Androgen insensitivity syndrome pathophysiology
|
Androgen insensitivity syndrome Microchapters |
|
Differentiating Androgen insensitivity syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Androgen insensitivity syndrome pathophysiology On the Web |
|
American Roentgen Ray Society Images of Androgen insensitivity syndrome pathophysiology |
|
Directions to Hospitals Treating Androgen insensitivity syndrome |
|
Risk calculators and risk factors for Androgen insensitivity syndrome pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Pathophysiology
Androgen insensitivity syndrome results from mutations of the gene encoding the androgen receptor. It has also been called androgen resistance in the medical literature. The nature of the resulting problem varies according to the structure and sensitivity of the abnormal receptor. Most of the forms of AIS involve variable degrees of undervirilization and/or infertility in XY persons of either sex. A woman with complete androgen insensitivity syndrome (CAIS) has a nearly normal female body despite a 46XY karyotype and undescended testes, a condition termed testicular feminization in the past.
Major changes in the understanding and management of the various forms of AIS have occurred since 1990. Laboratory research has greatly expanded our understanding of the molecular mechanisms of the clinical features, including a rare neuromuscular disorder. More importantly, patient advocacy groups for AIS and other intersex conditions have increased public awareness of these disorders, helped revise the understanding of gender identity, emphasized the value of accurate and sophisticated information for patients, and induced physicians to re-evaluate the effectiveness of the surgical corrections attempted in past decades. Surgery is increasingly seen as an elective option even for the more ambiguous conditions.
Normal function of androgens and the androgen receptor [2]
Understanding the effects of androgen insensitivity begins with an understanding of the normal effects of testosterone in male and female development. The principal mammalian androgens are testosterone and its more potent metabolite, dihydrotestosterone (DHT).
The androgen receptor (AR) is a large protein of at least 910 amino acids. Each molecule consists of a portion which binds the androgen, a zinc finger portion that binds to DNA in steroid sensitive areas of nuclear chromatin, and an area that controls transcription.
Testosterone diffuses from the circulation into the cytoplasm of a target cell. Some is metabolized to estradiol, some reduced to DHT, and some remains as testosterone (T). Both T and DHT can bind and activate the androgen receptor, though DHT does so with more potent and prolonged effect. As DHT (or T) binds to the receptor, a portion of the protein is cleaved. The AR-DHT combination dimerizes by combining with a second AR-DHT, both are phosphorylated, and the entire complex moves into the cell nucleus and binds to androgen response elements on the promoter region of androgen-sensitive target genes. The transcription effect is amplified or inhibited by coactivators or corepressors.
Although testosterone can be produced directly and indirectly from ovaries and adrenals later in life, the primary source of testosterone in early fetal life is the testes, and it plays a major role in human sexual differentiation. Before birth, testosterone induces the primary sex characteristics of males. At puberty, testosterone is primarily responsible for the secondary sex characteristics of males.
- See Testosterone article for fuller discussion of androgen sources and the role of testosterone in normal human development.
- See Sexual differentiation for a brief but fuller overview of human sexual differentiation and biological sex differences.
Prenatal effects of testosterone in 46,XY fetus
In a normal fetus with a 46,XY karyotype, the presence of the SRY gene induces testes to form on the genital ridges in the fetal abdomen a few weeks after conception. By 6 weeks of gestation, genital anatomies of XY and XX fetuses are still indistinguishable, consisting of a tiny underdeveloped button of tissue able to become a phallus, and a urogenital midline opening flanked by folds of skin able to become either labia or scrotum. By the 7th week, fetal testes begin to produce testosterone and release it into the blood.
Directly and as DHT, testosterone acts on the skin and tissues of the genital area and by 12 weeks of gestation, has produced a recognizable male, with a growing penis with a urethral opening at the tip, and a perineum fused and thinned into a scrotum, ready for the testes. Evidence suggests that this "remodelling" of the genitalia can only occur during this period of fetal life; if not complete by about 13 weeks, no amount of testosterone later will move the urethral opening or close a vagina-like opening.
For the remainder of gestation, the principal known effect of testosterone and DHT is continued growth of the penis and internal wolffian derivatives (part of prostate, epididymis, seminal vesicles, and vas deferens).
Early postnatal effects of testosterone in 46,XY infants
Testosterone levels are low at birth but rise within weeks, remaining at normal male pubertal levels for about 2 months before declining to the low, barely detectable childhood levels. The biological function of this rise is unknown. Animal research suggests a contribution to brain differentiation.
Pubertal effects of testosterone in 46,XY children
At puberty, many of the early physical changes in both sexes are androgenic (adult-type body odor, increased oiliness of skin and hair, acne, pubic hair, axillary hair, fine upper lip and sideburn hair).
As puberty progresses, later secondary sex characteristics in males are nearly entirely due to androgens (continued growth of the penis, maturation of spermatogenic tissue and fertility, beard, deeper voice, masculine jaw and musculature, body hair, heavier bones). In males, the major pubertal changes attributable to estradiol are growth acceleration, epiphyseal closure, termination of growth, and (if it occurs) gynecomastia.
Genetics
Because the Androgen Insensitivity Syndrome gives rise to ambiguity between the genetic and the phenotypic gender, we will use the convention 46,XY to designate a genotypic male, and 46,XX to designate a genotypic female. By this convention, a person with Androgen Insensitivity Syndrome is a 46,XY but a phenotypic female.
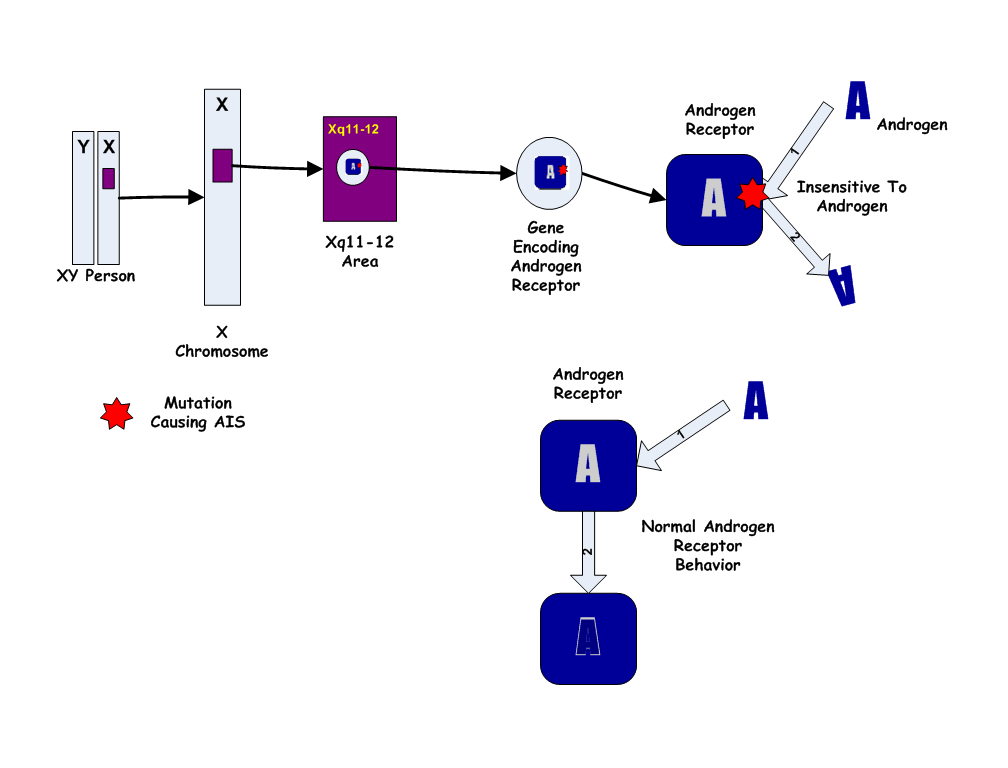
The Androgen Insensitivity Syndrome has been linked to mutations in AR, the gene for the human Androgen Receptor, located at Xq11-12 (i.e. on the X chromosome). Thus, it is an X-linked recessive trait, causing minimal or no effects in 46,XX people.

However, 46,XX women with a single mutated copy of the AR gene can be "carriers" of AIS, and their 46,XY children (male) will have a 50% chance of having the syndrome. As in some other X-linked recessive conditions, carrier mothers may display some minor traits of the condition: AIS carriers often have reduced axillary and pubic hair, and reduced normal adolescent acne.
Except in the rare instance of a new mutation, a person affected with AIS has inherited his/her single X chromosome with the defective gene from his/her mother, who may have an affected sibling. Generally the condition caused by a familial mutation will affect family members similarly, though differing degrees of severity occasionally occur in different relatives with apparently the same mutation. Carrier testing is now available for relatives at risk when a diagnosis of AIS is made in a family member.
Over 100 AR mutations causing various forms of AIS have been reported. In general, the milder types of AIS (4 and 5 in the list below) are caused by simple missense mutations with single codon/single amino acid difference, while CAIS and the nearly complete forms result from mutations that more severely affect the shape and structure of the protein. About one third of cases of AIS are new mutations rather than familial. A single case of CAIS attributed to an abnormality of the AF-1 coactivator (rather than AR itself) has been reported (OMIM 300274).
1. Complete AIS
People with CAIS are girls or women with internal testes, 46,XY karyotypes, and normal female bodies by external appearance except for some exceptions. The vagina is not as deep, and there are no ovaries or uterus— hence no menses or fertility. Gender identity is almost always female.
2. Incomplete or partial AIS
As with CAIS, girls and women with PAIS also have a 46,XY karyotype, testes, and a female body lacking a uterus, ovaries and full vagina. However, the mutations associated with PAIS do not entirely eliminate all responsiveness to androgens, and mild testosterone effects occur.
The most obvious testosterone effect seen in PAIS is pubic and axillary hair, which are usually normal. The clitoris may be enlarged, and the labia partially fused, though these features are usually not pronounced enough to cause noticeable ambiguity of the genitalia at birth, or may be subtle enough to be ascribed to normal anatomic variation. Internally, traces of undeveloped wolffian structures (epididymis, vas deferens, seminal vesicles, ejaculatory ducts) may be present.
3. Reifenstein syndrome
Androgen receptor mutations associated with more intermediate degrees of androgen responsiveness can result in more intermediate degrees of masculinization before birth and obvious ambiguity of the genitalia. Of the five clinical forms of AIS described here, this is the only one likely to result in uncertainty about a baby's sex at birth, and the most likely to be diagnosed in infancy.
The testes of a 46,XY fetus produce AMH and testosterone. In Reifenstein syndrome, as in CAIS, PAIS, and normal males, the AMH suppresses development of a uterus, fallopian tubes, and upper vagina. However, unlike CAIS and PAIS, fetal testosterone has a significant effect on the external genitalia, producing a phallus smaller than a typical penis but larger than a typical clitoris.
This most obvious birth defect, somewhat midway between male and female, nearly always leads to referral to a pediatric endocrinologist and a full genetic, anatomic, and hormonal evaluation.
4. Infertile male syndrome
Androgen receptor mutations have also been discovered in men with normal internal and external genitalia but infertility due to absence of sperm (azoospermia). Androgenic body hair is normal and gynecomastia uncommon. Some have mildly elevated testosterone and LH levels but this is not invariable. Several surveys suggest that androgen receptor mutations can be found in 30-40% of men with infertility due to otherwise unexplained oligospermia or azoospermia. AIS may also explain most cases of a rarer form of male infertility, the Del Castillo or Sertoli-cell-only syndrome.
5. Undervirilized fertile male syndrome
Some AR mutations with mildly reduced sensitivity cause mild undervirilization. These men have normally formed internal and external genitalia but a small penis. Androgenic body hair may be sparser than unaffected relatives. Ejaculate volume may be reduced, though sperm density is normal. Few examples of this variant of AIS have been reported, but unlike the previously listed phenotypes, many of these men are fertile.
6. X-linked spinal and bulbar atrophy syndrome
Kennedy disease is an X-linked spinal-bulbar muscle atrophy syndrome associated with mutations of the androgen receptor. Like the other forms of AIS described above, it affects only males. The distinctive AR mutation of Kennedy disease, reported in 1991, involves multiplied CAG repeats in the first exon. The mechanism by which this type of mutation causes neuromuscular disease, while complete insensitivity does not, is not yet understood.
Since the neuromuscular disease was first described in 1968 many kindreds have been reported. Ages of onset and severity of manifestations in affected males vary from adolescence to old age, but most commonly develop in middle adult life. Early signs often include weakness of tongue and mouth muscles, fasciculations, and gradually increasing weakness of proximal limb muscles. In some cases, premature muscle exhaustion began in adolescence. Neuromuscular management is supportive, and the disease progresses very slowly and often does not lead to extreme disability.
Endocrine manifestations of this disorder are variable and only rarely include undervirilization of internal or external genitalia. In the majority evidence of altered androgen sensitivity is restricted to exaggerated or persistent adolescent gynecomastia, and the mildly high LH, testosterone, and estradiol levels characteristic of other forms of AIS. In other words, most people affected with Kennedy disease are relatively normal XY men with normal fertility and normal or minimally reduced virilization.