Mitral regurgitation resident survival guide
|
Mitral Regurgitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Mitral regurgitation resident survival guide On the Web |
|
American Roentgen Ray Society Images of Mitral regurgitation resident survival guide |
|
Risk calculators and risk factors for Mitral regurgitation resident survival guide |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2]
Overview
Unlike mitral stenosis or aortic stenosis where one waits on symptoms as an indication for valve replacement, mitral valve repair or replacement is preferably undertaken before the development of symptoms.
Why the Mitral valve is replaced Before Symptoms in Patients with Chronic Mitral Regurgitation
- Mitral regurgitation is a syndrome of pure volume overload whereas aortic regurgitation is a combination of both volume and pressure overload.
- Both syndromes are associated with an increase in preload.
- in mitral regurgitation, the afterload is reduced whereas in aortic regurgitation the afterload is increased. This is very important because when the mitral valve is repaired, there is no longer a reduction afterload and the left ventricle may fail due to an abrupt rise in the afterload. In aortic regurgitation, because the afterload is already increased chronically, replacement of the valve is not as likely to precipitate acute left ventricular failure due to an abrupt rise in afterload.
Diagnosis
Symptoms
- Acute miral regurgitation causes the following symptoms:
- Chronic mitral regurgitation may have a prolonged asymptomatic interval phase until the heart decompensates and the symptoms of low cardiac output and pulmonary congestion start. By the time the symptoms develop, left ventricular dysfunction may have already occurred.
Physical Examination
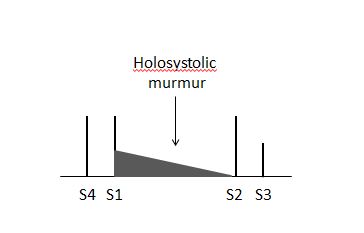
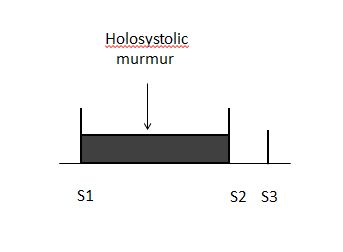
- S3 and S4 may be heard on auscultation.
- A holosystolic murmur is heard in the apical region of the heart. MR murmur radiates to the axillary region. It may be soft, short and even absent. 70% of the cases of papillary muscle rupture have no murmur.
 |
 |
Imaging
Transthoracic echocardiography
- Echocardiographic findings reflecting the severity of the mitral regurgitation include:
- Regurgitant volume >60 ml
- Regurgitant fraction >55%
- Effective regurgitant orifice (ERO) (ratio of regurgitant flow volume to the velocity of the mitral insufficiency jet: ERO = Flow / Velocity) >0.4 cm2
- If the left ventricular and left atrial sizes are normal on echocardiography, mitral regurgitation is not severe.
- Central jets indicate normal mitral valve and therefore not severe.
- Wide eccentric jets indicate that the regurgitation is severe.
- Echocardiographic findings must match the symptoms.
- If the TTE is negative, transesophageal echocardiography (TEE) or cardiac catheterization are the preferred diagnostic imaging modalities. TTE can underestimate the clinical picture in patients with clinical signs of severe and mild MR. In cases of any discrepancy in the results of different modalities, it is recommended to do a left ventriculogram.
Treatment
Acute severe Mitral regurgitation
- Treatment of acute severe mitral regurgitation depends on the stability of the patient.If the patient is clinically stable, the treatment options are:
- IV vasodilators, diuretics, antibiotics, anti-ischemic agents
- Surgery is preferred in the following cases:
- Endocarditis with progressive congestive heart failure
- No response to antibiotics
- Abscess formation
- Recurrent embolization
- If the patient is clinically unstable , the treatment options are:
- IV nitroprusside is used to maintain blood pressure. Ionotropes are added when needed.
- If medical therapy is not effective, an intra aortic balloon pump can be inserted to maintain hemodynamic stability.
- Surgical treatment is usually indicated.
- Knowledge of the etiology of the mitral regurgitation is important to know if the valve can be repaired or replaced.
Chronic Mitral regurgitation
- By the time symptoms develop, there is already left ventricular dysfunction.
- Because of the low pressure system into which the blood is ejected into through the mitral valve, the ejection fraction is always high in mitral regurgitation. If the ejection fraction appears to be "normal", there is already decline in left ventricular function.
- There is no indication for vasodilator therapy in the absence of systemic hypertension in asymptomatic patients with preserved left ventricular function.
Indications for surgery in Mitral regurgitation
- The indications for surgery in mitral regurgitation are:
- Any symptoms - this is unlike mitral stenosis where surgeons operate on the heart when patients have class III or IV symptoms.
- Severe organic MR.
- Left ventricular dysfunction - ejection fraction <60% and end systolic diameter >40 mm2.
- Surgery can be considered in asymptomatic patients in the following cases:
- Truly severe MR
- Low operative mortality
- High chance of successful repair (e.g: posterior leaflet - MVP)
- Pre-operative ejection fraction has a prognostic impact in patients who undergo mitral valve repair or replacement. The lower the ejection fraction is, the higher the mortality is.