipid syndrome]] (APS) | |||
* '''Abortion''' | |||
** [[Abortion]] at second or third trimester of [[pregnancy]] (suggestive of an inherited [[thrombophilia]] or APS) | |||
* '''Drugs that may increase the risk of VTE''' | |||
** [[Hydralazine]] | |||
** [[Phenothiazine]] | |||
** [[Procainamide]] | |||
** [[Tamoxifen]] | |||
** [[Bevacizumab]] | |||
** [[Glucocorticoids]] | |||
* '''Family history (suggestive of [[inherited thrombophilia]])''' | |||
** Deep vein thrombosis | |||
** Pulmonary embolism | |||
** Recurrent [[miscarriage]] | |||
* '''Social history''' | |||
** Heavy [[cigarette smoking]] (>25 cigarettes per day) | |||
** [[Intravenous drug use]] (if injected directly in [[femoral vein]]) | |||
** [[Alcohol]] | |||
==References== | ==References== | ||
Latest revision as of 19:45, 6 March 2018
| Resident Survival Guide |
Editor(s)-In-Chief: The APEX Trial Investigators, C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2] ; Kashish Goel, M.D.; Justine Cadet; Rim Halaby, M.D. [3]
|
Deep Vein Thrombosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Deep vein thrombosis history and symptoms On the Web |
|
Risk calculators and risk factors for Deep vein thrombosis history and symptoms |
Overview
A proper history and physical exam is very important for establishing an accurate diagnosis of deep vein thrombosis (DVT). DVT can be either asymptomatic or associated with tenderness and swelling of the calf or thigh. One of the first steps in the management of DVT is the determination of the Wells score for DVT, whose criteria can be ascertained solely on the basis of history and physical exam. A high index of suspicion is also necessary to diagnose DVT. DVT can be complicated by pulmonary embolism (PE); therefore, it is important to inquire about the symptoms of PE among patients suspected to have DVT.
History and Symptoms
As depicted in the image below, the majority of patients with venous thromboembolism (VTE), that is DVT, PE, or both, are asymptomatic.
Common Symptoms of DVT
The classical symptoms of DVT include:
- Pain in the affected area
- Swelling of the affected area
- Erythema around the affected area
- Dilation of the surface veins and erythema of the overlying area
However, sometimes there may be no symptoms referable to the location of the DVT.
Shown below is a picture depicting unilateral swelling and redness in a leg affected with DVT.

Less Common Symptoms of DVT
- In phlegmasia alba dolens, the leg is pale and cold with a diminished arterial pulse.
- In phlegmasia cerulea dolens, there is an acute and near-total venous occlusion of the entire extremity outflow, including the iliac and femoral veins. The leg is usually painful, cyanosed and edematous.
Symptoms of PE
Since VTE involves both DVT and PE, the patient can present with complaints of either of the diseases. Therefore it is important to inquire about the symptoms of both diseases. Symptoms of PE include:
- Dyspnea (78–81%)[1]
- Pleuritic chest pain (39–56%)[1]
- Fainting (22–26%)[1]
- Cough (20%)[2]
- Substernal chest pain (12%)[2]
- Hemoptysis (11%)[2]
- Wheezing
- Cyanosis (11%)[1]
- Fever (7%)[1]
- Symptoms suggestive of shock (in case of massive PE)
Complete History
If VTE is suspected or diagnosed, a complete history should be elicited, including the following:
- Risk factors[3][2]
- Chemotherapy
- Chronic heart failure
- Respiratory failure
- Hormone replacement therapy
- Cancer
- Oral contraceptive pills
- Stroke
- Pregnancy
- Postpartum
- Prior history of VTE
- Thrombophilia
- Advanced age
- Laparoscopic surgery
- Prepartum
- Obesity
- Varicose veins
- Chemotherapy
- Triggers[3][2]
- Bone fracture (hip or leg)
- Hip replacement surgery
- Knee replacement surgery
- Major general surgery
- Significant trauma
- Spinal cord injury
- Athroscopic knee surgery
- Central venous lines
- Chemotherapy
- Bed rest for more than 3 days
- Prolonged car or air travel
- Laparoscopic surgery
- Prepartum
- Bone fracture (hip or leg)
- Previous episode of VTE
- Age
- Location
- Past medical history of diseases associated with hyperviscosity
- History of thrombophilia
- Factor V Leiden mutation
- Prothrombin gene mutation G20210A
- Protein C or Protein S deficiency
- Antithrombin (AT) deficiency
- Antiphospholipid syndrome (APS)
- Abortion
- Abortion at second or third trimester of pregnancy (suggestive of an inherited thrombophilia or APS)
- Drugs that may increase the risk of VTE
- Family history (suggestive of inherited thrombophilia)
- Deep vein thrombosis
- Pulmonary embolism
- Recurrent miscarriage
- Social history
- Heavy cigarette smoking (>25 cigarettes per day)
- Intravenous drug use (if injected directly in femoral vein)
- Alcohol
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Cohen AT, Dobromirski M, Gurwith MM (2014). "Managing pulmonary embolism from presentation to extended treatment". Thromb Res. 133 (2): 139–48. doi:10.1016/j.thromres.2013.09.040. PMID 24182642.
- ↑ 2.0 2.1 2.2 2.3 2.4 Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P; et al. (2008). "Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC)". Eur Heart J. 29 (18): 2276–315. doi:10.1093/eurheartj/ehn310. PMID 18757870.
- ↑ 3.0 3.1 Anderson FA, Spencer FA (2003). "Risk factors for venous thromboembolism". Circulation. 107 (23 Suppl 1): I9–16. doi:10.1161/01.CIR.0000078469.07362.E6. PMID 12814980.