Aortic regurgitation physical examination: Difference between revisions
(→Eyes) |
|||
| (85 intermediate revisions by 11 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{| class="infobox" style="float:right;" | |||
|- | |||
| [[File:Siren.gif|30px|link=Aortic regurgitation resident survival guide]]|| <br> || <br> | |||
| [[Aortic regurgitation resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] | |||
|} | |||
{{Infobox disease | |||
| Name = Aortic insufficiency | |||
| Image = aortic_regurgitation.jpg| | |||
}} | |||
{{Aortic insufficiency}} | {{Aortic insufficiency}} | ||
{{CMG}}; {{AE}} {{CZ}}; {{VK}}; {{LG}}; {{USAMA}} | |||
{{ | ==Overview== | ||
Acute aortic regurgitation (AR) is characterized by the presence of a low pitched early diastolic murmur that is best heard at the right 2nd intercostal space, decreased or absent S1, and increased P2. Chronic AR is characterized by the presence of a high pitched holodiastolic decrescendo murmur that is best heard at the upper left sternal border and that increases with sitting forward, expiration, and handgrip. In chronic AR, a wide pulse pressure (≥ 60 mmHg), a [[S3]], and [[Corrigan's pulse]] might be present. An [[Systolic murmur|ejection systolic 'flow' murmur]] may also be present. The [[apex beat]] is typically displaced down and to the left. A patient with chronic AR may present with signs of [[congestive heart failure|congestive heart failure.]]<ref>Enriquez-Sarano M, Tajik AJ. Clinical practice. Aortic regurgitation. N Engl J Med 2004; 351:1539</ref><ref name="pmid8629648">{{cite journal| author=Desjardins VA, Enriquez-Sarano M, Tajik AJ, Bailey KR, Seward JB| title=Intensity of murmurs correlates with severity of valvular regurgitation. | journal=Am J Med | year= 1996 | volume= 100 | issue= 2 | pages= 149-56 | pmid=8629648 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8629648 }} </ref><ref name="pmid11498061">{{cite journal| author=Tribouilloy CM, Enriquez-Sarano M, Mohty D, Horn RA, Bailey KR, Seward JB et al.| title=Pathophysiologic determinants of third heart sounds: a prospective clinical and Doppler echocardiographic study. | journal=Am J Med | year= 2001 | volume= 111 | issue= 2 | pages= 96-102 | pmid=11498061 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11498061 }} </ref> | |||
==Physical Examination== | |||
===Vital Signs=== | |||
The following variations can be seen in Aortic Regurgitation.The following signs can be noticed in patients with Aortic Regurgitation.<ref name="pmid12729428">{{cite journal| author=Babu AN, Kymes SM, Carpenter Fryer SM| title=Eponyms and the diagnosis of aortic regurgitation: what says the evidence? | journal=Ann Intern Med | year= 2003 | volume= 138 | issue= 9 | pages= 736-42 | pmid=12729428 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12729428 }} </ref><ref name="pmid3963660">{{cite journal| author=Grayburn PA, Smith MD, Handshoe R, Friedman BJ, DeMaria AN| title=Detection of aortic insufficiency by standard echocardiography, pulsed Doppler echocardiography, and auscultation. A comparison of accuracies. | journal=Ann Intern Med | year= 1986 | volume= 104 | issue= 5 | pages= 599-605 | pmid=3963660 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3963660 }} </ref><ref name="pmid14325909">{{cite journal| author=FRANK MJ, CASANEGRA P, MIGLIORI AJ, LEVINSON GE| title=THE CLINICAL EVALUATION OF AORTIC REGURGITATION, WITH SPECIAL REFERENCE TO A NEGLECTED SIGN: THE POPLITEAL-BRACHIAL PRESSURE GRADIENT. | journal=Arch Intern Med | year= 1965 | volume= 116 | issue= | pages= 357-65 | pmid=14325909 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14325909 }} </ref> | |||
====Pulse and Blood Pressure==== | |||
*In acute aortic insufficiency, there may be a [[wide pulse pressure]] intitally. As the [[left ventricle]] fails, the [[pulse pressure]] narrows (the [[left ventricular end diastolic pressure]] rises to equal the [[diastolic blood pressure]]). [[Stroke volume]] of the [[left ventricle]] declines reducing the [[systolic blood pressure]]. In some cases, the sharply rising [[left ventricular end diastolic pressure]] causes the [[mitral valve]] to close earlier during [[diastole]]. This early closure prevents backward flow of [[blood]] into the pulmonary vascular bed and often keeps the aortic diastolic pressure from falling too low. Sometimes there may not be a [[wide pulse pressure]]. | |||
*In chronic aortic insufficiency, there is often a [[wide pulse pressure]] during the early compensatory period. The [[diastolic blood pressure]] is often < 60 mmHg and the [[pulse pressure]] often exceeds 100 mmHg. In younger patients the vasculature is more compliant, and the [[pulse pressure]] may not be as wide. | |||
*Bounding peripheral pulses (known as [[Watson's water hammer pulse]]) may be present. | |||
*There is often a compensatory [[tachycardia]] to compensate for the reduced [[stroke volume]]. | |||
* | |||
=== | ===Head and Neck=== | ||
*[[De Musset sign]]: Bobbing of the [[head]] with each heartbeat may be present. | |||
*[[ | *[[Lighthouse sign]]: [[Blanching]] and [[flushing]] of the forehead may be present. | ||
*[[Corrigan's pulse]] | *[[Corrigan's pulse]]: A rapid upstroke and collapse of the [[carotid artery]] [[pulse]] may be present. | ||
{{#ev:youtube| | {{#ev:youtube|rh7_MnjrOAY}} | ||
==Eyes== | ===Eyes=== | ||
*[[Becker sign]]: | *[[Becker sign]]: Systolic pulsations of the [[retinal arteries]] may be present. | ||
*[[Ashrafian sign]]: Pulsatile pseudo-[[proptosis]] may be present.<ref name="pmid16503268">{{cite journal |author=Ashrafian H |title=Pulsatile pseudo-proptosis, aortic regurgitation and 31 eponyms |journal=[[International Journal of Cardiology]] |volume=107 |issue=3 |pages=421–3 |year=2006 |month=March |pmid=16503268 |doi=10.1016/j.ijcard.2005.01.060 |url=http://linkinghub.elsevier.com/retrieve/pii/S0167-5273(05)00451-1 |accessdate=2012-04-15}}</ref> | |||
*[[Landolfi's sign]]: Alternating constriction and dilatation of the [[pupil]]s may be present<ref name="pmid35865711">{{cite journal| author=Ghosh R, Sengupta S, Siraj SM, Benito-León J| title=Landolfi's Sign: A Riddle for Primary Care Physicians. | journal=J Prim Care Spec | year= 2020 | volume= 1 | issue= 1 | pages= 13-14 | pmid=35865711 | doi=10.4103/jopcs.jopcs_14_20 | pmc=9297338 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=35865711 }} </ref>. | |||
==Throat== | ===Throat=== | ||
*[[ | *[[Müller's sign]]: Systolic pulsations of the [[uvula]] may be present.<ref name="pmid16855259">{{cite journal |author=Williams BR, Steinberg JP |title=Images in clinical medicine. Müller's sign |journal=[[The New England Journal of Medicine]] |volume=355 |issue=3 |pages=e3 |year=2006 |month=July |pmid=16855259 |doi=10.1056/NEJMicm050642 |url=http://dx.doi.org/10.1056/NEJMicm050642 |accessdate=2012-04-15}}</ref> | ||
{{#ev:youtube|HLMqkHZ-Mvo}} | |||
== | ===Heart=== | ||
===Palpation=== | ====Palpation==== | ||
*Apical impulse: | *[[Apical impulse]]: | ||
* | :*The [[point of maximal impulse]] is diffuse and hyperdynamic. The [[apical impulse]] is displaced laterally and inferiorly. | ||
*[[Thrill|Systolic thrill]]: | |||
:*[[Thrill|Systolic thrill]] (palpable ventricular filling wave) is felt at the [[apex]] and at the [[base]] of the [[heart]]. | |||
===Auscultation=== | ====Auscultation==== | ||
*[[S4]] | =====Heart Sounds===== | ||
:*An [[S3]] [[gallop]] is present if [[left ventricular dysfunction]] is present. | |||
:*An [[S4]] may be present consistent with impaired [[left ventricular]] filling against a [[LVH|hypertrophied left ventricular wall]]. | |||
=====Murmurs===== | |||
*An early diastolic, low pitched, decrescendo murmur in acute AR vs high pitched holodiastolic decrescendo murmur in chromic AR. | |||
:*Position: Patient seated and leans forward with breath held in expiration. | |||
:*Best heard at the aortic area with the diaphragm. | |||
:*Radiate to the right parasternal region ([[ascending aortic aneurysm]] should be excluded). | |||
<div align="left"> | |||
<gallery heights="145" widths="375"> | |||
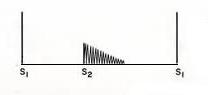
image:Early diastolic.jpg|Early diastolic murmur: [[Aortic Insufficiency]] | |||
Image:AI Left Sternal Border.jpg|Smooth A<sub>2</sub> and early diastolic murmur: [[Aortic Insufficiency]] | |||
</gallery> | |||
</div> | |||
{{clr}} | |||
{{#ev:youtube|shLGJi8dVQ8}} | |||
* | *Ejection systolic flow murmur: | ||
:*Best heard at the aortic area (only a concomitant [[aortic stenosis]] causes [[murmur]] with an ejection click). | |||
:*Heard in cases of increased [[stroke volume]] due to left ventricular volume overload. | |||
{{#ev:youtube|IfJotUSNgdo}} | {{#ev:youtube|IfJotUSNgdo}} | ||
*[[Austin Flint murmur]]: | |||
:*Quality: Soft mid-diastolic rumble | |||
:*Best heard at the cardiac apex | |||
:*Anterior [[mitral valve]] leaflet hit by regurgitant [[blood flow]] from the severe aortic regurgitation results in partial closure of the mitral leaflets causing [[Austin Flint murmur]]. | |||
{{#ev:youtube|y5CcncRHl38}} | {{#ev:youtube|y5CcncRHl38}} | ||
== | ===Lungs=== | ||
*[[ | *[[Pulmonary edema]] and [[rales]] may be present. | ||
===Abdomen=== | |||
*[[Rosenbach's sign]]: Systolic Pulsations of [[liver]] may be present. | |||
*[[Gerhardt's sign]]: Systolic pulsations of [[spleen]] may be present. | |||
* | ===Extremities=== | ||
* | *Upper extremities: | ||
:*[[Mayen's sign]]: Diastolic drop of > 15 mmHg with the arm raised. | |||
:*[[Quincke's sign]]: Pulsation of the [[capillary]] bed in the nail. | |||
{{#ev:youtube|9m_0RAQDFHM}} | |||
* | *Lower extremities: | ||
* | :*[[Traube's sign]]: Systolic and diastolic murmurs described as 'pistol shots' heard over the [[femoral artery]] when it is gradually compressed. | ||
:*[[Duroziez's sign]]: Systolic and diastolic murmurs heard over the [[femoral artery]] with proximal or distal compression of the [[femoral artery]] respectively. | |||
:*[[Lincoln's sign]]: A pulsatile [[Popliteal artery|popliteal]] pulse. | |||
:*[[Hill's sign]]: A ≥ 20 mmHg difference in popliteal and brachial systolic cuff pressures, seen in chronic severe AR. Considered to be an artifact of sphygmomanometric lower limb pressure measurement.<ref>{{cite journal |author=Kutryk M, Fitchett D |title=Hill's sign in aortic regurgitation: enhanced pressure wave transmission or artefact? |journal=The Canadian journal of cardiology |volume=13 |issue=3 |pages=237–40 |year=1997 |pmid=9117911 |doi=}}</ref> | |||
* | :*[[Sherman's sign]]: The [[dorsalis pedis pulse]] is located quickly and is unexpectedly prominent in a patient over 75 years of age. | ||
* | |||
==Underlying Causes of Aortic Insufficiency to be Cognizant of During the Physical Examination== | |||
: | During the physical exam, you should be looking for signs that would indicate the underlying cause of aortic insufficiency including signs of:<ref name="pmid24603191">{{cite journal| author=Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA et al.| title=2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. | journal=J Am Coll Cardiol | year= 2014 | volume= 63 | issue= 22 | pages= e57-185 | pmid=24603191 | doi=10.1016/j.jacc.2014.02.536 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24603191 }} </ref><ref name="pmid15172299">{{cite journal |author=Onorati F, De Santo LS, Carozza A, De Feo M, Renzulli A, Cotrufo M |title=Marfan syndrome as a predisposing factor for traumatic aortic insufficiency |journal=[[The Annals of Thoracic Surgery]] |volume=77 |issue=6 |pages=2192–4 |year=2004 |month=June |pmid=15172299 |doi=10.1016/S0003-4975(03)01409-7 |url=http://linkinghub.elsevier.com/retrieve/pii/S0003497503014097 |accessdate=2011-03-28}}</ref> | ||
: | *[[Endocarditis signs and physical examination|Infective endocarditis]] | ||
*[[Marfan syndrome]] | |||
*[[Spondyloarthropathy]] | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[CME Category::Cardiology]] | |||
[[Category:Disease]] | |||
[[Category:Cardiology]] | |||
[[Category:Valvular heart disease]] | [[Category:Valvular heart disease]] | ||
[[Category: | [[Category:Congenital heart disease]] | ||
[[Category: | [[Category:Surgery]] | ||
[[Category:Cardiac surgery]] | [[Category:Cardiac surgery]] | ||
[[Category: | [[Category:Emergency medicine]] | ||
[[Category: | [[Category:Intensive care medicine]] | ||
[[Category:Up-To-Date cardiology]] | |||
[[Category:Up-To-Date]] | |||
Latest revision as of 12:46, 31 March 2024
| Resident Survival Guide |
| Aortic insufficiency | |
| Classification and external resources | |

|
|---|
|
Aortic Regurgitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Acute Aortic regurgitation |
|
Chronic Aortic regurgitation |
|
Special Scenarios |
|
Case Studies |
|
Aortic regurgitation physical examination On the Web |
|
American Roentgen Ray Society Images of Aortic regurgitation physical examination |
|
Risk calculators and risk factors for Aortic regurgitation physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Varun Kumar, M.B.B.S. [3]; Lakshmi Gopalakrishnan, M.B.B.S. [4]; Usama Talib, BSc, MD [5]
Overview
Acute aortic regurgitation (AR) is characterized by the presence of a low pitched early diastolic murmur that is best heard at the right 2nd intercostal space, decreased or absent S1, and increased P2. Chronic AR is characterized by the presence of a high pitched holodiastolic decrescendo murmur that is best heard at the upper left sternal border and that increases with sitting forward, expiration, and handgrip. In chronic AR, a wide pulse pressure (≥ 60 mmHg), a S3, and Corrigan's pulse might be present. An ejection systolic 'flow' murmur may also be present. The apex beat is typically displaced down and to the left. A patient with chronic AR may present with signs of congestive heart failure.[1][2][3]
Physical Examination
Vital Signs
The following variations can be seen in Aortic Regurgitation.The following signs can be noticed in patients with Aortic Regurgitation.[4][5][6]
Pulse and Blood Pressure
- In acute aortic insufficiency, there may be a wide pulse pressure intitally. As the left ventricle fails, the pulse pressure narrows (the left ventricular end diastolic pressure rises to equal the diastolic blood pressure). Stroke volume of the left ventricle declines reducing the systolic blood pressure. In some cases, the sharply rising left ventricular end diastolic pressure causes the mitral valve to close earlier during diastole. This early closure prevents backward flow of blood into the pulmonary vascular bed and often keeps the aortic diastolic pressure from falling too low. Sometimes there may not be a wide pulse pressure.
- In chronic aortic insufficiency, there is often a wide pulse pressure during the early compensatory period. The diastolic blood pressure is often < 60 mmHg and the pulse pressure often exceeds 100 mmHg. In younger patients the vasculature is more compliant, and the pulse pressure may not be as wide.
- Bounding peripheral pulses (known as Watson's water hammer pulse) may be present.
- There is often a compensatory tachycardia to compensate for the reduced stroke volume.
Head and Neck
- De Musset sign: Bobbing of the head with each heartbeat may be present.
- Lighthouse sign: Blanching and flushing of the forehead may be present.
- Corrigan's pulse: A rapid upstroke and collapse of the carotid artery pulse may be present.
{{#ev:youtube|rh7_MnjrOAY}}
Eyes
- Becker sign: Systolic pulsations of the retinal arteries may be present.
- Ashrafian sign: Pulsatile pseudo-proptosis may be present.[7]
- Landolfi's sign: Alternating constriction and dilatation of the pupils may be present[8].
Throat
- Müller's sign: Systolic pulsations of the uvula may be present.[9]
{{#ev:youtube|HLMqkHZ-Mvo}}
Heart
Palpation
- The point of maximal impulse is diffuse and hyperdynamic. The apical impulse is displaced laterally and inferiorly.
- Systolic thrill (palpable ventricular filling wave) is felt at the apex and at the base of the heart.
Auscultation
Heart Sounds
- An S3 gallop is present if left ventricular dysfunction is present.
- An S4 may be present consistent with impaired left ventricular filling against a hypertrophied left ventricular wall.
Murmurs
- An early diastolic, low pitched, decrescendo murmur in acute AR vs high pitched holodiastolic decrescendo murmur in chromic AR.
- Position: Patient seated and leans forward with breath held in expiration.
- Best heard at the aortic area with the diaphragm.
- Radiate to the right parasternal region (ascending aortic aneurysm should be excluded).
-
Early diastolic murmur: Aortic Insufficiency
-
Smooth A2 and early diastolic murmur: Aortic Insufficiency
{{#ev:youtube|shLGJi8dVQ8}}
- Ejection systolic flow murmur:
- Best heard at the aortic area (only a concomitant aortic stenosis causes murmur with an ejection click).
- Heard in cases of increased stroke volume due to left ventricular volume overload.
{{#ev:youtube|IfJotUSNgdo}}
- Quality: Soft mid-diastolic rumble
- Best heard at the cardiac apex
- Anterior mitral valve leaflet hit by regurgitant blood flow from the severe aortic regurgitation results in partial closure of the mitral leaflets causing Austin Flint murmur.
{{#ev:youtube|y5CcncRHl38}}
Lungs
- Pulmonary edema and rales may be present.
Abdomen
- Rosenbach's sign: Systolic Pulsations of liver may be present.
- Gerhardt's sign: Systolic pulsations of spleen may be present.
Extremities
- Upper extremities:
- Mayen's sign: Diastolic drop of > 15 mmHg with the arm raised.
- Quincke's sign: Pulsation of the capillary bed in the nail.
{{#ev:youtube|9m_0RAQDFHM}}
- Lower extremities:
- Traube's sign: Systolic and diastolic murmurs described as 'pistol shots' heard over the femoral artery when it is gradually compressed.
- Duroziez's sign: Systolic and diastolic murmurs heard over the femoral artery with proximal or distal compression of the femoral artery respectively.
- Lincoln's sign: A pulsatile popliteal pulse.
- Hill's sign: A ≥ 20 mmHg difference in popliteal and brachial systolic cuff pressures, seen in chronic severe AR. Considered to be an artifact of sphygmomanometric lower limb pressure measurement.[10]
- Sherman's sign: The dorsalis pedis pulse is located quickly and is unexpectedly prominent in a patient over 75 years of age.
Underlying Causes of Aortic Insufficiency to be Cognizant of During the Physical Examination
During the physical exam, you should be looking for signs that would indicate the underlying cause of aortic insufficiency including signs of:[11][12]
References
- ↑ Enriquez-Sarano M, Tajik AJ. Clinical practice. Aortic regurgitation. N Engl J Med 2004; 351:1539
- ↑ Desjardins VA, Enriquez-Sarano M, Tajik AJ, Bailey KR, Seward JB (1996). "Intensity of murmurs correlates with severity of valvular regurgitation". Am J Med. 100 (2): 149–56. PMID 8629648.
- ↑ Tribouilloy CM, Enriquez-Sarano M, Mohty D, Horn RA, Bailey KR, Seward JB; et al. (2001). "Pathophysiologic determinants of third heart sounds: a prospective clinical and Doppler echocardiographic study". Am J Med. 111 (2): 96–102. PMID 11498061.
- ↑ Babu AN, Kymes SM, Carpenter Fryer SM (2003). "Eponyms and the diagnosis of aortic regurgitation: what says the evidence?". Ann Intern Med. 138 (9): 736–42. PMID 12729428.
- ↑ Grayburn PA, Smith MD, Handshoe R, Friedman BJ, DeMaria AN (1986). "Detection of aortic insufficiency by standard echocardiography, pulsed Doppler echocardiography, and auscultation. A comparison of accuracies". Ann Intern Med. 104 (5): 599–605. PMID 3963660.
- ↑ FRANK MJ, CASANEGRA P, MIGLIORI AJ, LEVINSON GE (1965). "THE CLINICAL EVALUATION OF AORTIC REGURGITATION, WITH SPECIAL REFERENCE TO A NEGLECTED SIGN: THE POPLITEAL-BRACHIAL PRESSURE GRADIENT". Arch Intern Med. 116: 357–65. PMID 14325909.
- ↑ Ashrafian H (2006). "Pulsatile pseudo-proptosis, aortic regurgitation and 31 eponyms". International Journal of Cardiology. 107 (3): 421–3. doi:10.1016/j.ijcard.2005.01.060. PMID 16503268. Retrieved 2012-04-15. Unknown parameter
|month=ignored (help) - ↑ Ghosh R, Sengupta S, Siraj SM, Benito-León J (2020). "Landolfi's Sign: A Riddle for Primary Care Physicians". J Prim Care Spec. 1 (1): 13–14. doi:10.4103/jopcs.jopcs_14_20. PMC 9297338 Check
|pmc=value (help). PMID 35865711 Check|pmid=value (help). - ↑ Williams BR, Steinberg JP (2006). "Images in clinical medicine. Müller's sign". The New England Journal of Medicine. 355 (3): e3. doi:10.1056/NEJMicm050642. PMID 16855259. Retrieved 2012-04-15. Unknown parameter
|month=ignored (help) - ↑ Kutryk M, Fitchett D (1997). "Hill's sign in aortic regurgitation: enhanced pressure wave transmission or artefact?". The Canadian journal of cardiology. 13 (3): 237–40. PMID 9117911.
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". J Am Coll Cardiol. 63 (22): e57–185. doi:10.1016/j.jacc.2014.02.536. PMID 24603191.
- ↑ Onorati F, De Santo LS, Carozza A, De Feo M, Renzulli A, Cotrufo M (2004). "Marfan syndrome as a predisposing factor for traumatic aortic insufficiency". The Annals of Thoracic Surgery. 77 (6): 2192–4. doi:10.1016/S0003-4975(03)01409-7. PMID 15172299. Retrieved 2011-03-28. Unknown parameter
|month=ignored (help)
- CS1 maint: Multiple names: authors list
- CS1 maint: Explicit use of et al.
- Pages with citations using unsupported parameters
- CS1 errors: PMC
- CS1 errors: PMID
- Disease
- Cardiology
- Valvular heart disease
- Congenital heart disease
- Surgery
- Cardiac surgery
- Emergency medicine
- Intensive care medicine
- Up-To-Date cardiology
- Up-To-Date