Atrial flutter resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Hilda Mahmoudi M.D., M.P.H.[2]; Priyamvada Singh, M.D. [3]
Definition
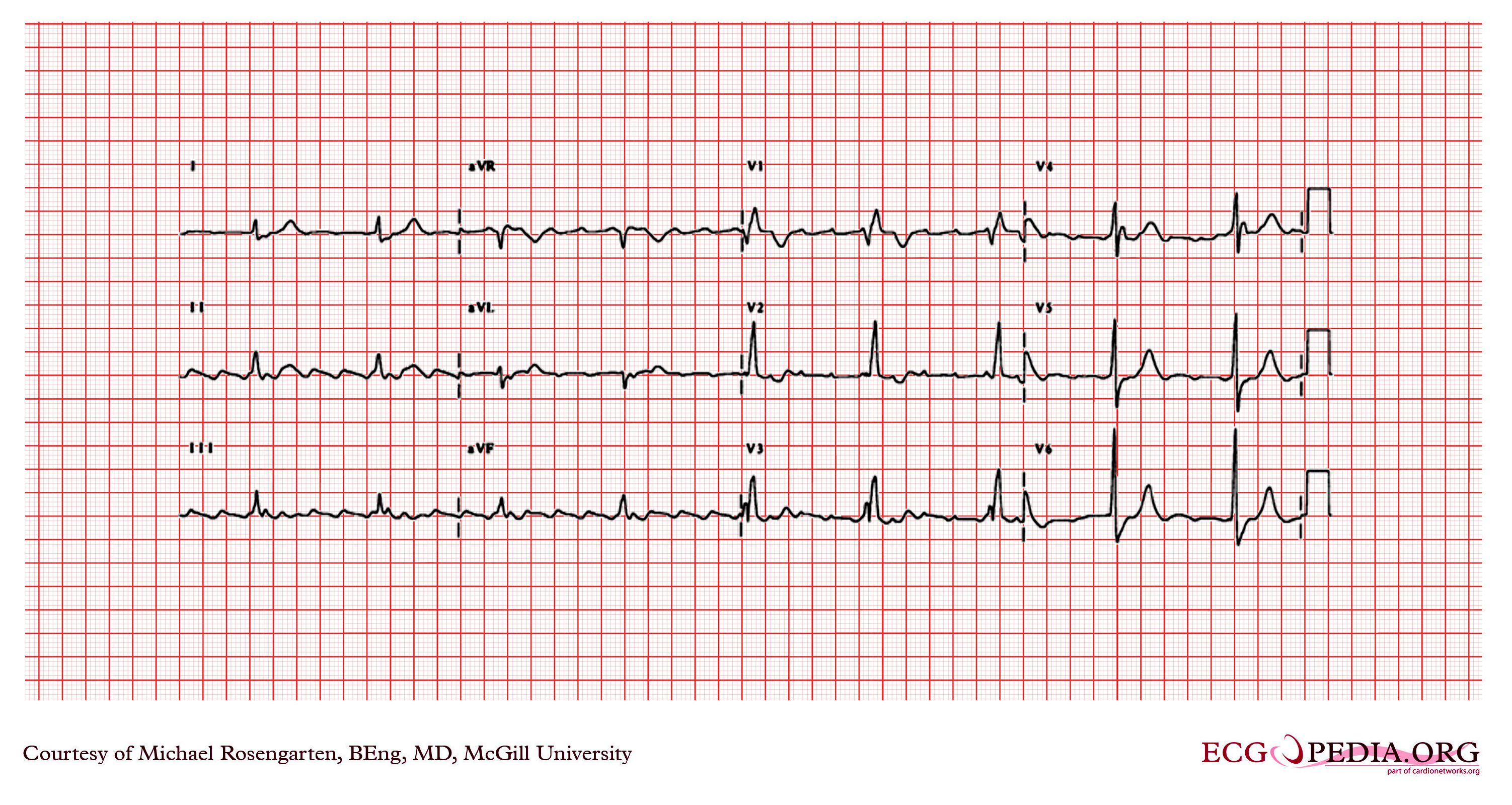
Atrial flutter is a reenterant arrhythmia, with atrial rates between 240 and 340/min, with a regular ventricular response and a saw tooth pattern on EKG.
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated. Atrial flutter can be a life-threatening condition and must be treated as such irrespective of the causes.
Common Causes
- Acute coronary syndromes
- Cardiomyopathy
- Carbon monoxide poisoning
- Congenital heart disease
- Hypertensive heart disease
- Hyperthyroidism
- Mitral valve disease[1] [2]
- Pulmonary embolism
- Myocardial infarction
Management
Diagnostic Approach
Shown below is an algorithm summarizing the initial approach to atrial fibrillation.
Characterize the symptoms:
Characterize the timing of the symptoms:
❑ Duration
| |||||||||||||||||||||||||||||||||||
Identify possible triggers:
| |||||||||||||||||||||||||||||||||||
❑ Examine the patient ❑ Order an ECG ♦ Atrial flutter rhythm
| |||||||||||||||||||||||||||||||||||
❑ Order a transthoracic echocardiogram | |||||||||||||||||||||||||||||||||||
Therapeutic Approach
Shown below is an algorithm summarizing the therapeutic approach to atrial flutter.[3]
| Atrial flutter | |||||||||||||||||||||||||||||||||||||||
| Unstable | Stable | ||||||||||||||||||||||||||||||||||||||
❑ Look for the presence of any of these:
| ❑ Administer anticoagulation therapy based on the risk of stroke, if total duration of flutter > 48 hours ❑ Administer rate control therapy (AV nodal blockers) THEN ❑ Attempt conversion
| ||||||||||||||||||||||||||||||||||||||
❑ Assess need for therapy to prevent recurrence | |||||||||||||||||||||||||||||||||||||||
❑ Administer antiarrythmic therapy to prevent recurrences
❑ Consider catheter ablation if antiarrhythmic therapy fails | |||||||||||||||||||||||||||||||||||||||
Acute management of atrial flutter
| ||||||||||||
| ||||||||||||
Long term management of atrial flutter
| |||||||||||||||
Pharmacological cardioversion
| ||||||||||||
Do's
- It is often the result of pulmonary disease exacerbation, pericarditis, and open heart surgery
- Radiofrequency catheter ablation is superior to medical therapy.
Anticoagulation for atrial flutter
- CHADS2 score
- Congestive heart failure - 1
- Hypertension -1
- Age > 75 -1
- Diabetes Mellitus -1
- Stroke or TIA - 2
- Score > 2 anticoagulate
- Score < 2 Aspirin may be sufficient
- CHA2DS2 VASc score
- Congestive heart failure - 1
- Hypertension -1
- Age > 75 - 2
- Diabetes Mellitus -1
- Stroke or TIA - 2
- Vascular disease - 1
- Age - 65 -74
- Sex - Female
- Score 0 low risk, no anticoagulation or aspirin 81-324
- Score 1, moderate risk, oral anticoagulation or Aspirin
- Score 2 or more, oral anticoagulation
Don'ts
References
- ↑ Gutierrez SD, Earing MG, Singh AK, Tweddell JS, Bartz PJ (2012). "Atrial Tachyarrhythmias and the Cox-maze Procedure in Congenital Heart Disease". Congenit Heart Dis. doi:10.1111/chd.12031. PMID 23280242. Unknown parameter
|month=ignored (help) - ↑ Granada, J.; Uribe, W.; Chyou, PH.; Maassen, K.; Vierkant, R.; Smith, PN.; Hayes, J.; Eaker, E.; Vidaillet, H. (2000). "Incidence and predictors of atrial flutter in the general population". J Am Coll Cardiol. 36 (7): 2242–6. PMID 11127467. Unknown parameter
|month=ignored (help) - ↑ "ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary". Retrieved 15 August 2013.