COVID-19-associated diabetes mellitus
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Tayyaba Ali, M.D.[2]
Synonyms and keywords: New-onset Diabetes in COVID-19 Islet cell injury by SARS-CoV 2
To browse the complete page of COVID-19, Click here.
Overview
ACE2 receptors in the endocrine pancreas serve the entrance for Severe acute respiratory syndrome coronavirus 2 (SARS-CoV 2), which causes Corononavirus Disease 2019 (COVID-19). Researchers in China observed new-onset diabetes among SARS-CoV patients. Therefore in agreement with this, the SARS-CoV-2 might enter pancreatic islets through binding to ACE2, and cause acute β-cell injury, leading to intense hyperglycemia and transient Type 2 Diabetes Mellitus. SARS-CoV 2 can cause hyperglycemia by direct injuring of pancreatic beta cells and by downregulating ACE2 receptors leading to unopposed angiotensin II, which may hinder insulin secretion
Historical Perspective
- Diabetes mellitus is defined by insulin deficiency due to either diminished insulin release or end-organ insulin resistance.[1]
- Diabetes is an umbrella term for conditions such as type I (T1DM) and type II (T2DM) diabetes mellitus, gestational diabetes, and maturity-onset diabetes of the young (MODY).[1]
- Type 1 Diabetes Mellitus is caused by pancreatic β-cell failure or auto-immune destruction of the pancreatic β-cells. It generally presents in children and young adults.[1]
- Type 2 Diabetes Mellitus (T2DM) is defined by insulin resistance and presents in adults. Family history, hypertension, obesity, and dyslipidemia play a significant role in causing T2DM.[1]
- Around 422 million individuals worldwide have diabetes, the dominant part living in low-and middle-income nations, and 1.6 million deaths are straightforwardly credited to diabetes every year. In the course of recent decades, a consistent rise has been observed in both the incidence and the prevalence.[2]
- In China, in the year 2008, a study was done in which they compared 39 SARS-CoV patients with no previous history of diabetes, who never used steroids, with 39 matched healthy siblings.The results of the study revealed that 20 out of 39 SARS-CoV patients developed new-onset diabetes during the hospital stay. After 3 years of recovery from the SARS-CoV infection, only 5% of patients remained diabetic whereas blood sugar levels normalized in the rest of the patients with the infection recovery.[3]
- ACE2 is the primary receptor For SARS-CoV spike protein. SARS-CoV causes infection by binding to ACE2 receptors on the target cells.[4][5] The study suggested, SARS-CoV may damage islets and cause acute insulin dependent diabetes mellitus.[3]
- In mid-April 2020, Finn Gnadt, an 18-year-old student from Kiel, Germany, learnt that he had been infected with the SARS-CoV-2 coronavirus.
- Gnadt thought he had endured the infection unscathed, but days later, he started to feel worn out and exceedingly thirsty. In early May, he was diagnosed with type 1 diabetes, and his physician, Tim Hollstein at the University Hospital Schleswig-Holstein in Kiel, suggested that the sudden onset might be linked to the viral infection.
- Hollstein suspected that the virus had destroyed his β-cells because his blood didn’t contain the types of immune cells that typically damage the pancreatic islets where the β-cells live.[6]
- To browse the historical perspective of COVID-19, Click here.
Classification
- There is no established system for the classification of COVID-19-associated Diabetes.
- Future research is needed to provide a better understanding of the type of Diabetes, SARS-CoV-2 can cause. Whether SARS-CoV causes T1DM or T2DM or a new type of Diabetes.
- To browse the classification of COVID-19, Click here.
Pathophysiology
- Angiotensin-converting enzyme 2 (ACE2) receptors expressed in the tissues that are highly involved in body metabolism. These tissues comprise of pancreatic beta cells, adipose tissue, small intestine, and the kidneys. ACE2 receptors in the endocrine pancreas serve the entrance for Severe acute respiratory syndrome coronavirus 2 (SARS-CoV 2), which causes Corononavirus Disease 2019 (COVID-19). [7]
- Expression of ACE2 receptors and effector protease TMPRSS2 in pancreas are associated with SARS-CoV 2 infection.[8]
- The pancreas consists of nine different cell types such as acinar cells, ductal cells, beta cells, alpha cells, mesenchymal cells, and endothelial cells. These pancreatic cells express both ACE2 and TMPRSS2. The expression of ACE2 in pancreatic alpha and beta cells is further proved by immunohistochemistry. Both beta cells that secrete insulin and alpha cells that secrete glucagon, stained positive for SARS-CoV 2 Spike protein and thus, it is postulated that SARS-CoV-2 can infect pancreatic islet cells.[8]
- A recent experiement was conducted to study SARS-CoV-2 tropism that is the cellular response to an external stimulus in human cells and organoids. Researchers infect human pluripotent stem cells (hPSC)-derived pancreatic endocrine cells with SARS-CoV-2.[9]
- Researchers found when SARS-CoV-2 infect pancreatic cells, it downregulates the pathways including calcium signaling pathways, glucagon signaling pathways of alpha cells, and metabolic pathways that assist in insulin secretion from pancreatic beta cells.[9]
- Researchers further stained SARS-CoV-2 infected hPSC-derived pancreatic endocrine cells with a cell apoptotic marker (CASP3). As a result of this staining, they found a large number of CASP3 cells in infected hPSC-derived pancreatic cells. This indicates that change in metabolic pathways of the pancreas is mainly due to cell apoptosis, trigger by SARS-CoV-2. This experiment suggest that when SARS-CoV-2 binds to ACE2 in pancreas, this will upregulate the genes responsible for apoptosis and downregulate the genes responsible for the cell survival. [9]
- ACE2 is the target receptor for both SARS-CoV and SARS-CoV-2. Researchers in China observed new-onset diabetes among SARS-CoV patients. Therefore in agreement with this, the SARS-CoV-2 might enter pancreatic islets through binding to ACE2, and cause acute β-cell injury, leading to intense hyperglycemia and transient Type 2 Diabetes Mellitus.[3]
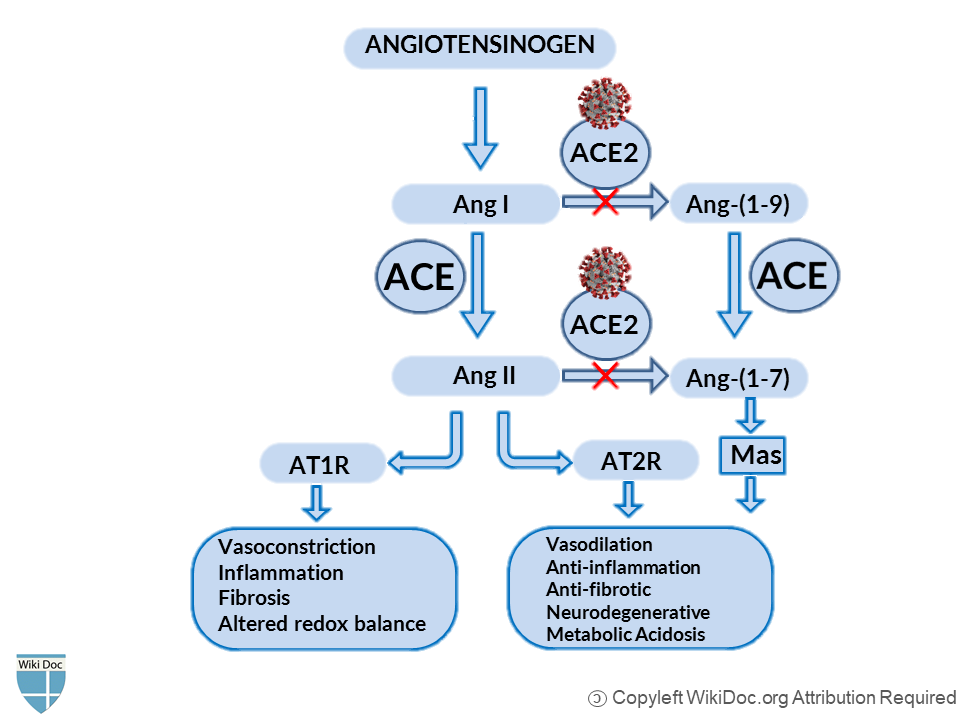
- ACE2 serves as the negative regulator of the Renin-Angiotensin System (RAS) mainly by converting Ang (angiotensin) I and Ang II into Ang 1-9 and Ang 1-7, respectively.[10][11] When SARS-CoV and SARS-CoV-2 bind to ACE2 receptors, this will lead to the subsequent downregulation of surface ACE2 expression.[5][12][13] SARS-CoV-2 differs from SARS-CoV by 380 amino acid substitutions and thus has a stronger binding affinity than SARS-CoV, which explains the global impact of SARS-CoV-2 than the previous SARS-CoV outbreak.[14][15]
- ACE2 is the negative regulator of the Renin-Angiotensin system (RAS) and has protective benefits against many diseases and complications. SARS-CoV-2 binds to ACE2 receptors, this blocks all the protective benefits of the ACE2 pathway and shifts the cascade back to ACE/Ang II/AT1R-pathway, increasing Ang II, decreasing ACE2 and Ang-( 1-7)[16][17] as shown in the figure.
- Inhibition of RAS(Angiotensin→Ang1→Ang2→AT1R) protects pancreatic β-cells from oxidative stress-related tissue damage, therefore improves insulin synthesis and secretion.[18]Hyperactivity of RAS works in contrast. In adipose tissue, Ras decreases insulin sensitivity, decreases glucose uptake. In pancreatic tissue, it decreases insulin secretion, increases islet oxidative stress and fibrosis, decrease perfusion.[19]
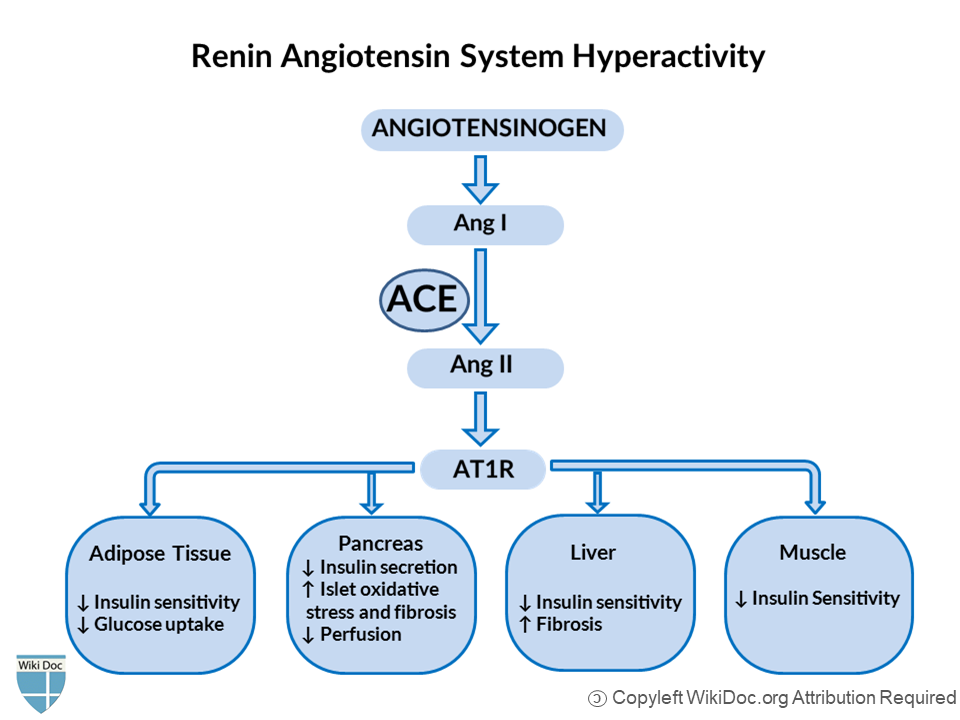
- In an experimental trial, pressor doses of Ang-II were given to healthy human subjects. As a result, researchers observed suppression of basal, pulsatile, and glucose-stimulated insulin release.[20]This loss of insulin release is supposed to be the contributing factor in the development of T2DM.[21]
- SARS-CoV 2 can cause hyperglycemia by direct injuring of pancreatic beta cells[3] and by downregulating ACE2 receptors leading to unopposed angiotensin II, which may hinder insulin secretion.[22]
- To browse the pathophysiology of COVID-19, Click here.
Causes
- SARS-CoV-2 can cause COVID-19-associated diabetes mellitus by two mechanisms:
- Direst damage of pancreatic beta-cells by SARS-CoV 2 [3]
- Downregulation of ACE2 by SARS-CoV 2 shift the cascade to the ACE/AngII/AT1R pathway which further leads to decrease insulin release and islet cell oxidative damage.[22]
- To browse the causes of COVID-19, Click here.
Differentiating COVID-19-associated diabetes mellitus from other Diseases
- For more information on COVID-19-associated diabetes mellitus differential diagnosis click here.
- To browse the differential diagnosis of COVID-19, Click here.
Epidemiology and Demographics
- There is not enough data available on incidence and prevalence of COVID-19-associated Diabetes Mellitus.
- To browse the epidemiology and Demographics of Diabetes Mellitus. Click here.
- To browse the epidemiology and demographics of COVID-19, Click here.
Risk Factors
- There are no established risk factors for COVID-19-associated Diabetes.
- To browse the risk factors for different types of Diabetes Mellitus, Click here.
- To browse the risk factors of COVID-19 clicking here.
Screening
- There is insufficient evidence to recommend routine screening for COVID-19-associated Diabetes.
- To browse the screening performed for Diabetes Mellitus, Click here.
- To browse the screening performed for COVID-19, Click here.
Natural History, Complications, and Prognosis
Natural History
- A high blood sugar level can cause several symptoms, including:[23]
Complications
- After many years, diabetes can lead to serious health problems:[23]
- Blindness
- Infection:As a result of high blood sugar, feet and skin can develop sores and infections.
- High blood pressure and cholesterol: Diabetes may make it harder to control blood pressure and cholesterol. This can lead to a heart attack, stroke, and other problems. It can become harder for blood to flow to legs and feet.
- Neuropathy: High blood sugar can damage the nerves, causing pain, tingling, and numbness.
- Nephropathy: High blood sugar and other problems can lead to kidney damage. Kidneys may not work as well as they used to. They may even stop working so that one needs dialysis or a kidney transplant.
- Immune Dysfunction: Immune system can weaken, which can lead to frequent infections.[23]
Prognosis
- There is not enough data available on the prognosis of SARS-CoV-2 induced Diabetes Mellitus. Based on the data of SARS-CoV induced diabetes, the overall prognosis is good.
- In China, in the year 2008, a study was done in which they compared 39 SARS-CoV patients with no previous history of diabetes, who never used steroids, with 39 matched healthy siblings. The results of the study revealed that 20 out of 39 SARS-CoV patients developed new-onset diabetes during the hospital stay. After 3 years of recovery from the SARS-CoV infection, only 5% of patients remained diabetic whereas blood sugar levels normalized in the rest of the patients with the infection recovery.[3]
- To browse the natural history, complications, and prognosis of COVID-19, Click here.
Diagnosis
Diagnostic Study of Choice
- Diagnostic study of choice for diabetes mellitus is fasting plasma glucose (FPG). According to the American Diabetes Association (ADA) criteria, diabetes mellitus is diagnosed with FPG ≥126 mg/dL (7.0 mmol/L). [24][25][26]
- To browse the diagnostic study of choice of COVID-19, Click here.
History and Symptoms
- According to a recent case report of Diabetic ketoacidoses precipitated by COVID-19 in a patient with newly diagnosed diabetes mellitus. He was a previously healthy man presented with 1-week history of:
- Fever (38.5 °C)
- Vomiting,
- Polydipsia (intense thirst)
- Polyuria (production of abnormally large volumes of dilute urine)[27]
- To browse the history and symptoms of COVID-19, Click here.
Physical Examination
- Mildly tachycardic
- Kusmmaul's breathing was not observed.[27]
- To browse the physical examination of COVID-19, Click here.
Laboratory Findings
| Investigation | Result | Reference Range |
|---|---|---|
| Venous glucose (mmol/L) | 39.7 | – |
| Arterial blood gas | ||
| pH (mmHg) | 7.28 | 7.25–7.35 |
| Bicarbonate (mmol/L) | 12 | 22–28 |
| pCO2 (mmHg) | 25 | 35–45 |
| Sodium (mmol/L) | 128 | 135–145 |
| Chloride (mmol/L) | 86 | 95–110 |
| Anion gap | 30 | 8–16 |
| Ketones (mmol/L) | 6.4 | <0.6 |
| Creatinine (umol/L) | 95 | 67–112 |
| Glycated hemoglobin (%) | 14.2 | – |
- COVID-19 infection can cause ketosis and ketoacidosis.[29]When the body doesn’t make enough insulin to break down sugar, it uses ketones as an alternative source of fuel.[30]
- To browse the laboratory findings of COVID-19, Click here.
- To browse the diagnosis of Diabetes mellitus, Click here.
Electrocardiogram
- There are no electrocardiographic findings of COVID-19 associated Diabetes Mellitus.
- To browse the electrocardiogram findings of COVID-19, click here.
X-ray
- There are no X-ray findings of COVID-19-associated diabetes mellitus.
- To view the x-ray finidings of COVID-19, click here.
Echocardiography or Ultrasound
- There are no echocardiography/ultrasound findings associated with COVID-19-associated diabetes mellitus.
- To browse the echocardiography findings of COVID-19, Click here.
CT Scan
- There are no CT scan findings associated with COVID-19-associated diabetes mellitus.
- To browse the CT Scan findings of COVID-19, Click here.
MRI
- There are no MRI findings associated with COVID-19-associated diabetes mellitus.
- To browse the MRI findings of COVID-19, Click here.
Other Diagnostic Studies
- Fasting plasma glucose (FPG) test
- HbA1C or A1C test
- Random plasma glucose (RPG) test[31]
Treatment
Medical Therapy
- A 37-year-old, previously healthy man diagnosed with COVID-19-associated diabetes mellitus. The patient received 6 L of intravenous fluids and intravenous insulin infusion in the first 24 h. Serum electrolytes were closely monitored. Diabetic ketoacidosis resolved the following day and he was transitioned to subcutaneous insulin therapy.[28]
- To browse the treatment of Diabetes Mellitus, Click here.
Primary Prevention
- Keeping an ideal body weight and an active lifestyle may prevent or delay the start of diabetes. If overweight, losing just 5% of body weight can reduce the risk.[23]
- There have been rigorous efforts in order to develop a vaccine for novel coronavirus and several vaccines are in the later phases of trials.[32]
- The best way to prevent infection is to avoid being exposed to this virus. CDC recommends following practices that should be adopted for infection control:[33]
- Hand washing often with soap and water for at least 20 seconds.
- Using an alcohol-based hand sanitizer that contains at least 60% alcohol if soap and water are not available.
- Staying at least 6 feet (about 2 arms’ length) from other people who do not live with you.
- Covering your mouth and nose with a cloth face cover when around others and covering sneezes and coughs.
- Cleaning and disinfecting.
Secondary Prevention
- Getting better control over your blood sugar, cholesterol, and blood pressure levels help reduce the risk for kidney disease, eye disease, nervous system disease, heart attack, and stroke.[23]
- WHO recommends home care for patients with suspected COVID-19 who present with mild symptoms.[34]
- It is highly recommended for people with suspected or affirmed COVID-19 (including those anticipating test results) should remain at home and attempt to isolate themselves from other members and animals in the family unit.[35][36]
- World Health Organization (WHO) has recommended wearing a medical mask if family members are in the same room with the COVID-19 patient to prevent the spread of the virus.[37] Whereas, according to the United States Centers for Disease Control and Prevention (CDC), a cloth face Cover can be acceptable for caregivers at home and has considered the use of a medical mask for healthcare workers.[38]
- It is highly recommended for COVID-19 patients to use a separate bedroom and bathroom to prevent the spread of infection to family members. To avoid sharing rooms and if sharing space in a home is unavoidable, keeping a six feet (two meters) distance is extremely emphasized. Care providers should perform hand hygiene after any form of contact with patients or their immediate environment. In a process of providing care to the patient, the caregiver should wear gloves while touching the patient's blood, stool, or body fluids, such as saliva, sputum, nasal mucus, vomit, and urine. Certain things should not be shared with COVID-19 patients such as dishes, drinking glasses, cups, eating utensils, towels, bedding, and thermometers. After the COVID-19 patients use these things, they should be properly disinfected.[39][40][41][42]
- To browse the secondary prevention of COVID-19, Click here.
References
- ↑ 1.0 1.1 1.2 1.3 King, H.; Aubert, R. E.; Herman, W. H. (1998). "Global Burden of Diabetes, 1995-2025: Prevalence, numerical estimates, and projections". Diabetes Care. 21 (9): 1414–1431. doi:10.2337/diacare.21.9.1414. ISSN 0149-5992.
- ↑ "Diabetes".
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Yang, Jin-Kui; Lin, Shan-Shan; Ji, Xiu-Juan; Guo, Li-Min (2009). "Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes". Acta Diabetologica. 47 (3): 193–199. doi:10.1007/s00592-009-0109-4. ISSN 0940-5429.
- ↑ Turner, Anthony J; Hiscox, Julian A; Hooper, Nigel M (2004). "ACE2: from vasopeptidase to SARS virus receptor". Trends in Pharmacological Sciences. 25 (6): 291–294. doi:10.1016/j.tips.2004.04.001. ISSN 0165-6147.
- ↑ 5.0 5.1 Li, Wenhui; Moore, Michael J.; Vasilieva, Natalya; Sui, Jianhua; Wong, Swee Kee; Berne, Michael A.; Somasundaran, Mohan; Sullivan, John L.; Luzuriaga, Katherine; Greenough, Thomas C.; Choe, Hyeryun; Farzan, Michael (2003). "Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus". Nature. 426 (6965): 450–454. doi:10.1038/nature02145. ISSN 0028-0836.
- ↑ Bornstein, Stefan R.; Dalan, Rinkoo; Hopkins, David; Mingrone, Geltrude; Boehm, Bernhard O. (2020). "Endocrine and metabolic link to coronavirus infection". Nature Reviews Endocrinology. 16 (6): 297–298. doi:10.1038/s41574-020-0353-9. ISSN 1759-5029.
- ↑ 8.0 8.1 Hoffmann, Markus; Kleine-Weber, Hannah; Schroeder, Simon; Krüger, Nadine; Herrler, Tanja; Erichsen, Sandra; Schiergens, Tobias S.; Herrler, Georg; Wu, Nai-Huei; Nitsche, Andreas; Müller, Marcel A.; Drosten, Christian; Pöhlmann, Stefan (2020). "SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor". Cell. 181 (2): 271–280.e8. doi:10.1016/j.cell.2020.02.052. ISSN 0092-8674.
- ↑ 9.0 9.1 9.2 Yang, Liuliu; Han, Yuling; Nilsson-Payant, Benjamin E.; Gupta, Vikas; Wang, Pengfei; Duan, Xiaohua; Tang, Xuming; Zhu, Jiajun; Zhao, Zeping; Jaffré, Fabrice; Zhang, Tuo; Kim, Tae Wan; Harschnitz, Oliver; Redmond, David; Houghton, Sean; Liu, Chengyang; Naji, Ali; Ciceri, Gabriele; Guttikonda, Sudha; Bram, Yaron; Nguyen, Duc-Huy T.; Cioffi, Michele; Chandar, Vasuretha; Hoagland, Daisy A.; Huang, Yaoxing; Xiang, Jenny; Wang, Hui; Lyden, David; Borczuk, Alain; Chen, Huanhuan Joyce; Studer, Lorenz; Pan, Fong Cheng; Ho, David D.; tenOever, Benjamin R.; Evans, Todd; Schwartz, Robert E.; Chen, Shuibing (2020). "A Human Pluripotent Stem Cell-based Platform to Study SARS-CoV-2 Tropism and Model Virus Infection in Human Cells and Organoids". Cell Stem Cell. doi:10.1016/j.stem.2020.06.015. ISSN 1934-5909.
- ↑ Patel, Vaibhav B.; Zhong, Jiu-Chang; Grant, Maria B.; Oudit, Gavin Y. (2016). "Role of the ACE2/Angiotensin 1–7 Axis of the Renin–Angiotensin System in Heart Failure". Circulation Research. 118 (8): 1313–1326. doi:10.1161/CIRCRESAHA.116.307708. ISSN 0009-7330.
- ↑ Wang, Kaiming; Gheblawi, Mahmoud; Oudit, Gavin Y. (2020). "Angiotensin Converting Enzyme 2: A Double-Edged Sword". Circulation. doi:10.1161/CIRCULATIONAHA.120.047049. ISSN 0009-7322.
- ↑ Walls, Alexandra C.; Park, Young-Jun; Tortorici, M. Alejandra; Wall, Abigail; McGuire, Andrew T.; Veesler, David (2020). "Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein". Cell. 181 (2): 281–292.e6. doi:10.1016/j.cell.2020.02.058. ISSN 0092-8674.
- ↑ Zhou, Peng; Yang, Xing-Lou; Wang, Xian-Guang; Hu, Ben; Zhang, Lei; Zhang, Wei; Si, Hao-Rui; Zhu, Yan; Li, Bei; Huang, Chao-Lin; Chen, Hui-Dong; Chen, Jing; Luo, Yun; Guo, Hua; Jiang, Ren-Di; Liu, Mei-Qin; Chen, Ying; Shen, Xu-Rui; Wang, Xi; Zheng, Xiao-Shuang; Zhao, Kai; Chen, Quan-Jiao; Deng, Fei; Liu, Lin-Lin; Yan, Bing; Zhan, Fa-Xian; Wang, Yan-Yi; Xiao, Geng-Fu; Shi, Zheng-Li (2020). "A pneumonia outbreak associated with a new coronavirus of probable bat origin". Nature. 579 (7798): 270–273. doi:10.1038/s41586-020-2012-7. ISSN 0028-0836.
- ↑ Yan, Renhong; Zhang, Yuanyuan; Li, Yaning; Xia, Lu; Guo, Yingying; Zhou, Qiang (2020). "Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2". Science. 367 (6485): 1444–1448. doi:10.1126/science.abb2762. ISSN 0036-8075.
- ↑ Shang, Jian; Ye, Gang; Shi, Ke; Wan, Yushun; Luo, Chuming; Aihara, Hideki; Geng, Qibin; Auerbach, Ashley; Li, Fang (2020). "Structural basis of receptor recognition by SARS-CoV-2". Nature. 581 (7807): 221–224. doi:10.1038/s41586-020-2179-y. ISSN 0028-0836.
- ↑ Gheblawi, Mahmoud; Wang, Kaiming; Viveiros, Anissa; Nguyen, Quynh; Zhong, Jiu-Chang; Turner, Anthony J.; Raizada, Mohan K.; Grant, Maria B.; Oudit, Gavin Y. (2020). "Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System". Circulation Research. 126 (10): 1456–1474. doi:10.1161/CIRCRESAHA.120.317015. ISSN 0009-7330.
- ↑ D’Ardes, Damiano; Boccatonda, Andrea; Rossi, Ilaria; Guagnano, Maria Teresa; Santilli, Francesca; Cipollone, Francesco; Bucci, Marco (2020). "COVID-19 and RAS: Unravelling an Unclear Relationship". International Journal of Molecular Sciences. 21 (8): 3003. doi:10.3390/ijms21083003. ISSN 1422-0067.
- ↑ Grankvist, K; Marklund, S L; Täljedal, I B (1981). "CuZn-superoxide dismutase, Mn-superoxide dismutase, catalase and glutathione peroxidase in pancreatic islets and other tissues in the mouse". Biochemical Journal. 199 (2): 393–398. doi:10.1042/bj1990393. ISSN 0264-6021.
- ↑ Bindom, Sharell M.; Lazartigues, Eric (2009). "The sweeter side of ACE2: Physiological evidence for a role in diabetes". Molecular and Cellular Endocrinology. 302 (2): 193–202. doi:10.1016/j.mce.2008.09.020. ISSN 0303-7207.
- ↑ Fliser, Danilo; Schaefer, Franz; Schmid, Daniela; Veldhuis, Johannes D.; Ritz, Eberhard (1997). "Angiotensin II Affects Basal, Pulsatile, and Glucose-Stimulated Insulin Secretion in Humans". Hypertension. 30 (5): 1156–1161. doi:10.1161/01.HYP.30.5.1156. ISSN 0194-911X.
- ↑ Gerich, J. E. (2002). "Is Reduced First-Phase Insulin Release the Earliest Detectable Abnormality in Individuals Destined to Develop Type 2 Diabetes?". Diabetes. 51 (Supplement 1): S117–S121. doi:10.2337/diabetes.51.2007.S117. ISSN 0012-1797.
- ↑ 22.0 22.1 Carlsson, P.-O.; Berne, C.; Jansson, L. (1998). "Angiotensin II and the endocrine pancreas: effects on islet blood flow and insulin secretion in rats". Diabetologia. 41 (2): 127–133. doi:10.1007/s001250050880. ISSN 0012-186X.
- ↑ 23.0 23.1 23.2 23.3 23.4 "Diabetes: MedlinePlus Medical Encyclopedia".
- ↑ Nguyen Q, Nguyen L, Felicetta J (October 2008). "Evaluation and management of diabetes mellitus". Am Health Drug Benefits. 1 (8): 39–48. PMC 4106505. PMID 25126259.
- ↑ "Standards of medical care in diabetes--2008". Diabetes Care. 31 Suppl 1: S12–54. January 2008. doi:10.2337/dc08-S012. PMID 18165335.
- ↑ "2. Classification and Diagnosis of Diabetes:Standards of Medical Care in Diabetes—2018". Diabetes Care. 41 (Supplement 1): S13–S27. 2017. doi:10.2337/dc18-S002. ISSN 0149-5992.
- ↑ 27.0 27.1 Chee, Ying Jie; Ng, Shereen Jia Huey; Yeoh, Ester (2020). "Diabetic ketoacidosis precipitated by Covid-19 in a patient with newly diagnosed diabetes mellitus". Diabetes Research and Clinical Practice. 164: 108166. doi:10.1016/j.diabres.2020.108166. ISSN 0168-8227.
- ↑ 28.0 28.1 Chee YJ, Ng SJH, Yeoh E (2020). "Diabetic ketoacidosis precipitated by Covid-19 in a patient with newly diagnosed diabetes mellitus". Diabetes Res Clin Pract. 164: 108166. doi:10.1016/j.diabres.2020.108166. PMC 7194589 Check
|pmc=value (help). PMID 32339533 Check|pmid=value (help). - ↑ Li, Juyi; Wang, Xiufang; Chen, Jian; Zuo, Xiuran; Zhang, Hongmei; Deng, Aiping (2020). "COVID
‐19 infection may cause ketosis and ketoacidosis". Diabetes, Obesity and Metabolism. doi:10.1111/dom.14057. ISSN 1462-8902. line feed character in
|title=at position 6 (help) - ↑ "Mounting clues suggest the coronavirus might trigger diabetes".
- ↑ "Diabetes Tests & Diagnosis | NIDDK".
- ↑ "NIH clinical trial of investigational vaccine for COVID-19 begins | National Institutes of Health (NIH)".
- ↑ https://www.cdc.gov/coronavirus/2019-ncov/index.html. Missing or empty
|title=(help) - ↑ "Home care for patients with COVID-19 presenting with mild symptoms and management of their contacts".
- ↑ "COVID-19 and Animals | CDC". Retrieved 7/11/2020. Check date values in:
|accessdate=(help) - ↑ [+http://dx.doi.org/10.15585/mmwr.mm6923e3 "First Reported Cases of SARS-CoV-2 Infection in Companion Animals — New York, March–April 2020 | MMWR"] Check
|url=value (help). Retrieved 7/11/2020. Check date values in:|accessdate=(help) - ↑ [+https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak "Advice on the use of masks in the community, during home care and in healthcare settings in the context of the novel coronavirus (COVID-19) outbreak"] Check
|url=value (help). Retrieved 7/11/2020. Check date values in:|accessdate=(help) - ↑ "www.cdc.gov". Retrieved 7/11/2020. Check date values in:
|accessdate=(help) - ↑ "Home care for patients with COVID-19 presenting with mild symptoms and management of their contacts". Retrieved 7/11/2020. Check date values in:
|accessdate=(help) - ↑ "COVID19 - Caring for someone at home | CDC". Retrieved 7/12/2020. Check date values in:
|accessdate=(help) - ↑ "Cleaning and Disinfection for Households | CDC". Retrieved 7/12/2020. Check date values in:
|accessdate=(help) - ↑ "Advice on the use of masks in the community, during home care and in healthcare settings in the context of the novel coronavirus (COVID-19) outbreak". Retrieved 7/12/2020. Check date values in:
|accessdate=(help)