Deep vein thrombosis pathophysiology
| https://https://www.youtube.com/watch?v=mMEdNCdUeAE%7C350}} |
| Resident Survival Guide |
Editor(s)-In-Chief: The APEX Trial Investigators, C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2] ; Kashish Goel, M.D.; Assistant Editor(s)-In-Chief: Justine Cadet
|
Deep Vein Thrombosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Deep vein thrombosis pathophysiology On the Web |
|
Risk calculators and risk factors for Deep vein thrombosis pathophysiology |
Overview
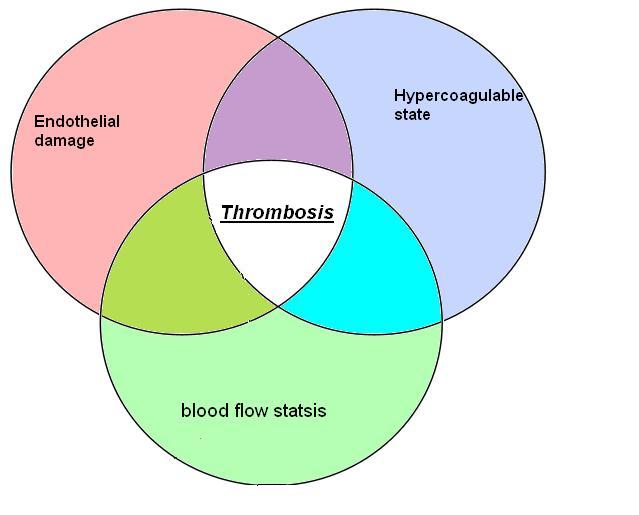
Deep vein thrombosis (DVT) results from the formation of a blood clot in the deep veins. Three mechanisms predispose to DVT, they are collectively described as the Virchow's triad. 1. Alterations in blood flow (stasis): Venous stasis is a major risk factor for the development of thrombosis. It occurs in certain pathological conditions (as in heart failure) wherein it causes an increase in platelet to endothelium contact and decreases the dilution of clotting factors. This increases the risk of clot formation, and it forms microthrombi, which further grow and propagate. 2. Injury to the vascular endothelium (Endothelial dysfunction): Intrinsic or secondary to external trauma, such as catheterization, can cause intimal damage and stimulate clot formation. 3. Alterations in the constitution of blood (Hypercoagulability): Abnormal changes in coagulation can increase the propensity to develop thrombosis.
Pathophysiology
Virchow's Triad
- Virchow's triad describes the three broad categories of factors that are thought to contribute to thrombosis.[1][2]
- Alterations in blood flow
- Vascular endothelial injury
- Alterations in the constitution of the blood
Shown below is a table depicting the elements of Virchow's triad and their modern counterparts.
| Virchow's[3] | Modern | Notes |
|---|---|---|
| Phenomena of interrupted blood-flow | "Stasis" or "venous stasis"[4] | The first category, alterations in normal blood flow, refers to several situations. These include turbulence, stasis, mitral stenosis, and varicose veins. The equivalence of Virchow's version and the modern version has been disputed.[5] |
| Phenomena associated with irritation of the vessel and its vicinity | "Endothelial injury" or "vessel wall injury" | The second category, injuries and/or trauma to endothelium includes damage to the veins arising from shear stress or hypertension. |
| Phenomena of blood-coagulation | "Hypercoagulability" | The last category, alterations in the constitution of blood,[6] has numerous possible risk factors such as hyperviscosity, deficiency of antithrombin III, nephrotic syndrome, changes after severe trauma or burn, disseminated cancer, late pregnancy and delivery, race, age, whether the patient is a smoker, and obesity. All of these risk factors lead to hypercoagulability. |
Thrombus Formation
- Normal homeostasis is maintained by the balance between the coagulation and fibrinolysis systems of the body. A homeostatic imbalance leads to the formation of a thrombus or hemorrhage.
- Factors that increase the risk for a homeostatic imbalance include:
- Thrombophilia
- Immobilization
- Trauma
- An insult to homeostatic balance can expose the sub-endothelium and lead to the collection of various coagulation factors. Accumulation of coagulation factors can lead to the formation of a thrombus of red blood cells, leukocytes, and fibrin.
- A thrombus is characteristically found to first develop in the calf veins and progressively grow in the direction of blood flow (leading to the heart).
- An exceedingly extensive DVT can extend well into the iliac veins or the inferior vena cava.
Shown below is an image depicting a thrombus formed in the deep vein of the leg.

Source: Wikipedia [7]
Venous Insufficiency
- In patients with DVT, there is a potential to develop chronic venous insufficiency, also known as post-phlebitic syndrome.
- At 10 years of follow-up, the incidence of venous insufficiency is around 30%.
- Valvular incompetence is the mechanism responsible for venous insufficiency development. Valves within the deep veins may be involved early in the formation of a deep vein thrombus (DVT) and subsequently become damaged. This damage causes a lack of blood flow back into the involved veins. When the calf muscle is contracted, the blood moves to superficial veins and can ultimately lead to superficial venous insufficiency.
Special Conditions
- May-Thurner syndrome: As a result of the right common iliac artery compressing the left common iliac vein, DVTs occur more commonly in left leg vasculature than the right.
- Phlegmasia alba dolens: Following an acute episode of DVT, the leg may turn a milky white color. Causation is not clear but may be linked to edema-induced compartment syndrome resulting in tissue ischemia and gangrene.
- Phlegmasia cerulea dolens: Complete occlusion of the venous flow secondary to massive ilio-femoral thrombus and excessive edema.
Video: The Process of Thrombosis
{{#ev:youtube|CETfozL0cQg}}
{{#ev:youtube|X_POCRsy7i4}}
Pathophysiology in Upper Extremity DVT
- While approximately 80% of upper extremity DVT are secondary, only 20% of the cases are primary.[8]
- Primary upper extremity DVT occurs in the following conditions:[8]
- Venous thoracic outlet syndrome caused by compression of the subclavian vein
- Paget Schroetter syndrome caused by repetitive trauma to the subclavian vein due to repetitive overhead arm movement
- Idiopathic etiology
- Secondary upper extremity DVT occurs in the following conditions:[8]
- Catheter associated thrombosis
- Indwelling central venous catheter
- Pacemaker
- Defibrillator
- Cancer and chemotherapy
- Surgery or trauma to the upper extremities that predisposes to thrombosis due to injury of the veins, compression of the veins, immobilization, or placement of plaster cast.
- Hormone-induced hypercoagulabity in pregnancy or due to oral contraceptive intake
- Catheter associated thrombosis
References
- ↑ April Wang Armstrong; David E. Golan; Armen H. Tashjian; Ehrin Armstrong (2008). Principles of pharmacology: the pathophysiologic basis of drug therapy. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 396. ISBN 0-7817-8355-0.
- ↑ Bagot CN, Arya R (2008). "Virchow and his triad: a question of attribution". Br. J. Haematol. 143 (2): 180–90. doi:10.1111/j.1365-2141.2008.07323.x. PMID 18783400. Unknown parameter
|month=ignored (help) - ↑ Agutter, Paul S. (2008). The Aetiology of Deep Venous Thrombosis: A Critical, Historical and Epistemological Survey. Berlin: Springer. p. 84. ISBN 1-4020-6649-X.
- ↑ Lowe GD (2003). "Virchow's triad revisited: abnormal flow". Pathophysiol. Haemost. Thromb. 33 (5–6): 455–7. doi:10.1159/000083845. PMID 15692260.
- ↑ "Further reflections on Virchow's triad. - Free Online Library". Retrieved 2009-02-10.
- ↑ Chung I, Lip GY (2003). "Virchow's triad revisited: blood constituents". Pathophysiol. Haemost. Thromb. 33 (5–6): 449–54. doi:10.1159/000083844. PMID 15692259.
- ↑ Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. - Obra do próprio
- ↑ Jump up to: 8.0 8.1 8.2 Kucher N (2011). "Clinical practice. Deep-vein thrombosis of the upper extremities". N Engl J Med. 364 (9): 861–9. doi:10.1056/NEJMcp1008740. PMID 21366477.