Anencephaly: Difference between revisions
No edit summary |
|||
| (46 intermediate revisions by the same user not shown) | |||
| Line 8: | Line 8: | ||
Name = Anencephaly | | Name = Anencephaly | | ||
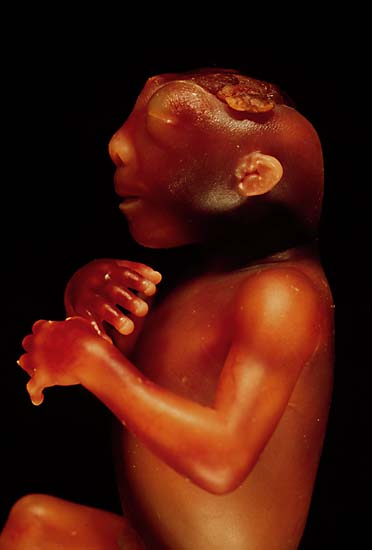
Image = Anencephaly side.jpg| | Image = Anencephaly side.jpg| | ||
Caption = The side view of the head of an anencephalic fetus. Source: https://en.wikipedia.org/| | Caption = The side view of the head of an anencephalic fetus. | ||
Source: https://en.wikipedia.org/| | |||
DiseasesDB = 705 | | DiseasesDB = 705 | | ||
ICD10 = {{ICD10|Q|00|0|q|00}} | | ICD10 = {{ICD10|Q|00|0|q|00}} | | ||
| Line 24: | Line 26: | ||
==Historical Perspective== | ==Historical Perspective== | ||
* Anencephaly was first recognized in the 16th century. In 1989, [[Aubrey Milunsky]] and his colleagues observed a reduction in the cases of [[neural tube defects]] in the mothers who took [[folic acid]] supplements during [[pregnancy]].<ref name="pmidPMID: 2478730">{{cite journal| author=Milunsky A, Jick H, Jick SS, Bruell CL, MacLaughlin DS, Rothman KJ | display-authors=etal| title=Multivitamin/folic acid supplementation in early pregnancy reduces the prevalence of neural tube defects. | journal=JAMA | year= 1989 | volume= 262 | issue= 20 | pages= 2847-52 | pmid=PMID: 2478730 | doi=10.1001/jama.262.20.2847 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2478730 }} </ref> | * Anencephaly was first recognized in the 16th century. In 1989, [[Aubrey Milunsky]] and his colleagues observed a [[reduction]] in the [[cases]] of [[neural tube defects]] in the [[mothers]] who took [[folic acid]] [[supplements]] during [[pregnancy]].<ref name="pmidPMID: 2478730">{{cite journal| author=Milunsky A, Jick H, Jick SS, Bruell CL, MacLaughlin DS, Rothman KJ | display-authors=etal| title=Multivitamin/folic acid supplementation in early pregnancy reduces the prevalence of neural tube defects. | journal=JAMA | year= 1989 | volume= 262 | issue= 20 | pages= 2847-52 | pmid=PMID: 2478730 | doi=10.1001/jama.262.20.2847 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2478730 }} </ref> | ||
* In 1992, Thresa was born with anencephaly. Her parents knew their daughter is going to die. So, they requested if her [[organs]] could be used for [[transplantation]]. This initiated a debate on anencephalic [[infant]] [[organ donation]].<ref name="pmidPMID 12774804">{{cite journal| author=Bard JS| title=The diagnosis is anencephaly and the parents ask about organ donation: now what? A guide for hospital counsel and ethics committees. | journal=West New Engl Law Rev | year= 1999 | volume= 21 | issue= 1 | pages= 49-95 | pmid=PMID 12774804 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12774804 }} </ref> | * In 1992, Thresa was born with anencephaly. Her parents knew their daughter is going to [[die]]. So, they requested if her [[organs]] could be used for [[transplantation]]. This initiated a debate on anencephalic [[infant]] [[organ donation]].<ref name="pmidPMID 12774804">{{cite journal| author=Bard JS| title=The diagnosis is anencephaly and the parents ask about organ donation: now what? A guide for hospital counsel and ethics committees. | journal=West New Engl Law Rev | year= 1999 | volume= 21 | issue= 1 | pages= 49-95 | pmid=PMID 12774804 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12774804 }} </ref> | ||
==Classification== | ==Classification== | ||
| Line 34: | Line 36: | ||
|- | |- | ||
| align="center" style="background:#ADD8E6;" |Meroanencephaly<ref name="pmidPMID 8286034">{{cite journal| author=Isada NB, Qureshi F, Jacques SM, Holzgreve W, Tout MJ, Johnson MP | display-authors=etal| title=Meroanencephaly: pathology and prenatal diagnosis. | journal=Fetal Diagn Ther | year= 1993 | volume= 8 | issue= 6 | pages= 423-8 | pmid=PMID 8286034 | doi=10.1159/000263862 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8286034 }} </ref> | | align="center" style="background:#ADD8E6;" |Meroanencephaly<ref name="pmidPMID 8286034">{{cite journal| author=Isada NB, Qureshi F, Jacques SM, Holzgreve W, Tout MJ, Johnson MP | display-authors=etal| title=Meroanencephaly: pathology and prenatal diagnosis. | journal=Fetal Diagn Ther | year= 1993 | volume= 8 | issue= 6 | pages= 423-8 | pmid=PMID 8286034 | doi=10.1159/000263862 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8286034 }} </ref> | ||
|Meroanencephaly is a rare form of anencephaly. [[Fetus]] born have [[clinical features]] including | |Meroanencephaly is a [[rare]] form of anencephaly. [[Fetus]] [[born]] have [[clinical features]] including [[misshape]]n [[skull]] [[bones]] and a [[vascular]] [[tissue]] [[protuberance]] called cerebrovasculosa. | ||
|- | |- | ||
| align="center" style="background:#ADD8E6;" |Holoanencephaly<ref name="pmidPMID 8286034" /> | | align="center" style="background:#ADD8E6;" |Holoanencephaly<ref name="pmidPMID 8286034" /> | ||
|It is the most common type of anencephaly. In this condition, the entire [[fetus]] [[brain]] fails to develop except for the [[brain stem]]. Usually, [[infant]] survives for only one day after [[birth]]. | |It is the most common type of anencephaly. In this [[condition]], the entire [[fetus]] [[brain]] fails to [[develop]] except for the [[brain stem]]. Usually, [[infant]] survives for only one day after [[birth]]. | ||
|- | |- | ||
| align="center" style="background:#ADD8E6;" |Craniorachischisis<ref name="pmidPMID: 25032496">{{cite journal| author=Greene ND, Copp AJ| title=Neural tube defects. | journal=Annu Rev Neurosci | year= 2014 | volume= 37 | issue= | pages= 221-42 | pmid=PMID: 25032496 | doi=10.1146/annurev-neuro-062012-170354 | pmc=4486472 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25032496 }} </ref> | | align="center" style="background:#ADD8E6;" |Craniorachischisis<ref name="pmidPMID: 25032496">{{cite journal| author=Greene ND, Copp AJ| title=Neural tube defects. | journal=Annu Rev Neurosci | year= 2014 | volume= 37 | issue= | pages= 221-42 | pmid=PMID: 25032496 | doi=10.1146/annurev-neuro-062012-170354 | pmc=4486472 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25032496 }} </ref> | ||
|It is the most [[severe]] type of anencephaly. Along with the [[cranial]] defect, [[fetus]] also has a defect in the [[vertebral column]] exposing the underlying [[neural tissue]]. [[Area cerebrovasculosa]] and [[area medullovasculosa]] fill the areas with [[cranial]] and [[spinal]] [[defects]]. | |It is the most [[severe]] [[type]] of anencephaly. Along with the [[cranial]] [[defect]], [[fetus]] also has a [[defect]] in the [[vertebral column]] exposing the underlying [[neural tissue]]. [[Area cerebrovasculosa]] and [[area medullovasculosa]] fill the areas with [[cranial]] and [[spinal]] [[defects]]. | ||
|} | |} | ||
== | ==Pathophysiology== | ||
* By the 3rd week of gestation, the embryo has 3 layers, from outer to inner these layers are [[ectoderm]], [[mesoderm]] and [[endoderm]]. [[Notochord]] in the [[mesoderm]] sends signal molecule called [[Sonic Hedgehog]] protein to the overlying ectoderm forming it a [[neuroectoderm]].<ref>[[Neuroectoderm]] becomes a [[neural plate]].{{cite web|url=https://www.ncbi.nlm.nih.gov/books/NBK542285/|title=Embryology, Neural Tube - StatPearls - NCBI Bookshelf|format=|work=|accessdate=}}</ref> | * By the 3rd week of gestation, the embryo has 3 layers, from outer to inner these layers are [[ectoderm]], [[mesoderm]] and [[endoderm]]. [[Notochord]] in the [[mesoderm]] sends signal molecule called [[Sonic Hedgehog]] protein to the overlying ectoderm forming it a [[neuroectoderm]].<ref>[[Neuroectoderm]] becomes a [[neural plate]].{{cite web|url=https://www.ncbi.nlm.nih.gov/books/NBK542285/|title=Embryology, Neural Tube - StatPearls - NCBI Bookshelf|format=|work=|accessdate=}}</ref> | ||
* The [[neural plate]] folds and closes to form a tube-like structure called [[neural tube]] and [[neural crest cells]]. The [[neural tube]] then goes on to form structures of the adult [[brain]].<ref>{{cite book | last = Sadler | first = T. W. | title = Langman's medical embryology | publisher = Lippincott Williams & Wilkins | location = Philadelphia | year = 2006 | isbn = 9780781794855 }}</ref> | * The [[neural plate]] folds and closes to form a tube-like structure called [[neural tube]] and [[neural crest cells]]. The [[neural tube]] then goes on to form structures of the adult [[brain]].<ref>{{cite book | last = Sadler | first = T. W. | title = Langman's medical embryology | publisher = Lippincott Williams & Wilkins | location = Philadelphia | year = 2006 | isbn = 9780781794855 }}</ref> | ||
* A [[neural tube defect]] occurs if the the opening of the [[neural tube]], called [[neuropore]], fails to close in the 4th week of [[gestation]]. [[Neural tube]] has two [[neuropores]], rostral and caudial. [[Anencephaly]] results from failure of the [[rostral]] [[neuropore]] to close [[anteriorly]] around day 25.<ref name="pmidPMID: 25032496">{{cite journal| author=Greene ND, Copp AJ| title=Neural tube defects. | journal=Annu Rev Neurosci | year= 2014 | volume= 37 | issue= | pages= 221-42 | pmid=PMID: 25032496 | doi=10.1146/annurev-neuro-062012-170354 | pmc=4486472 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25032496 }} </ref> | |||
A [[neural tube defect]] occurs if the the opening of the [[neural tube]], called [[neuropore]], fails to close in the 4th week of [[gestation]]. [[Neural tube]] has two [[neuropores]], rostral and caudial. [[Anencephaly]] results from failure of the [[rostral]] [[neuropore]] to close [[anteriorly]] around day 25.<ref name="pmidPMID: 25032496">{{cite journal| author=Greene ND, Copp AJ| title=Neural tube defects. | journal=Annu Rev Neurosci | year= 2014 | volume= 37 | issue= | pages= 221-42 | pmid=PMID: 25032496 | doi=10.1146/annurev-neuro-062012-170354 | pmc=4486472 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25032496 }} </ref> | |||
The craniofacial abnormalities in anencephaly are caused by abnormal induction by the neural crest cells.<ref name="pmidPMID 16225807">{{cite journal| author=Sarnat HB, Flores-Sarnat L| title=Embryology of the neural crest: its inductive role in the neurocutaneous syndromes. | journal=J Child Neurol | year= 2005 | volume= 20 | issue= 8 | pages= 637-43 | pmid=PMID 16225807 | doi=10.1177/08830738050200080101 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16225807 }} </ref> | * The craniofacial abnormalities in anencephaly are caused by abnormal induction by the neural crest cells.<ref name="pmidPMID 16225807">{{cite journal| author=Sarnat HB, Flores-Sarnat L| title=Embryology of the neural crest: its inductive role in the neurocutaneous syndromes. | journal=J Child Neurol | year= 2005 | volume= 20 | issue= 8 | pages= 637-43 | pmid=PMID 16225807 | doi=10.1177/08830738050200080101 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16225807 }} </ref> | ||
== | ==Clinical Features== | ||
*[[Infants]] born with anencephaly have the following clinical features:<ref name="pmidPMID: 25386414">{{cite journal| author=Gole RA, Meshram PM, Hattangdi SS| title=Anencephaly and its associated malformations. | journal=J Clin Diagn Res | year= 2014 | volume= 8 | issue= 9 | pages= AC07-9 | pmid=PMID: 25386414 | doi=10.7860/JCDR/2014/10402.4885 | pmc=4225866 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25386414 }} </ref> | |||
**Facial features: [[Cleft lip]], [[cleft palate]]. | |||
**CNS: Absence of bony covering over the back of the [[head]], [[spina bifida]], [[blindness]], [[deafness]]. | |||
**GIT: Absence or underdeveloped [[organs]], [[gastroschisis]], [[omphalocele]]. | |||
**Genito-urinary system: [[Hypospadia]]s, penile [[hypoplasia]], renal [[agenesis]]. | |||
**Skeletal system: [[Clubbed foot]], clubbed hands. | |||
**Lungs: Diapharagmatic [[hernia]]. | |||
==Differentiating Anencephalopathy from other Disorders== | ==Differentiating Anencephalopathy from other Disorders== | ||
At times, anencephaly could be misdiagnosed with other similar [[diagnosis]] such as [[exencephaly]] | At times, anencephaly could be [[misdiagnosed]] with other similar [[diagnosis]] such as; | ||
* [[exencephaly]] | |||
* [[microcephaly]]<ref>{{cite web |url=https://psychology.wikia.org/wiki/Anencephaly |title=Anencephaly | Psychology Wiki | Fandom |format= |work= |accessdate=}}a</ref> | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
| Line 116: | Line 126: | ||
* Anencephaly and other physical and mental deformities have also been blamed on high exposure to such toxins as [[lead]], [[chromium]], [[mercury]], and [[nickel]]. <ref>Goldsmith, Alexander (1996, quoted by Millen and Holtz, "Dying for Growth")</ref> | * Anencephaly and other physical and mental deformities have also been blamed on high exposure to such toxins as [[lead]], [[chromium]], [[mercury]], and [[nickel]]. <ref>Goldsmith, Alexander (1996, quoted by Millen and Holtz, "Dying for Growth")</ref> | ||
== | ==Natural History, Complications, Prognosis== | ||
* [[Prognosis]] of children born with anencephaly is extremely poor as there is no cure or standard [[treatment]] available so far. Most [[anencephalic]] babies do not survive [[birth]], accounting for 55% of non-aborted cases. If the [[infant]] is not [[stillborn]], then he or she will usually die within a few hours or days after [[birth]] from [[cardiorespiratory arrest]].<ref>{{cite web |url=https://link.springer.com/book/10.1007/978-1-4020-8811-7 |title=Applications of Mass Spectrometry in Life Safety | SpringerLink |format= |work= |accessdate=}}</ref> | |||
* | * Anencephalic [[infants]] are not aggressively [[resuscitation|resuscitated]] as there is very little chance of the infant to achieve a full level of [[consciousness]]. Instead, [[clinicians]] prefer to provide them with adequate hydration, [[food|nutrition]] and comfort.<ref>{{cite web |url=https://psychology.wikia.org/wiki/Anencephaly |title=Anencephaly | Psychology Wiki | Fandom |format= |work= |accessdate=}}</ref> Artificial [[ventilation]], [[surgery]] (to fix any co-existing congenital defects), and medications are not considered an option as they have no role in any improvement.<ref>{{cite web |url=https://www.stlouischildrens.org/conditions-treatments/anencephaly |title=Anencephaly: Causes, Symptoms, Diagnosis and Treatment for Newborns | St. Louis Childrens Hospital |format= |work= |accessdate=}}</ref> Due to this poor prognosis, couple are discussed about the option of the terminating the [[pregnancy]] soon after the [[prenatal diagnosis]] is established.<ref name="pmidPMID: 22462001">{{cite journal| author=Machado IN, Martinez SD, Barini R| title=Anencephaly: do the pregnancy and maternal characteristics impact the pregnancy outcome? | journal=ISRN Obstet Gynecol | year= 2012 | volume= 2012 | issue= | pages= 127490 | pmid=PMID: 22462001 | doi=10.5402/2012/127490 | pmc=3302112 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22462001 }} </ref> | ||
* | == Diagnosis == | ||
===Diagnostic Criteria=== | |||
*The [[diagnosis]] of Anencephaly is made either during a [[prenatal scan]] or after the [[birth]]. | |||
:*In [[prenatal]] [[ultrasound]], [[features]] like [[absent]] [[calvarium]] and characteristic [[frog-like appearance]] or Micky mouse appearance of the [[fetus]] are [[diagnostic]].<ref>{{cite web |url=https://radiopaedia.org/articles/anencephaly |title=Anencephaly | Radiology Reference Article | Radiopaedia.org |format= |work= |accessdate=}}</ref> | |||
:*After the [[birth]], [[clinical features]] like lack of [[bony]] covering over the back of the [[head]] and less number of [[bones]] around the front and sides of the [[head]] are [[diagnostic]].<ref>{{cite web |url=http://www.childrenshospital.org/conditions-and-treatments/conditions/a/anencephaly/symptoms-and-causes |title=Anencephaly | Symptoms & Causes | Boston Children's Hospital |format= |work= |accessdate=}}</ref> | |||
=== | === Symptoms === | ||
* Majority of the [[infants]] are [[stillborn]] or die soon after [[birth]].<ref>{{cite web |url=https://www.cdc.gov/ncbddd/birthdefects/anencephaly.html#:~:text=Treatments,will%20die%20shortly%20after%20birth. |title=Facts about Anencephaly | CDC |format= |work= |accessdate=}}</ref><ref name="pmidPMID: 16827827">{{cite journal| author=Jaquier M, Klein A, Boltshauser E| title=Spontaneous pregnancy outcome after prenatal diagnosis of anencephaly. | journal=BJOG | year= 2006 | volume= 113 | issue= 8 | pages= 951-3 | pmid=PMID: 16827827 | doi=10.1111/j.1471-0528.2006.01014.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16827827 }} </ref> | |||
*[[Symptoms]] of anencephaly may include the following: | |||
:*Decrease or loss of [[consciousness]]. | |||
:*[[Blindness]] | |||
:*[[Deafness]] | |||
:*Inability to feel [[pain]].<ref name="pmidPMID: 7950143">{{cite journal| author=Murphy PA| title=Nursing the permanently unconscious. | journal=Trends Health Care Law Ethics | year= 1994 | volume= 9 | issue= 1 | pages= 33-6 | pmid=PMID: 7950143 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7950143 }} </ref> <ref>{{cite web |url=https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Cephalic-Disorders-Fact-Sheet |title=Cephalic Disorders Fact Sheet | National Institute of Neurological Disorders and Stroke |format= |work= |accessdate=}}</ref> | |||
The [[ | === Physical Examination === | ||
*Physical examination may be remarkable for: | |||
:*Flattened [[head]] | |||
:*Absence of the [[cranial]] [[vault]]<ref>{{cite web |url=https://emedicine.medscape.com/article/1181570-overview#a6 |title=Anencephaly: Overview, Pathophysiology, Causes |format= |work= |accessdate=}}</ref> | |||
:*Positive [[grasp reflex]] in both the [[hands]] and [[feet]] | |||
:*[[Moro reflex]] could be present or absent depending on the severity of the defect.<ref name="pmidPMID: 22778756">{{cite journal| author=Futagi Y, Toribe Y, Suzuki Y| title=The grasp reflex and moro reflex in infants: hierarchy of primitive reflex responses. | journal=Int J Pediatr | year= 2012 | volume= 2012 | issue= | pages= 191562 | pmid=PMID: 22778756 | doi=10.1155/2012/191562 | pmc=3384944 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22778756 }} </ref> | |||
:*A [[heart]] [[murmur]] could be present due to associated [[congenital heart disease]]. | |||
:*[[cleft lip]] and/or [[cleft palate]] could be present. | |||
:*[[Clubbed foot]] could be present. | |||
:*[[Gastroschisis]], [[omphalocele]], [[hypospadias]] could be present in some anencephalic infants.<ref name="pmidPMID: 25386414">{{cite journal| author=Gole RA, Meshram PM, Hattangdi SS| title=Anencephaly and its associated malformations. | journal=J Clin Diagn Res | year= 2014 | volume= 8 | issue= 9 | pages= AC07-9 | pmid=PMID: 25386414 | doi=10.7860/JCDR/2014/10402.4885 | pmc=4225866 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25386414 }} </ref> | |||
=== Laboratory Findings === | |||
==== Alpha-Fetoprotein ==== | |||
* [[Alpha-fetoprotein]] ([[AFP]]) levels can be measured in [[maternal]] [[serum]] (MSAFP), [[amniotic fluid]], and [[fetal]] [[plasma]].<ref name="pmidPMID 28613501">{{cite journal| author=| title=StatPearls | journal= | year= 2020 | volume= | issue= | pages= | pmid=PMID 28613501 | doi= | pmc= | url= }} </ref> | |||
* Normally, the level rises in early [[pregnancy]], peaks between 10 and 13th week, and then the level declines becoming extremely low near the term.<ref name="pmidPMID 4111729">{{cite journal| author=Gitlin D, Perricelli A, Gitlin GM| title=Synthesis of -fetoprotein by liver, yolk sac, and gastrointestinal tract of the human conceptus. | journal=Cancer Res | year= 1972 | volume= 32 | issue= 5 | pages= 979-82 | pmid=PMID 4111729 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4111729 }} </ref> | |||
* [[Alpha-fetoprotein]] ([[AFP]]) levels can be measured in [[maternal]] serum (MSAFP), [[amniotic fluid]], and [[fetal]] [[plasma]].<ref name="pmidPMID 28613501">{{cite journal| author=| title=StatPearls | journal= | year= 2020 | volume= | issue= | pages= | pmid=PMID 28613501 | doi= | pmc= | url= }} </ref> | * For the purpose of [[prenatal screening]], [[alpha-fetoprotein]] levels are checked and are found to elevated. This test is non-specific for [[NTD]], as [[AFP]] can also be elevated due to other [[maternal]] and [[fetal]] factors. Therefore, results should always be combined with [[ultrasound]] findings and the levels of [[Acetylcholinesterase]] ([[Acetylcholinesterase|AChE]]). | ||
* Normally, the level rises in early pregnancy, peaks between 10 and 13th week, and then the level declines becoming extremely low near the term.<ref name="pmidPMID 4111729">{{cite journal| author=Gitlin D, Perricelli A, Gitlin GM| title=Synthesis of -fetoprotein by liver, yolk sac, and gastrointestinal tract of the human conceptus. | journal=Cancer Res | year= 1972 | volume= 32 | issue= 5 | pages= 979-82 | pmid=PMID 4111729 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4111729 }} </ref> | |||
* For the purpose of prenatal screening, [[alpha-fetoprotein]] levels are checked and are found to elevated. This test is non-specific for [[NTD]], as [[AFP]] can also be elevated due to other maternal and fetal factors. Therefore, results should always be combined with ultrasound findings and the levels of [[Acetylcholinesterase]] ([[Acetylcholinesterase|AChE]]). | |||
===Acetylcholinesterase=== | ===Acetylcholinesterase=== | ||
| Line 167: | Line 190: | ||
|Decreased | |Decreased | ||
|} | |} | ||
===Imaging Findings=== | |||
====Ultrasound==== | |||
[[Ultrasound]] provides a [[definitive]] [[diagnosis]] of anencephaly before [[birth]]. It can often be [[diagnosed]] through a [[transvaginal]] [[ultrasound]] performed at 12th week [[postmenstrual]].<ref name="pmidPMID: 9060123">{{cite journal| author=Johnson SP, Sebire NJ, Snijders RJ, Tunkel S, Nicolaides KH| title=Ultrasound screening for anencephaly at 10-14 weeks of gestation. | journal=Ultrasound Obstet Gynecol | year= 1997 | volume= 9 | issue= 1 | pages= 14-6 | pmid=PMID: 9060123 | doi=10.1046/j.1469-0705.1997.09010014.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9060123 }} </ref> | |||
The [[ultrasound]] findings include: | |||
* Absent [[calvarium]]. | |||
*[[ | * No [[parenchymal]] [[tissue]] above the orbits. | ||
* | * Reduced [[crown rump length]] ([[CRL]]) | ||
* | * A characteristic [[frog-like appearance]] or [[Micky mouse appearance]] of the fetus due to absent [[brain]] and [[cranial]] bone and, protruding [[orbits]]. | ||
* | * A large amount of [[amniotic fluid]] called [[polyhydromnios]] is also seen.<ref>{{cite web |url=https://radiopaedia.org/articles/anencephaly |title=Anencephaly | Radiology Reference Article | Radiopaedia.org |format= |work= |accessdate=}}</ref> | ||
[[Image:Anencephaly- frog like appearance.gif|300px|right|thumb|Anencephaly - frog like appearance on prenatal USG. | |||
*[[ | |||
Source: <nowiki>https://radiopaedia.org</nowiki>]]. | |||
==Management == | ==Management == | ||
===Medical Therapy=== | ===Medical Therapy=== | ||
| Line 211: | Line 217: | ||
* At this point in time, there are no surgical options available.{{cite web |url=https://www.stlouischildrens.org/conditions-treatments/anencephaly |title=Anencephaly: Causes, Symptoms, Diagnosis and Treatment for Newborns | St. Louis Childrens Hospital |format= |work= |accessdate=}} | * At this point in time, there are no surgical options available.{{cite web |url=https://www.stlouischildrens.org/conditions-treatments/anencephaly |title=Anencephaly: Causes, Symptoms, Diagnosis and Treatment for Newborns | St. Louis Childrens Hospital |format= |work= |accessdate=}} | ||
==Prevention== | ===Prevention=== | ||
* Recent studies have shown that the addition of [[folic acid]] to the [[diet (nutrition)|diet]] of women of child-bearing age may significantly reduce, although not eliminate, the incidence of [[neural tube defects]]. Therefore, it is recommended that all [[women]] of child-bearing age consume 0.4 mg of [[folic acid]] daily, especially those attempting to conceive or who may possibly conceive, as this can reduce the risk to 0.03%.<ref>{{NINDS|anencephaly}}</ref> | |||
* Recent studies have shown that the addition of [[folic acid]] to the [[diet (nutrition)|diet]] of women of child-bearing age may significantly reduce, although not eliminate, the incidence of [[neural tube defects]]. Therefore, it is recommended that all women of child-bearing age consume 0.4 mg of [[folic acid]] daily, especially those attempting to conceive or who may possibly conceive, as this can reduce the risk to 0.03%.<ref>{{NINDS|anencephaly}}</ref> | * It is not advisable to wait until [[pregnancy]] has begun, since by the time a woman knows she is [[pregnant]], the critical time for the formation of a [[neural tube defect]] has usually already passed. A [[physician may]] prescribe even higher dosages of [[folic acid]] (4 mg/day) for women who have had a previous [[pregnancy]] with a [[neural tube defect]].<ref name="pmidPMID: 22439027">{{cite journal| author=Cavalli P| title=Prevention of Neural Tube Defects and proper folate periconceptional supplementation. | journal=J Prenat Med | year= 2008 | volume= 2 | issue= 4 | pages= 40-1 | pmid=PMID: 22439027 | doi= | pmc=3279093 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22439027 }} </ref> | ||
* It is not advisable to wait until [[pregnancy]] has begun, since by the time a woman knows she is [[pregnant]], the critical time for the formation of a neural tube defect has usually already passed. A physician may prescribe even higher dosages of [[folic acid]] (4 mg/day) for women who have had a previous pregnancy with a neural tube defect.<ref name="pmidPMID: 22439027">{{cite journal| author=Cavalli P| title=Prevention of Neural Tube Defects and proper folate periconceptional supplementation. | journal=J Prenat Med | year= 2008 | volume= 2 | issue= 4 | pages= 40-1 | pmid=PMID: 22439027 | doi= | pmc=3279093 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22439027 | |||
==References== | ==References== | ||
Latest revision as of 03:36, 23 June 2020
|
WikiDoc Resources for Anencephaly |
|
Articles |
|---|
|
Most recent articles on Anencephaly Most cited articles on Anencephaly |
|
Media |
|
Powerpoint slides on Anencephaly |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Anencephaly at Clinical Trials.gov Clinical Trials on Anencephaly at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Anencephaly
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Anencephaly Discussion groups on Anencephaly Patient Handouts on Anencephaly Directions to Hospitals Treating Anencephaly Risk calculators and risk factors for Anencephaly
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Anencephaly |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ayesha Javid, MBBS[2]
For patient information click here
| Anencephaly | ||
 | ||
|---|---|---|
The side view of the head of an anencephalic fetus.
Source: https://en.wikipedia.org/ | ||
| ICD-10 | Q00.0 | |
| ICD-9 | 740.0 | |
| OMIM | 206500 | |
| DiseasesDB | 705 | |
| MeSH | C10.500.680.196 | |
Overview
Anencephaly is a cephalic disorder in which there is the partial or total absence of the brain. It is an open neural tube defect occurs when the rostral (head) end of the neural tube fails to close resulting in the absence of a major portion of the brain, skull and spinal cord. Children with this disorder are born without a forebrain, the largest part of the brain consisting mainly of the cerebral hemispheres which is responsible for higher cognitive functions and cerebellum which control balance and movement. However, hindbrain is developed. The remaining brain tissue is often exposed - not covered by bone or skin.
Historical Perspective
- Anencephaly was first recognized in the 16th century. In 1989, Aubrey Milunsky and his colleagues observed a reduction in the cases of neural tube defects in the mothers who took folic acid supplements during pregnancy.[1]
- In 1992, Thresa was born with anencephaly. Her parents knew their daughter is going to die. So, they requested if her organs could be used for transplantation. This initiated a debate on anencephalic infant organ donation.[2]
Classification
| Type of Anencephaly | Clinical features |
|---|---|
| Meroanencephaly[3] | Meroanencephaly is a rare form of anencephaly. Fetus born have clinical features including misshapen skull bones and a vascular tissue protuberance called cerebrovasculosa. |
| Holoanencephaly[3] | It is the most common type of anencephaly. In this condition, the entire fetus brain fails to develop except for the brain stem. Usually, infant survives for only one day after birth. |
| Craniorachischisis[4] | It is the most severe type of anencephaly. Along with the cranial defect, fetus also has a defect in the vertebral column exposing the underlying neural tissue. Area cerebrovasculosa and area medullovasculosa fill the areas with cranial and spinal defects. |
Pathophysiology
- By the 3rd week of gestation, the embryo has 3 layers, from outer to inner these layers are ectoderm, mesoderm and endoderm. Notochord in the mesoderm sends signal molecule called Sonic Hedgehog protein to the overlying ectoderm forming it a neuroectoderm.[5]
- The neural plate folds and closes to form a tube-like structure called neural tube and neural crest cells. The neural tube then goes on to form structures of the adult brain.[6]
- A neural tube defect occurs if the the opening of the neural tube, called neuropore, fails to close in the 4th week of gestation. Neural tube has two neuropores, rostral and caudial. Anencephaly results from failure of the rostral neuropore to close anteriorly around day 25.[4]
- The craniofacial abnormalities in anencephaly are caused by abnormal induction by the neural crest cells.[7]
Clinical Features
- Infants born with anencephaly have the following clinical features:[8]
- Facial features: Cleft lip, cleft palate.
- CNS: Absence of bony covering over the back of the head, spina bifida, blindness, deafness.
- GIT: Absence or underdeveloped organs, gastroschisis, omphalocele.
- Genito-urinary system: Hypospadias, penile hypoplasia, renal agenesis.
- Skeletal system: Clubbed foot, clubbed hands.
- Lungs: Diapharagmatic hernia.
Differentiating Anencephalopathy from other Disorders
At times, anencephaly could be misdiagnosed with other similar diagnosis such as;
Epidemiology and Demographics
Incidence
In the United States, approximately 1,000 to 2,000 babies are born with anencephaly each year. In 2001, the National Center for Health Statistics reported 9.4 cases among 100,000 live births.[10] Anually, more than 300,000 babies are born with neural tube defects throughout the world.[11]
Demographics
In United States, the highest prevalence has been seen among the Hispanic [12]. Female babies, whites and children born to mothers who are at extreme of ages are more likely to be affected by the disorder. Worldwide, Ireland and British Islands has higher prevalence as compared to Asia and Africa which has a lower prevalence rate.[13]
Recurrence rate
Like any other neural tube defect, the recurrence rate of anencephaly is 2-4 percent if one sibling is affected and 10 percent if two siblings are affected.[14][15] This familial tendency is due to genetics, environmental factors, or both.[16]
Risk Factors
Folate deficiency
- Studies show that most of the neural tube defects are caused by folic acid deficiency[17].
- This inadequate folate could be due to less oral intake, decreased intestinal absorption, or due to abnormal folate metabolism due to gene mutation. Some drugs antagonize the effect of folic acid resulting in folic acid deficiency and hence NTD. Most important ones are anti-epileptic drugs such as valproic acid and carbamazepine. Also, methotrexate, which is an antineoplastic drug also used for the treatment of ectopic pregnancy, has been linked with increased risk of NTD.[18]
Genetics
Neural tube defects do not follow direct patterns of heredity, though there is some indirect evidence of inheritance.[19] Recent animal models indicate a possible association with deficiencies of the transcription factor TEAD2.[20]
The motivation behind studying genetic patterns is the following:
- NTDs are consistently prevalent among monozygotic twins as compared to dizygotic twins.[21]
- There is a high recurrence rate within families. Statistics show the recurrence risk of 1/20 if one previous pregnancy is affected and 1/10 if two pregnancies are affected in a family.[22]
- There is higher female preponderence as compared to the males. [23]
Syndromes
- Anencephaly is associated with:[24]
- Trisomy 13 or Trisomy 18
- Meckel-Gruber syndrome
- Roberts syndrome
- Jarcho-Levin syndrome
- HARD (hydrocephalus, agyria and retinal dysplasia)
- OEIS complex (omphalocele, exstrophy of the cloaca, imperforate anus and spinal defects)
- Limb-body wall complex (LBWC)
Fever/hyperthermia
- If a pregnant mother’s core body temperature elevates from baseline it could lead to congenital anomalies such neural tube defects, including anencephaly.[25][26]
- The risk is more profound if this happens during the first trimester as this is the time during which organogenesis takes place. The National Birth Defects Prevention Study (NBDPS) infers that the risk of birth defects due to maternal infection-related fever can be reduced by the usage of acetaminophen.[27]
Amniotic bands
- If a pregnant mother develops amniotic bands, it could affect the normal development and growth of the central nervous system. It could result in neural tube defects including anencephaly.[28]
Pregestational diabetes
- If a woman has uncontrolled diabetes mellitus before conception, it could result in neural tube defects including anencephaly.[23]
- Therefore, close monitoring of periconceptional glycemic level is essential to prevent neural tube defects and other congenital anomalies.
Maternal Obesity
- Obesity doubles the risk of neural tube defects. Also, it provides a limitation to fetal imaging.[29]
- Folic acid supplementation does not decrease this risk of NTD, therefore it is mandatory to control weight before conceiving.[30]
Toxins
- Anencephaly and other physical and mental deformities have also been blamed on high exposure to such toxins as lead, chromium, mercury, and nickel. [31]
Natural History, Complications, Prognosis
- Prognosis of children born with anencephaly is extremely poor as there is no cure or standard treatment available so far. Most anencephalic babies do not survive birth, accounting for 55% of non-aborted cases. If the infant is not stillborn, then he or she will usually die within a few hours or days after birth from cardiorespiratory arrest.[32]
- Anencephalic infants are not aggressively resuscitated as there is very little chance of the infant to achieve a full level of consciousness. Instead, clinicians prefer to provide them with adequate hydration, nutrition and comfort.[33] Artificial ventilation, surgery (to fix any co-existing congenital defects), and medications are not considered an option as they have no role in any improvement.[34] Due to this poor prognosis, couple are discussed about the option of the terminating the pregnancy soon after the prenatal diagnosis is established.[35]
Diagnosis
Diagnostic Criteria
- The diagnosis of Anencephaly is made either during a prenatal scan or after the birth.
- In prenatal ultrasound, features like absent calvarium and characteristic frog-like appearance or Micky mouse appearance of the fetus are diagnostic.[36]
- After the birth, clinical features like lack of bony covering over the back of the head and less number of bones around the front and sides of the head are diagnostic.[37]
Symptoms
- Majority of the infants are stillborn or die soon after birth.[38][39]
- Symptoms of anencephaly may include the following:
Physical Examination
- Physical examination may be remarkable for:
- Flattened head
- Absence of the cranial vault[42]
- Positive grasp reflex in both the hands and feet
- Moro reflex could be present or absent depending on the severity of the defect.[43]
- A heart murmur could be present due to associated congenital heart disease.
- cleft lip and/or cleft palate could be present.
- Clubbed foot could be present.
- Gastroschisis, omphalocele, hypospadias could be present in some anencephalic infants.[8]
Laboratory Findings
Alpha-Fetoprotein
- Alpha-fetoprotein (AFP) levels can be measured in maternal serum (MSAFP), amniotic fluid, and fetal plasma.[44]
- Normally, the level rises in early pregnancy, peaks between 10 and 13th week, and then the level declines becoming extremely low near the term.[45]
- For the purpose of prenatal screening, alpha-fetoprotein levels are checked and are found to elevated. This test is non-specific for NTD, as AFP can also be elevated due to other maternal and fetal factors. Therefore, results should always be combined with ultrasound findings and the levels of Acetylcholinesterase (AChE).
Acetylcholinesterase
AChE is an enzyme contained in blood cells, muscle, and nerve tissue. Its levels can be checked from the amniotic fluid via amniocentesis. An elevation of both AFP and AChE values is highly suggestive and accurate for fetal NTD.
Triple screen
Triple screen is a prenatal screening test which includes 3 biomarkers; AFP, hCG and estradiol. It helps to detect certain congenital anomalies, including neural tube defect. The following table shows the triple screening of neural tube defect and how it is differentiated from other anomalies.[46]
| Anomaly | AFP | hCG | Estradiol |
|---|---|---|---|
| NTD | Increased | Normal | Normal |
| Trisomy 21 | Decreased | Increased | Decreased |
| Trisomy 18 | Decreased | Decreased | Decreased |
Imaging Findings
Ultrasound
Ultrasound provides a definitive diagnosis of anencephaly before birth. It can often be diagnosed through a transvaginal ultrasound performed at 12th week postmenstrual.[47]
The ultrasound findings include:
- Absent calvarium.
- No parenchymal tissue above the orbits.
- Reduced crown rump length (CRL)
- A characteristic frog-like appearance or Micky mouse appearance of the fetus due to absent brain and cranial bone and, protruding orbits.
- A large amount of amniotic fluid called polyhydromnios is also seen.[48]
.
Management
Medical Therapy
- There is no known medical therapy available for anencephaly.
Surgery
- At this point in time, there are no surgical options available."Anencephaly: Causes, Symptoms, Diagnosis and Treatment for Newborns | St. Louis Childrens Hospital".
Prevention
- Recent studies have shown that the addition of folic acid to the diet of women of child-bearing age may significantly reduce, although not eliminate, the incidence of neural tube defects. Therefore, it is recommended that all women of child-bearing age consume 0.4 mg of folic acid daily, especially those attempting to conceive or who may possibly conceive, as this can reduce the risk to 0.03%.[49]
- It is not advisable to wait until pregnancy has begun, since by the time a woman knows she is pregnant, the critical time for the formation of a neural tube defect has usually already passed. A physician may prescribe even higher dosages of folic acid (4 mg/day) for women who have had a previous pregnancy with a neural tube defect.[50]
References
- ↑ Milunsky A, Jick H, Jick SS, Bruell CL, MacLaughlin DS, Rothman KJ; et al. (1989). "Multivitamin/folic acid supplementation in early pregnancy reduces the prevalence of neural tube defects". JAMA. 262 (20): 2847–52. doi:10.1001/jama.262.20.2847. PMID 2478730 PMID: 2478730 Check
|pmid=value (help). - ↑ Bard JS (1999). "The diagnosis is anencephaly and the parents ask about organ donation: now what? A guide for hospital counsel and ethics committees". West New Engl Law Rev. 21 (1): 49–95. PMID 12774804 PMID 12774804 Check
|pmid=value (help). - ↑ 3.0 3.1 Isada NB, Qureshi F, Jacques SM, Holzgreve W, Tout MJ, Johnson MP; et al. (1993). "Meroanencephaly: pathology and prenatal diagnosis". Fetal Diagn Ther. 8 (6): 423–8. doi:10.1159/000263862. PMID 8286034 PMID 8286034 Check
|pmid=value (help). - ↑ 4.0 4.1 Greene ND, Copp AJ (2014). "Neural tube defects". Annu Rev Neurosci. 37: 221–42. doi:10.1146/annurev-neuro-062012-170354. PMC 4486472. PMID 25032496 PMID: 25032496 Check
|pmid=value (help). - ↑ Neuroectoderm becomes a neural plate."Embryology, Neural Tube - StatPearls - NCBI Bookshelf".
- ↑ Sadler, T. W. (2006). Langman's medical embryology. Philadelphia: Lippincott Williams & Wilkins. ISBN 9780781794855.
- ↑ Sarnat HB, Flores-Sarnat L (2005). "Embryology of the neural crest: its inductive role in the neurocutaneous syndromes". J Child Neurol. 20 (8): 637–43. doi:10.1177/08830738050200080101. PMID 16225807 PMID 16225807 Check
|pmid=value (help). - ↑ 8.0 8.1 Gole RA, Meshram PM, Hattangdi SS (2014). "Anencephaly and its associated malformations". J Clin Diagn Res. 8 (9): AC07–9. doi:10.7860/JCDR/2014/10402.4885. PMC 4225866. PMID 25386414 PMID: 25386414 Check
|pmid=value (help). - ↑ "Anencephaly | Psychology Wiki | Fandom".a
- ↑ Mathews TJ, Honein MA, Erickson JD (2002). "Spina bifida and anencephaly prevalence--United States, 1991-2001". MMWR Recomm Rep. 51 (RR-13): 9–11. PMID 12353510 PMID: 12353510 Check
|pmid=value (help). - ↑ "Health Dimensions of Sex and Reproduction — Christopher J. L. Murray, Alan D. Lopez | Harvard University Press".
- ↑ population."Folic Acid & Neural Tube Defects: Data & Statistics | CDC".
- ↑ Frey L, Hauser WA (2003). "Epidemiology of neural tube defects". Epilepsia. 44 Suppl 3: 4–13. doi:10.1046/j.1528-1157.44.s3.2.x. PMID 12790881.
- ↑ Cowchock S, Ainbender E, Prescott G, Crandall B, Lau L, Heller R; et al. (1980). "The recurrence risk for neural tube defects in the United States: a collaborative study". Am J Med Genet. 5 (3): 309–14. doi:10.1002/ajmg.1320050314. PMID 7405962 PMID: 7405962 Check
|pmid=value (help). - ↑ Toriello HV, Higgins JV (1983). "Occurrence of neural tube defects among first-, second-, and third-degree relatives of probands: results of a United States study". Am J Med Genet. 15 (4): 601–6. doi:10.1002/ajmg.1320150409. PMID 6614048 PMID: 6614048 Check
|pmid=value (help). - ↑ Copp AJ, Greene ND (2010). "Genetics and development of neural tube defects". J Pathol. 220 (2): 217–30. doi:10.1002/path.2643. PMC 4239538. PMID 19918803 PMID: 19918803 Check
|pmid=value (help). - ↑ Copp AJ, Stanier P, Greene ND (2013). "Neural tube defects: recent advances, unsolved questions, and controversies". Lancet Neurol. 12 (8): 799–810. doi:10.1016/S1474-4422(13)70110-8. PMC 4023229. PMID 23790957 PMID: 23790957 Check
|pmid=value (help). - ↑ Wen SW, Walker M (2004). "Risk of fetal exposure to folic acid antagonists". J Obstet Gynaecol Can. 26 (5): 475–80. doi:10.1016/s1701-2163(16)30658-2. PMID 15151734 PMID: 15151734 Check
|pmid=value (help). - ↑ Shaffer LG, Marazita ML, Bodurtha J, Newlin A, Nance WE (1990). "Evidence for a major gene in familial anencephaly". Am. J. Med. Genet. 36 (1): 97–101. doi:10.1002/ajmg.1320360119. PMID 2333913.
- ↑ Kaneko KJ, Kohn MJ, Liu C, Depamphilis ML (2007). "Transcription factor TEAD2 is involved in neural tube closure". Genesis. 45 (9): 577–87. doi:10.1002/dvg.20330. PMID 17868131.
- ↑ Windham GC, Bjerkedal T, Sever LE (1982). "The association of twinning and neural tube defects: studies in Los Angeles, California, and Norway". Acta Genet Med Gemellol (Roma). 31 (3–4): 165–72. doi:10.1017/s0001566000008254. PMID 6763438 PMID: 6763438 Check
|pmid=value (help). - ↑ Ross ME, Mason CE, Finnell RH (2017). "Genomic approaches to the assessment of human spina bifida risk". Birth Defects Res. 109 (2): 120–128. doi:10.1002/bdra.23592. PMC 5388593. PMID 27883265 PMID: 27883265 Check
|pmid=value (help). - ↑ 23.0 23.1 Deak KL, Siegel DG, George TM, Gregory S, Ashley-Koch A, Speer MC; et al. (2008). "Further evidence for a maternal genetic effect and a sex-influenced effect contributing to risk for human neural tube defects". Birth Defects Res A Clin Mol Teratol. 82 (10): 662–9. doi:10.1002/bdra.20511. PMC 2981339. PMID 18937341 PMID: 18937341 Check
|pmid=value (help). - ↑ Phadke S, Agarwal M (2012). "Neural tube defects: A need for population-based prevention program". Indian J Hum Genet. 18 (2): 145–7. doi:10.4103/0971-6866.100747. PMC 3491283. PMID 23162285 PMID: 23162285 Check
|pmid=value (help). - ↑ Li DK, Janevic T, Odouli R, Liu L (2003). "Hot tub use during pregnancy and the risk of miscarriage". Am J Epidemiol. 158 (10): 931–7. doi:10.1093/aje/kwg243. PMID 14607798 PMID: 14607798 Check
|pmid=value (help). - ↑ Edwards MJ (2006). "Review: Hyperthermia and fever during pregnancy". Birth Defects Res A Clin Mol Teratol. 76 (7): 507–16. doi:10.1002/bdra.20277. PMID 16933304 PMID: 16933304 Check
|pmid=value (help). - ↑ Feldkamp ML, Meyer RE, Krikov S, Botto LD (2010). "Acetaminophen use in pregnancy and risk of birth defects: findings from the National Birth Defects Prevention Study". Obstet Gynecol. 115 (1): 109–15. doi:10.1097/AOG.0b013e3181c52616. PMID 20027042 .PMID: 20027042 Check
|pmid=value (help). - ↑ "StatPearls". 2020. PMID 32310363 Check
|pmid=value (help). - ↑ Sukanya S, Bay BH, Tay SS, Dheen ST (2012). "Frontiers in research on maternal diabetes-induced neural tube defects: Past, present and future". World J Diabetes. 3 (12): 196–200. doi:10.4239/wjd.v3.i12.196. PMC 3538985. PMID 23301121 PMID: 23301121 Check
|pmid=value (help). - ↑ Moussa, Hind N; Hosseini Nasab, Susan; Haidar, Ziad A; Blackwell, Sean C; Sibai, Baha M (2016). "Folic acid supplementation: what is new? Fetal, obstetric, long-term benefits and risks". Future Science OA. 2 (2). doi:10.4155/fsoa-2015-0015. ISSN 2056-5623.
- ↑ Goldsmith, Alexander (1996, quoted by Millen and Holtz, "Dying for Growth")
- ↑ "Applications of Mass Spectrometry in Life Safety | SpringerLink".
- ↑ "Anencephaly | Psychology Wiki | Fandom".
- ↑ "Anencephaly: Causes, Symptoms, Diagnosis and Treatment for Newborns | St. Louis Childrens Hospital".
- ↑ Machado IN, Martinez SD, Barini R (2012). "Anencephaly: do the pregnancy and maternal characteristics impact the pregnancy outcome?". ISRN Obstet Gynecol. 2012: 127490. doi:10.5402/2012/127490. PMC 3302112. PMID 22462001 PMID: 22462001 Check
|pmid=value (help). - ↑ "Anencephaly | Radiology Reference Article | Radiopaedia.org".
- ↑ "Anencephaly | Symptoms & Causes | Boston Children's Hospital".
- ↑ "Facts about Anencephaly | CDC".
- ↑ Jaquier M, Klein A, Boltshauser E (2006). "Spontaneous pregnancy outcome after prenatal diagnosis of anencephaly". BJOG. 113 (8): 951–3. doi:10.1111/j.1471-0528.2006.01014.x. PMID 16827827 PMID: 16827827 Check
|pmid=value (help). - ↑ Murphy PA (1994). "Nursing the permanently unconscious". Trends Health Care Law Ethics. 9 (1): 33–6. PMID 7950143 PMID: 7950143 Check
|pmid=value (help). - ↑ "Cephalic Disorders Fact Sheet | National Institute of Neurological Disorders and Stroke".
- ↑ "Anencephaly: Overview, Pathophysiology, Causes".
- ↑ Futagi Y, Toribe Y, Suzuki Y (2012). "The grasp reflex and moro reflex in infants: hierarchy of primitive reflex responses". Int J Pediatr. 2012: 191562. doi:10.1155/2012/191562. PMC 3384944. PMID 22778756 PMID: 22778756 Check
|pmid=value (help). - ↑ "StatPearls". 2020. PMID 28613501 PMID 28613501 Check
|pmid=value (help). - ↑ Gitlin D, Perricelli A, Gitlin GM (1972). "Synthesis of -fetoprotein by liver, yolk sac, and gastrointestinal tract of the human conceptus". Cancer Res. 32 (5): 979–82. PMID 4111729 PMID 4111729 Check
|pmid=value (help). - ↑ "Triple Screening in Pregnancy--What It Is and What to Expect - American Family Physician".
- ↑ Johnson SP, Sebire NJ, Snijders RJ, Tunkel S, Nicolaides KH (1997). "Ultrasound screening for anencephaly at 10-14 weeks of gestation". Ultrasound Obstet Gynecol. 9 (1): 14–6. doi:10.1046/j.1469-0705.1997.09010014.x. PMID 9060123 PMID: 9060123 Check
|pmid=value (help). - ↑ "Anencephaly | Radiology Reference Article | Radiopaedia.org".
- ↑ Template:NINDS
- ↑ Cavalli P (2008). "Prevention of Neural Tube Defects and proper folate periconceptional supplementation". J Prenat Med. 2 (4): 40–1. PMC 3279093. PMID 22439027 PMID: 22439027 Check
|pmid=value (help).
Template:Congenital malformations and deformations of nervous system
de:Anenzephalie it:Anencefalia he:אננצפלוס nl:Anencefalie fi:Aivottomuus sv:Anencefali