Mitral regurgitation resident survival guide
|
Mitral Regurgitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Mitral regurgitation resident survival guide On the Web |
|
American Roentgen Ray Society Images of Mitral regurgitation resident survival guide |
|
Risk calculators and risk factors for Mitral regurgitation resident survival guide |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2]
Overview
Mitral regurgitation is a disorder of the heart valve that is present between the left atrium and left ventricle. Mitral regurgitation is characterized by the incompetence of the mitral valve which fails to completely close during systole. Hence, when the left ventricle contracts and pumps blood into the aorta, a certain amount of blood leaks from the left ventricle into the left atrium (dual outlet left ventricle).
Classification
Mitral regurgitation can be acute or chronic. Acute mitral regurgitation causes sudden overload on left atrium and left ventricle and can cause pulmonary congestion. Chronic regurgitation develops over a period of months to years during which the left ventricle undergoes eccentric hypertrophy as a compensatory mechanism for the pressure changes in the heart. Long standing volume overload on the left ventricle results in the inability of the left ventricle to compensate beyond a certain extent and thus leads to left ventricular dysfunction.
Causes
Mitral regurgitation (MR) can be caused either by intrinsic defects in the mitral valve or by defects in the ventricle.
- Defects in the mitral valve:
- Degeneration
- Chordal rupture
- Defects in the ventricle (otherwise called secondary or functional MR):

Differentiating Mitral regurgitation from Aortic regurgitation

Natural History and Prognosis
Natural History
The natural history of mitral regurgitation is dictated by the underlying etiology.
- Papillary muscle rupture and deihisced mitral valve prosthesis - there is poor prognosis without surgery.
- Endocarditis - the natural history and progression of mitral regurgitation depends on the response to the antibiotics.
Prognosis
- Effective regurgitant orifice (ERO) area is a good prognostic indicator of the severity of the MR and the survival. The mortality risk is related directly to the degree of ERO. The higher the area is, the lower the survival is.
- Untreated severe MR has a poor prognosis.
Diagnosis
Symptoms
- Acute miral regurgitation causes the following symptoms:
- Chronic mitral regurgitation may have a prolonged asymptomatic interval phase until the heart decompensates and the symptoms of low cardiac output and pulmonary congestion start. By the time symptoms develop, left ventricular dysfunction may have already occurred.
Physical Examination
- S3 and S4 may be heard on auscultation.
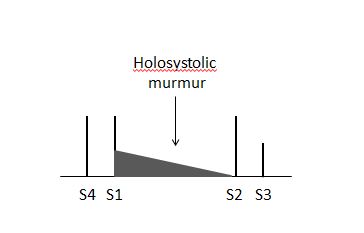
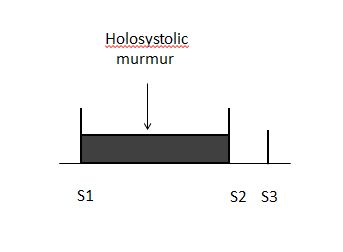
- A holosystolic murmur is heard in the apex region of the heart and radiating to the axilla. MR murmur may be soft, short and even absent. 70% papillary muscle rupture cases have no murmur.
 |
 |
Imaging
Transthoracic echocardiography
Echocardiographic findings reflecting the severity of the mitral regurgitation include:
- Regurgitant volume - (>60 ml)
- Regurgitant fraction - (>55%)
- Effective regurgitant orifice (ERO) (ratio of regurgitant flow volume to the velocity of the mitral insufficiency jet (ERO = Flow / Velocity)) - (>0.4 cm2)
All the three factors mentioned above are better parameters to quantify severity than color jet area.
- If the left ventricular and left atrial sizes are normal on an ECHO mitral regurgitation is not severe.
- Central jets indicate normal mitral valve and therefore not severe.
- Wide eccentric jets indicate that the regurgitation is severe.
Echocardiographic findings must match the symptoms.
If the TTE is negative transesophageal echocardiography (TEE) or cardiac catheterization are the preferred diagnostic imaging modalities. TTE can underestimate the clinical picture in patients with clinical signs of severe and mild MR. In case of any discrepancy in the results of different modalities, it is recommended to do a left ventriculogram.
Treatment
Acute severe Mitral regurgitation
Treatment of acute severe mitral regurgitation depends on the stability of the patient. If the patient is clinically stable, the treatment options are:
- IV vasodilators, diuretics, antibiotics, anti-ischemic agents
- Surgery is preferred in the following cases:
- Endocarditis with progressive congestive heart failure
- No response to antibiotics
- Abscess formation
- Recurrent embolization
If the patient is clinically unstable , the treatment options are:
- IV nitroprusside to maintain blood pressure. Ionotropes are added when needed.
- If medical therapy is not effective, an intra aortic balloon pump can be inserted to maintain hemodynamic stability.
- Surgical treatment is usually indicated.
- Knowledge of the etiology of the mitral regurgitation is important to know if the valve can be repaired or replaced.
Chronic Mitral regurgitation
- There is no indication for vasodilator therapy in the absence of systemic hypertension in asymptomatic patients with preserved left ventricular function .
Indications for surgery in Mitral regurgitation
- Any symptoms - this is unlike mitral stenosis where surgeons operate on the heart when patients have class III or IV symptoms.
- Severe organic MR.
- Left ventricular dysfunction - ejection fraction <60% and end systolic diameter >40 mm2.
- Surgery can be considered in asymptomatic patients in the following cases:
- Truly severe MR
- Low operative mortality
- High chance of successful repair (e.g: posterior leaflet - MVP)
Pre-operative ejection fraction has a prognostic impact in patients who undergo mitral valve repair or replacement. The lower the ejection fraction is, the higher the mortality is.