Clostridium perfringens: Difference between revisions
Becca Cohen (talk | contribs) No edit summary |
Ahmed Younes (talk | contribs) |
||
| (7 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
{{Taxobox | {{Taxobox | ||
| image = Clostridium_perfringens.jpg | | image = Clostridium_perfringens.jpg | ||
| image_width = 240px | | image_width = 240px | ||
| image_caption = Photomicrograph of gram-positive ''Clostridium | | image_caption = Photomicrograph of gram-positive ''Clostridium perfringens'' bacilli. | ||
| regnum = [[ | | regnum = [[Bacteria]] | ||
| | | phylum = [[Firmicutes]] | ||
| classis = [[Clostridia]] | | classis = [[Clostridia]] | ||
| ordo = [[Clostridia]]les | | ordo = [[Clostridia]]les | ||
| Line 13: | Line 11: | ||
| species = '''''C. perfringens''''' | | species = '''''C. perfringens''''' | ||
| binomial = ''Clostridium perfringens'' | | binomial = ''Clostridium perfringens'' | ||
| binomial_authority = Veillon & Zuber 1898<br>Hauduroy ''et al.'' 1937 | | binomial_authority = Veillon & Zuber 1898<br />Hauduroy ''et al.'' 1937 | ||
}} | }} | ||
{{ | __NOTOC__ | ||
{{About0|Gas gangrene}} | |||
{{Gas gangrene}} | |||
{{CMG}} | |||
'''''Clostridium perfringens''''' (formerly known as ''C. welchii,'' or ''Bacillus welchii'') is a [[Gram-positive]], rod-shaped, [[anaerobic bacterium|anaerobic]], [[Endospore|spore-forming]] [[bacterium]] of the genus ''[[Clostridium]]''.<ref name=Sherris>{{cite book | author = Ryan KJ; Ray CG (editors) | title = Sherris Medical Microbiology | edition = 4th | publisher = McGraw Hill | year = 2004|isbn = 0-8385-8529-9 }}{{Page needed|date=April 2011}}</ref> ''C. perfringens'' is everpresent in nature and can be found as a normal component of decaying vegetation, [[Pelagic sediment|marine sediment]], the [[Gut flora|intestinal tract of humans]] and other [[vertebrate]]s, [[insect]]s, and [[soil]]. It has the shortest reported generation time of any organism at 6.3 minutes in [[thioglycollate broth|thioglycollate]] medium.<ref name=bionumbers>http://bionumbers.hms.harvard.edu//bionumber.aspx?id=105474&ver=1</ref> | |||
''C. perfringens'' is the third most common cause of [[food poisoning]] in the United Kingdom and the United States though it can sometimes be ingested and cause no harm. | |||
'' | Infections due to ''C. perfringens'' show evidence of tissue [[necrosis]], [[bacteremia]], [[emphysema]]tous [[cholecystitis]], and [[gas gangrene]], which is also known as clostridial [[myonecrosis]]. The toxin involved in [[gas gangrene]] is known as [[Clostridium perfringens alpha toxin|α-toxin]], which inserts into the plasma membrane of cells, producing gaps in the membrane that disrupt normal cellular function. ''C. perfringens'' can participate in polymicrobial [[anaerobic infection]]s. ''Clostridium perfringens ''is commonly encountered in [[infection]]s as a component of the normal [[flora (microbiology)|flora]]. In this case, its role in disease is minor. | ||
The action of ''C. perfringens'' on dead bodies is known to [[mortuary]] workers as [[tissue gas]] and can be halted only by [[embalming]]. | |||
''C. perfringens'' is | |||
==Food poisoning== | |||
In the United Kingdom and United States, ''C. perfringens'' bacteria are the third most common cause of foodborne illness, with poorly prepared meat and poultry, or food properly prepared but left to stand too long, the main culprits in harboring the bacterium.<ref name="O.T.M">{{cite book | author = Warrell | title = Oxford Textbook of Medicine | edition = 4th | publisher = Oxford University Press | year = 2003 | isbn = 0-19-262922-0 |display-authors=etal}}{{Page needed|date=April 2011}}</ref> The [[clostridium perfringens enterotoxin]] (CPE) mediating the disease is heat-labile (inactivated at {{convert|74|C|F}}). It can be detected in contaminated food (if not heated properly), and feces.<ref name=M.D.T>{{cite book | author = Murray | title = Medical Microbiology | edition = 6th | publisher = Mosby Elsevier | year = 2009 | isbn = 978-0-323-05470-6 |display-authors=etal}}{{Page needed|date=April 2011}}</ref> Incubation time is between six and 24 (commonly 10-12) hours after ingestion of contaminated food. | |||
Since ''C. perfringens'' forms spores that can withstand cooking temperatures, if cooked food is let stand for long enough, germination can ensue and infective bacterial colonies develop. Symptoms typically include abdominal cramping, diarrhea; vomiting and fever are usual. The whole course usually resolves within 24 hours. Very rare, fatal cases of [[clostridial necrotizing enteritis]] (also known as pigbel) have been known to involve "Type C" strains of the organism, which produce a potently ulcerative [[Clostridium perfringens beta toxin|β-toxin]]. This strain is most frequently encountered in [[Papua New Guinea]]. | |||
Many cases of ''C. perfringens'' food poisoning likely remain [[subclinical]], as [[antibody|antibodies]] to the toxin are common among the population. This has led to the conclusion that most of the population has experienced food poisoning due to ''C. perfringens''. | |||
Despite its potential dangers, ''C. perfringens'' is used as the [[leavening agent]] in [[salt rising bread]]. The baking process is thought to reduce the bacterial contamination, precluding negative effects.<ref>{{cite journal|last1=Juckett|first1=Gregory|last2=et al|title=The Microbiology of Salt Rising Bread|journal=West Virginia Medical Journal|date=November 2008|issue=22|url=http://mediad.publicbroadcasting.net/p/wvpn/files/201404/microbiologySRB.pdf|accessdate=22 July 2015}}</ref> | |||
== | == Infection == | ||
''Clostridium perfringens'' is the most common bacterial agent for [[gas gangrene]], which is necrosis, putrefaction of tissues, and gas production. It is caused primarily by [[Clostridium perfringens alpha toxin]]. The gases form bubbles in muscle (crepitus) and the characteristic smell in decomposing tissue. After rapid and destructive local spread (which can take only hours), systemic spread of bacteria and bacterial toxins may cause death. This is a problem in major trauma and in military contexts. ''C. perfringens'' grows readily on blood agar plate in anaerobic conditions, and often produces a double zone of beta hemolysis. | |||
Research published in 2014 suggested that a strain of ''C. perfringens'' might be implicated in [[multiple sclerosis]] (MS). Tests in [[Laboratory mouse|mice]] found that a toxin made by a rare strain of ''C. perfringens'' caused MS-like damage in the brain, and earlier work had identified this strain of ''C. perfringens'' in a human with MS.<ref>{{cite web | url=http://www.bbc.co.uk/news/health-25925658 | title=Multiple sclerosis 'linked to food bug' | publisher=BBC | date=29 January 2014 | accessdate=29 January 2014}}</ref> MS patients were found to be ten times more immune-reactive to the epsilon toxin than healthy people.<ref>http://www.foxnews.com/health/2014/01/29/bacterial-toxin-may-trigger-multiple-sclerosis-research-finds/?intcmp=trending</ref> | |||
== | == Diagnosis == | ||
''C. perfringens'' can be diagnosed by [[Nagler's reaction]] where the suspect organism is cultured on an egg yolk media plate. One side of the plate contains anti-alpha-toxin, while the other side does not. A streak of suspect organism is placed through both sides. An area of turbidity will form around the side that does not have the anti-alpha-toxin, indicating uninhibited [[lecithinase]] activity. | |||
Other tests/reactions: Catalase: Negative, Spot indole: Positive, Lecithinase: Positive, Lipase: Negative, Litmus Milk: Stormy Fermentation, Reverse CAMP plate: Positive, Gas Liquid Chromatography products: (Acetic, Butyric and Lactic Acids). | |||
==Differential diagnosis== | |||
Clostridium perfringens infection must be differentiated from other causes of viral, bacterial, and parasitic gastroentritis. | |||
< | {| style="border: 0px; font-size: 90%; margin: 3px;" align=center | ||
! colspan="3" rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Organism | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Age predilection | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Travel History | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Incubation Size (cell) | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Incubation Time | |||
! colspan="3" align="center" style="background:#4479BA; color: #FFFFFF;"|History and Symptoms | |||
! colspan="4" align="center" style="background:#4479BA; color: #FFFFFF;"|Diarrhea type8 | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Food source | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Specific consideration | |||
|- | |||
!style="background:#4479BA; color: #FFFFFF|Fever | |||
!style="background:#4479BA; color: #FFFFFF|N/V | |||
!style="background:#4479BA; color: #FFFFFF|Cramping Abd Pain | |||
!style="background:#4479BA; color: #FFFFFF|Small Bowel | |||
!style="background:#4479BA; color: #FFFFFF|Large Bowel | |||
!style="background:#4479BA; color: #FFFFFF|Inflammatory | |||
!style="background:#4479BA; color: #FFFFFF|Non-inflammatory | |||
|- | |||
| rowspan="4" align="center" style="background:#4479BA; color: #FFFFFF;"|'''Viral''' | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Rotavirus]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<2 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<10<sup>2</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<48 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Mostly in day cares, most common in winter. | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Norovirus]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any age | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10 -10<sup>3</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |24-48 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Most common cause of gastroenteritis, abdominal tenderness, | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Adenoviridae|Adenovirus]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<2 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>5</sup> -10<sup>6</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |8-10 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |No seasonality | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Astrovirus]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<5 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |72-96 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Seafood | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Mostly during winter | |||
|- | |||
| rowspan="11" align="center" style="background:#4479BA; color: #FFFFFF;"|'''Bacterial''' | |||
| rowspan="5" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Escherichia coli]]'' | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[ETEC]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any age | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>8</sup> -10<sup>10</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |24 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Causes travelers diarrhea, contains heat-labile toxins (LT) and heat-stable toxins (ST) | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[EPEC]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<1 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>†</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |6-12 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Raw beef and chicken | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[EIEC]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>†</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |24 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Hamburger meat and unpasteurized milk | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Similar to [[shigellosis]], can cause bloody diarrhea | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[EHEC]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10 | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |3-4 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Undercooked or raw hamburger (ground beef) | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Known as ''[[Escherichia coli O157:H7|E. coli]]'' [[Escherichia coli O157:H7|O157:H7]], can cause [[Hemolytic-uremic syndrome|HUS]]/[[TTP]]. | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[EAEC]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>10</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |8-18 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause prolonged or persistent diarrhea in children | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Salmonella|Salmonella sp.]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1 | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |6 to 72 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Meats, poultry, eggs, milk and dairy products, fish, shrimp, spices, yeast, coconut, sauces, freshly prepared salad. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Can cause [[salmonellosis]] or [[typhoid fever]]. | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Shigella|Shigella sp.]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10 - 200 | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |8-48 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Raw foods, for example, lettuce, salads (potato, tuna, shrimp, macaroni, and chicken) | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Some strains produce enterotoxin and Shiga toxin similar to those produced by E. coli O157:H7 | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Campylobacter|Campylobacter sp.]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<5 y, 15-29 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>4</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |2-5 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Undercooked poultry products, unpasteurized milk and cheeses made from unpasteurized milk, vegetables, seafood and contaminated water. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause [[bacteremia]], [[Guillain-Barré syndrome]] (GBS), [[Hemolytic-uremic syndrome|hemolytic uremic syndrome]] (HUS) and recurrent [[colitis]] | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Yersinia enterocolitica]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<10 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>4</sup> -10<sup>6</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1-11 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Meats (pork, beef, lamb, etc.), oysters, fish, crabs, and raw milk. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause [[reactive arthritis]]; [[glomerulonephritis]]; [[endocarditis]]; [[erythema nodosum]]. | |||
can mimic [[appendicitis]] and mesenteric [[lymphadenitis]]. | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Clostridium perfringens]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |> 10<sup>6</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |16 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Meats (especially beef and poultry), meat-containing products (e.g., gravies and stews), and Mexican foods. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Can survive high heat, | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Vibrio cholerae]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>6</sup>-10<sup>10</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |24-48 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Seafoods, including molluscan shellfish (oysters, mussels, and clams), crab, lobster, shrimp, squid, and finfish. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Hypotension]], [[tachycardia]], decreased [[Turgor|skin turgor]]. Rice-water stools | |||
|- | |||
| rowspan="7" align="center" style="background:#4479BA; color: #FFFFFF;"|'''Parasites''' | |||
| rowspan="4" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Protozoa | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Giardia lamblia]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |2-5 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1 cyst | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1-2 we | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Contaminated water | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause [[malabsorption syndrome]] and severe [[weight loss]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Entamoeba histolytica]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |4-11 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<10 cysts | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |2-4 we | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Contaminated water and raw foods | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause intestinal amebiasis and amebic liver abscess | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Cryptosporidium parvum]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10-100 oocysts | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |7-10 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Juices and milk | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause copious diarrhea and [[dehydration]] in patients with [[AIDS]] especially with 180 > [[CD4|CD<sub>4</sub>]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Cyclospora cayetanensis]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10-100 oocysts | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |7-10 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Fresh produce, such as raspberries, basil, and several varieties of lettuce. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |More common in rainy areas | |||
|- | |||
| rowspan="3" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Helminths | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Trichinella]]'' [[Trichinella|spp]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Two viable larvae (male and female) | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1-4 we | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Undercooked meats | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |More common in hunters or people who eat traditionally uncooked meats | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Taenia (tapeworm)|Taenia]]'' [[Taenia (tapeworm)|spp]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1 larva or egg | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |2-4 m | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Undercooked beef and pork | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Neurocysticercosis]]: Cysts located in the brain may be asymptomatic or [[seizures]], increased [[intracranial pressure]], [[headache]]. | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Diphyllobothrium|Diphyllobothrium latum]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1 larva | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |15 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Raw or undercooked fish. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause vitamin B<sub>12</sub> deficiency | |||
|} | |||
<br><br> | |||
<small><small> | |||
8'''Small bowel diarrhea''': watery, voluminous with less than 5 WBC/high power field | |||
'''Large bowel diarrhea''': Mucousy and/or bloody with less volume and more than 10 WBC/high power field<br> | |||
† It could be as high as 1000 based on patient's immunity system. | |||
</small></small> | |||
'''The table below summarizes the findings that differentiate inflammatory causes of chronic diarrhea'''<ref name="pmid8209928">{{cite journal| author=Konvolinka CW| title=Acute diverticulitis under age forty. | journal=Am J Surg | year= 1994 | volume= 167 | issue= 6 | pages= 562-5 | pmid=8209928 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8209928 }} </ref><ref name="pmid16151544">{{cite journal| author=Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR et al.| title=Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. | journal=Can J Gastroenterol | year= 2005 | volume= 19 Suppl A | issue= | pages= 5A-36A | pmid=16151544 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16151544 }} </ref><ref name="pmid16698746">{{cite journal| author=Satsangi J, Silverberg MS, Vermeire S, Colombel JF| title=The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. | journal=Gut | year= 2006 | volume= 55 | issue= 6 | pages= 749-53 | pmid=16698746 | doi=10.1136/gut.2005.082909 | pmc=1856208 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16698746 }} </ref><ref name="pmid12700377">{{cite journal| author=Haque R, Huston CD, Hughes M, Houpt E, Petri WA| title=Amebiasis. | journal=N Engl J Med | year= 2003 | volume= 348 | issue= 16 | pages= 1565-73 | pmid=12700377 | doi=10.1056/NEJMra022710 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12700377 }} </ref><ref name="pmid12700377">{{cite journal| author=Haque R, Huston CD, Hughes M, Houpt E, Petri WA| title=Amebiasis. | journal=N Engl J Med | year= 2003 | volume= 348 | issue= 16 | pages= 1565-73 | pmid=12700377 | doi=10.1056/NEJMra022710 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12700377 }} </ref> | |||
{| class="wikitable" | |||
!Cause | |||
!History | |||
!Laboratory findings | |||
!Diagnosis | |||
!Treatment | |||
|- | |||
|[[Diverticulitis]] | |||
| | |||
* [[Bloody diarrhea]] | |||
* Left lower quadrant [[abdominal pain]] | |||
* [[Abdominal tenderness]] on [[physical examination]] | |||
* Low grade [[fever]] | |||
| | |||
* [[Leukocytosis]] | |||
* Elevated serum [[amylase]] and [[lipase]] | |||
* [[Sterile]] [[pyuria]] on [[urinalysis]] | |||
|Abdominal [[CT scan]] with oral and intravenous [[Contrast medium|(IV) contrast]] | |||
|bowel rest, [[Intravenous fluids|IV fluid]] resuscitation, and [[Broad-spectrum antibiotic|broad-spectrum antimicrobial therapy]] which covers [[Anaerobic organism|anaerobic]] [[bacteria]] and [[gram-negative]] [[Bacteria|rods]] | |||
|- | |||
|[[Ulcerative colitis]] | |||
| | |||
* [[Diarrhea]] mixed with blood and [[mucus]], of gradual onset. | |||
* Signs of [[weight loss]] | |||
* [[Rectal pain|Rectal urgency]] | |||
* [[Tenesmus]] | |||
* [[Blood]] is often noticed on underwear | |||
* Different degrees of [[abdominal pain]] | |||
| | |||
* [[Anemia]] | |||
* [[Thrombocytosis]] | |||
* A high [[platelet]] count | |||
* Elevated [[ESR]] (>30mm/hr) | |||
* Low [[albumin]] | |||
|[[Endoscopy]] | |||
|Induction of [[Remission (medicine)|remission]] with [[mesalamine]] and [[corticosteroids]] followed by the administration of [[sulfasalazine]] and [[Mercaptopurine|6-Mercaptopurine]] depending on the severity of the [[disease]]. | |||
|- | |||
|[[Entamoeba histolytica]] | |||
| | |||
* [[Abdominal cramps]] | |||
* [[Diarrhea]] | |||
** Passage of 3 - 8 semiformed [[stools]] per day | |||
** Passage of soft [[stools]] with [[mucus]] and occasional [[blood]] | |||
* [[Fatigue]] | |||
* [[Intestinal]] gas (excessive [[flatus]]) | |||
* [[Rectal pain]] while having a [[bowel movement]] ([[tenesmus]]) | |||
* Unintentional [[weight loss]] | |||
|cysts shed with the stool | |||
|detects ameba [[DNA]] in feces | |||
|[[Amebic dysentery]] | |||
* [[Metronidazole]] 500-750mg three times a day for 5-10 days | |||
* [[Tinidazole]] 2g once a day for 3 days is an alternative to [[metronidazole]] | |||
Luminal amebicides for ''[[E. histolytica]]'' in the [[colon]]: | |||
* [[Paromomycin]] 500mg three times a day for 10 days | |||
* [[Diloxanide furoate]] 500mg three times a day for 10 days | |||
* [[Iodoquinol]] 650mg three times a day for 20 days | |||
For [[Amoebiasis|amebic liver abscess]]: | |||
* [[Metronidazole]] 400mg three times a day for 10 days | |||
* [[Tinidazole]] 2g once a day for 6 days is an alternative to [[metronidazole]] | |||
* [[Diloxanide furoate]] 500mg three times a day for 10 days must always be given afterwards. | |||
|} | |||
==Food poisoning incidents== | |||
On May 7, 2010, 42 residents and 12 staff members at a Louisiana state psychiatric hospital experienced vomiting, abdominal cramps, and diarrhea. Within 24 hours, three patients had died. The outbreak was linked to chicken which was cooked a day prior to being served and was not cooled down according to hospital guidelines. The outbreak affected 31% of the residents of the hospital and 69% of the staff who ate the chicken. It is unknown how many of the affected residents ate the chicken.<ref>{{cite web|title=Fatal Foodborne Clostridium perfringens Illness at a State Psychiatric Hospital — Louisiana, 2010|url=http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6132a1.htm|work=Centers for Disease Control and Prevention|accessdate=16 November 2013}}</ref> | |||
In May 2011, a man died after allegedly eating food contaminated with the bacteria on a [[Transatlantic flight|transatlantic]] [[American Airlines]] flight. The man's wife and daughter are suing American and [[LSG Sky Chefs]], the German company that prepared the inflight food.<ref>{{cite web|last=Mohn |first=Tanya |url=http://overheadbin.msnbc.msn.com/_news/2011/12/01/9146822-passenger-dies-in-flight-family-says-airline-to-blame |title=Overhead Bin - Passenger dies in-flight, family says airline to blame |publisher=Overheadbin.msnbc.msn.com |date= |accessdate=2012-02-13}}</ref> | |||
In December 2012, a 46-year-old woman died two days after eating a Christmas Day meal at a pub in [[Hornchurch]], [[Essex]], [[England]]. She was among about 30 people to fall ill after eating the meal. Samples taken from the victims contained ''C.perfringens''. The hotel manager and the cook were jailed for offences arising from the incident.<ref>{{cite news|title=Pub chef and manager jailed over Christmas dinner that left a diner dead|url=http://www.theguardian.com/uk-news/2015/jan/23/pub-chef-manager-jailed-christmas-dinner-diner-dead|accessdate=3 August 2015|work=[[The Guardian]]|date=23 January 2015}}</ref> | |||
</ | In December 2014, 87 year old Bessie Scott died three days after eating a church potluck supper in [[Nackawic]], [[New Brunswick]], [[Canada]]. Over 30 other people reported signs of gastrointestinal illness, diarrhea and abdominal pain. The province's acting chief medical officer says ''Clostridium perfringens'' is the bacteria that most likely caused the woman’s death.<ref>{{cite news|url=http://www.cbc.ca/news/canada/new-brunswick/woman-s-death-likely-caused-by-bacteria-from-christmas-supper-1.2870869|title=Woman's death likely caused by bacteria from Christmas supper|publisher=''[[Canadian Broadcasting Corporation|CBC]]''|date=12 December 2014}}</ref> | ||
==References== | ==References== | ||
{{ | {{reflist|2}} | ||
==External links== | ==External links== | ||
* [http://patricbrc.org/portal/portal/patric/Taxon?cType=taxon&cId=1502 Clostridium perfringens] genomes and related information at [http://patricbrc.org/ PATRIC], a Bioinformatics Resource Center funded by [http://www.niaid.nih.gov/ NIAID] | |||
* [http://pathema.jcvi.org/cgi-bin/Clostridium/PathemaHomePage.cgi Pathema-''Clostridium'' Resource] | |||
{{Gram-positive firmicutes diseases}} | |||
{{Toxins}} | |||
{{Consumer Food Safety}} | |||
{{Authority control}} | |||
{{DEFAULTSORT:Clostridium Perfringens}} | |||
[[Category:Clostridiaceae]] | [[Category:Clostridiaceae]] | ||
[[Category: | [[Category:Gas gangrene]] | ||
[[Category: | [[Category:Gram-positive bacteria]] | ||
[[Category:Bacteria with sequenced genomes]] | |||
[[ | |||
Latest revision as of 01:20, 11 September 2017
| style="background:#Template:Taxobox colour;"|Template:Taxobox name | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
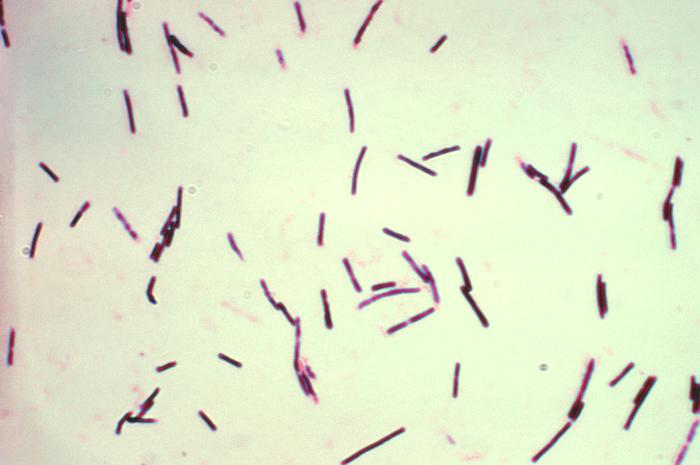 Photomicrograph of gram-positive Clostridium perfringens bacilli.
| ||||||||||||||
| style="background:#Template:Taxobox colour;" | Scientific classification | ||||||||||||||
| ||||||||||||||
| Binomial name | ||||||||||||||
| Clostridium perfringens Veillon & Zuber 1898 Hauduroy et al. 1937 |
|
Gas gangrene Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Clostridium perfringens On the Web |
|
American Roentgen Ray Society Images of Clostridium perfringens |
|
Risk calculators and risk factors for Clostridium perfringens |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Clostridium perfringens (formerly known as C. welchii, or Bacillus welchii) is a Gram-positive, rod-shaped, anaerobic, spore-forming bacterium of the genus Clostridium.[1] C. perfringens is everpresent in nature and can be found as a normal component of decaying vegetation, marine sediment, the intestinal tract of humans and other vertebrates, insects, and soil. It has the shortest reported generation time of any organism at 6.3 minutes in thioglycollate medium.[2]
C. perfringens is the third most common cause of food poisoning in the United Kingdom and the United States though it can sometimes be ingested and cause no harm.
Infections due to C. perfringens show evidence of tissue necrosis, bacteremia, emphysematous cholecystitis, and gas gangrene, which is also known as clostridial myonecrosis. The toxin involved in gas gangrene is known as α-toxin, which inserts into the plasma membrane of cells, producing gaps in the membrane that disrupt normal cellular function. C. perfringens can participate in polymicrobial anaerobic infections. Clostridium perfringens is commonly encountered in infections as a component of the normal flora. In this case, its role in disease is minor.
The action of C. perfringens on dead bodies is known to mortuary workers as tissue gas and can be halted only by embalming.
Food poisoning
In the United Kingdom and United States, C. perfringens bacteria are the third most common cause of foodborne illness, with poorly prepared meat and poultry, or food properly prepared but left to stand too long, the main culprits in harboring the bacterium.[3] The clostridium perfringens enterotoxin (CPE) mediating the disease is heat-labile (inactivated at 74 °C (165.2 °F)). It can be detected in contaminated food (if not heated properly), and feces.[4] Incubation time is between six and 24 (commonly 10-12) hours after ingestion of contaminated food.
Since C. perfringens forms spores that can withstand cooking temperatures, if cooked food is let stand for long enough, germination can ensue and infective bacterial colonies develop. Symptoms typically include abdominal cramping, diarrhea; vomiting and fever are usual. The whole course usually resolves within 24 hours. Very rare, fatal cases of clostridial necrotizing enteritis (also known as pigbel) have been known to involve "Type C" strains of the organism, which produce a potently ulcerative β-toxin. This strain is most frequently encountered in Papua New Guinea.
Many cases of C. perfringens food poisoning likely remain subclinical, as antibodies to the toxin are common among the population. This has led to the conclusion that most of the population has experienced food poisoning due to C. perfringens.
Despite its potential dangers, C. perfringens is used as the leavening agent in salt rising bread. The baking process is thought to reduce the bacterial contamination, precluding negative effects.[5]
Infection
Clostridium perfringens is the most common bacterial agent for gas gangrene, which is necrosis, putrefaction of tissues, and gas production. It is caused primarily by Clostridium perfringens alpha toxin. The gases form bubbles in muscle (crepitus) and the characteristic smell in decomposing tissue. After rapid and destructive local spread (which can take only hours), systemic spread of bacteria and bacterial toxins may cause death. This is a problem in major trauma and in military contexts. C. perfringens grows readily on blood agar plate in anaerobic conditions, and often produces a double zone of beta hemolysis.
Research published in 2014 suggested that a strain of C. perfringens might be implicated in multiple sclerosis (MS). Tests in mice found that a toxin made by a rare strain of C. perfringens caused MS-like damage in the brain, and earlier work had identified this strain of C. perfringens in a human with MS.[6] MS patients were found to be ten times more immune-reactive to the epsilon toxin than healthy people.[7]
Diagnosis
C. perfringens can be diagnosed by Nagler's reaction where the suspect organism is cultured on an egg yolk media plate. One side of the plate contains anti-alpha-toxin, while the other side does not. A streak of suspect organism is placed through both sides. An area of turbidity will form around the side that does not have the anti-alpha-toxin, indicating uninhibited lecithinase activity. Other tests/reactions: Catalase: Negative, Spot indole: Positive, Lecithinase: Positive, Lipase: Negative, Litmus Milk: Stormy Fermentation, Reverse CAMP plate: Positive, Gas Liquid Chromatography products: (Acetic, Butyric and Lactic Acids).
Differential diagnosis
Clostridium perfringens infection must be differentiated from other causes of viral, bacterial, and parasitic gastroentritis.
| Organism | Age predilection | Travel History | Incubation Size (cell) | Incubation Time | History and Symptoms | Diarrhea type8 | Food source | Specific consideration | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fever | N/V | Cramping Abd Pain | Small Bowel | Large Bowel | Inflammatory | Non-inflammatory | |||||||||
| Viral | Rotavirus | <2 y | - | <102 | <48 h | + | + | - | + | + | - | Mostly in day cares, most common in winter. | |||
| Norovirus | Any age | - | 10 -103 | 24-48 h | + | + | + | + | + | - | Most common cause of gastroenteritis, abdominal tenderness, | ||||
| Adenovirus | <2 y | - | 105 -106 | 8-10 d | + | + | + | + | + | - | No seasonality | ||||
| Astrovirus | <5 y | - | 72-96 h | + | + | + | + | + | Seafood | Mostly during winter | |||||
| Bacterial | Escherichia coli | ETEC | Any age | + | 108 -1010 | 24 h | - | + | + | + | + | - | Causes travelers diarrhea, contains heat-labile toxins (LT) and heat-stable toxins (ST) | ||
| EPEC | <1 y | - | 10† | 6-12 h | - | + | + | + | + | Raw beef and chicken | - | ||||
| EIEC | Any ages | - | 10† | 24 h | + | + | + | + | + | Hamburger meat and unpasteurized milk | Similar to shigellosis, can cause bloody diarrhea | ||||
| EHEC | Any ages | - | 10 | 3-4 d | - | + | + | + | + | Undercooked or raw hamburger (ground beef) | Known as E. coli O157:H7, can cause HUS/TTP. | ||||
| EAEC | Any ages | + | 1010 | 8-18 h | - | - | + | + | + | - | May cause prolonged or persistent diarrhea in children | ||||
| Salmonella sp. | Any ages | + | 1 | 6 to 72 h | + | + | + | + | + | Meats, poultry, eggs, milk and dairy products, fish, shrimp, spices, yeast, coconut, sauces, freshly prepared salad. | Can cause salmonellosis or typhoid fever. | ||||
| Shigella sp. | Any ages | - | 10 - 200 | 8-48 h | + | + | + | + | + | Raw foods, for example, lettuce, salads (potato, tuna, shrimp, macaroni, and chicken) | Some strains produce enterotoxin and Shiga toxin similar to those produced by E. coli O157:H7 | ||||
| Campylobacter sp. | <5 y, 15-29 y | - | 104 | 2-5 d | + | + | + | + | + | Undercooked poultry products, unpasteurized milk and cheeses made from unpasteurized milk, vegetables, seafood and contaminated water. | May cause bacteremia, Guillain-Barré syndrome (GBS), hemolytic uremic syndrome (HUS) and recurrent colitis | ||||
| Yersinia enterocolitica | <10 y | - | 104 -106 | 1-11 d | + | + | + | + | + | Meats (pork, beef, lamb, etc.), oysters, fish, crabs, and raw milk. | May cause reactive arthritis; glomerulonephritis; endocarditis; erythema nodosum.
can mimic appendicitis and mesenteric lymphadenitis. | ||||
| Clostridium perfringens | Any ages | > 106 | 16 h | - | - | + | + | + | Meats (especially beef and poultry), meat-containing products (e.g., gravies and stews), and Mexican foods. | Can survive high heat, | |||||
| Vibrio cholerae | Any ages | - | 106-1010 | 24-48 h | - | + | + | + | + | Seafoods, including molluscan shellfish (oysters, mussels, and clams), crab, lobster, shrimp, squid, and finfish. | Hypotension, tachycardia, decreased skin turgor. Rice-water stools | ||||
| Parasites | Protozoa | Giardia lamblia | 2-5 y | + | 1 cyst | 1-2 we | - | - | + | + | + | Contaminated water | May cause malabsorption syndrome and severe weight loss | ||
| Entamoeba histolytica | 4-11 y | + | <10 cysts | 2-4 we | - | + | + | + | + | Contaminated water and raw foods | May cause intestinal amebiasis and amebic liver abscess | ||||
| Cryptosporidium parvum | Any ages | - | 10-100 oocysts | 7-10 d | + | + | + | + | + | Juices and milk | May cause copious diarrhea and dehydration in patients with AIDS especially with 180 > CD4 | ||||
| Cyclospora cayetanensis | Any ages | + | 10-100 oocysts | 7-10 d | - | + | + | + | + | Fresh produce, such as raspberries, basil, and several varieties of lettuce. | More common in rainy areas | ||||
| Helminths | Trichinella spp | Any ages | - | Two viable larvae (male and female) | 1-4 we | - | + | + | + | + | Undercooked meats | More common in hunters or people who eat traditionally uncooked meats | |||
| Taenia spp | Any ages | - | 1 larva or egg | 2-4 m | - | + | + | + | + | Undercooked beef and pork | Neurocysticercosis: Cysts located in the brain may be asymptomatic or seizures, increased intracranial pressure, headache. | ||||
| Diphyllobothrium latum | Any ages | - | 1 larva | 15 d | - | - | - | + | + | Raw or undercooked fish. | May cause vitamin B12 deficiency | ||||
8Small bowel diarrhea: watery, voluminous with less than 5 WBC/high power field
Large bowel diarrhea: Mucousy and/or bloody with less volume and more than 10 WBC/high power field
† It could be as high as 1000 based on patient's immunity system.
The table below summarizes the findings that differentiate inflammatory causes of chronic diarrhea[8][9][10][11][11]
| Cause | History | Laboratory findings | Diagnosis | Treatment |
|---|---|---|---|---|
| Diverticulitis |
|
|
Abdominal CT scan with oral and intravenous (IV) contrast | bowel rest, IV fluid resuscitation, and broad-spectrum antimicrobial therapy which covers anaerobic bacteria and gram-negative rods |
| Ulcerative colitis |
|
|
Endoscopy | Induction of remission with mesalamine and corticosteroids followed by the administration of sulfasalazine and 6-Mercaptopurine depending on the severity of the disease. |
| Entamoeba histolytica |
|
cysts shed with the stool | detects ameba DNA in feces | Amebic dysentery
Luminal amebicides for E. histolytica in the colon:
For amebic liver abscess:
|
Food poisoning incidents
On May 7, 2010, 42 residents and 12 staff members at a Louisiana state psychiatric hospital experienced vomiting, abdominal cramps, and diarrhea. Within 24 hours, three patients had died. The outbreak was linked to chicken which was cooked a day prior to being served and was not cooled down according to hospital guidelines. The outbreak affected 31% of the residents of the hospital and 69% of the staff who ate the chicken. It is unknown how many of the affected residents ate the chicken.[12]
In May 2011, a man died after allegedly eating food contaminated with the bacteria on a transatlantic American Airlines flight. The man's wife and daughter are suing American and LSG Sky Chefs, the German company that prepared the inflight food.[13]
In December 2012, a 46-year-old woman died two days after eating a Christmas Day meal at a pub in Hornchurch, Essex, England. She was among about 30 people to fall ill after eating the meal. Samples taken from the victims contained C.perfringens. The hotel manager and the cook were jailed for offences arising from the incident.[14]
In December 2014, 87 year old Bessie Scott died three days after eating a church potluck supper in Nackawic, New Brunswick, Canada. Over 30 other people reported signs of gastrointestinal illness, diarrhea and abdominal pain. The province's acting chief medical officer says Clostridium perfringens is the bacteria that most likely caused the woman’s death.[15]
References
- ↑ Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. ISBN 0-8385-8529-9.[page needed]
- ↑ http://bionumbers.hms.harvard.edu//bionumber.aspx?id=105474&ver=1
- ↑ Warrell; et al. (2003). Oxford Textbook of Medicine (4th ed.). Oxford University Press. ISBN 0-19-262922-0.[page needed]
- ↑ Murray; et al. (2009). Medical Microbiology (6th ed.). Mosby Elsevier. ISBN 978-0-323-05470-6.[page needed]
- ↑ Juckett, Gregory; et al. (November 2008). "The Microbiology of Salt Rising Bread" (PDF). West Virginia Medical Journal (22). Retrieved 22 July 2015.
- ↑ "Multiple sclerosis 'linked to food bug'". BBC. 29 January 2014. Retrieved 29 January 2014.
- ↑ http://www.foxnews.com/health/2014/01/29/bacterial-toxin-may-trigger-multiple-sclerosis-research-finds/?intcmp=trending
- ↑ Konvolinka CW (1994). "Acute diverticulitis under age forty". Am J Surg. 167 (6): 562–5. PMID 8209928.
- ↑ Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR; et al. (2005). "Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology". Can J Gastroenterol. 19 Suppl A: 5A–36A. PMID 16151544.
- ↑ Satsangi J, Silverberg MS, Vermeire S, Colombel JF (2006). "The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications". Gut. 55 (6): 749–53. doi:10.1136/gut.2005.082909. PMC 1856208. PMID 16698746.
- ↑ 11.0 11.1 Haque R, Huston CD, Hughes M, Houpt E, Petri WA (2003). "Amebiasis". N Engl J Med. 348 (16): 1565–73. doi:10.1056/NEJMra022710. PMID 12700377.
- ↑ "Fatal Foodborne Clostridium perfringens Illness at a State Psychiatric Hospital — Louisiana, 2010". Centers for Disease Control and Prevention. Retrieved 16 November 2013.
- ↑ Mohn, Tanya. "Overhead Bin - Passenger dies in-flight, family says airline to blame". Overheadbin.msnbc.msn.com. Retrieved 2012-02-13.
- ↑ "Pub chef and manager jailed over Christmas dinner that left a diner dead". The Guardian. 23 January 2015. Retrieved 3 August 2015.
- ↑ "Woman's death likely caused by bacteria from Christmas supper". CBC. 12 December 2014.
External links
- Clostridium perfringens genomes and related information at PATRIC, a Bioinformatics Resource Center funded by NIAID
- Pathema-Clostridium Resource
Template:Gram-positive firmicutes diseases
Lua error in Module:Authority_control at line 788: attempt to index field 'wikibase' (a nil value).
- CS1 maint: Extra text: authors list
- Wikipedia articles needing page number citations from April 2011
- Articles with invalid date parameter in template
- CS1 maint: Explicit use of et al.
- CS1 maint: Multiple names: authors list
- Pages with script errors
- Clostridiaceae
- Gas gangrene
- Gram-positive bacteria
- Bacteria with sequenced genomes