Pulmonary embolism medical therapy
|
Pulmonary Embolism Microchapters |
|
Diagnosis |
|---|
|
Pulmonary Embolism Assessment of Probability of Subsequent VTE and Risk Scores |
|
Treatment |
|
Follow-Up |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Pulmonary embolism medical therapy On the Web |
|
Directions to Hospitals Treating Pulmonary embolism medical therapy |
|
Risk calculators and risk factors for Pulmonary embolism medical therapy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editors-in-Chief: Ujjwal Rastogi, MBBS [2]
Overview
In most cases, anticoagulant therapy is the mainstay of treatment. Acutely, supportive treatments, such as oxygen or analgesia, are often required.
Massive PE causing hemodynamic instability (marked decreased oxygen saturation, tachycardia and/or hypotension) is an indication for thrombolysis, the enzymatic destruction of the clot with medication. Some advocate, the usage of thrombolytic, if right ventricular dysfunction is demonstrated on echocardiography.[1]
Anticoagulation
- Salient Features:
- Prevent further clot formation, so should be started as early as possible.
- It has no effect on pre-existing clot lysis.
- It has no effect in decreasing the size of thrombus.
- In most cases, anticoagulant therapy is the mainstay of treatment. It includes Heparin, Low molecular weight heparins (such as enoxaparin and dalteparin), or Factor Xa inhibitors (fondaparinux). These are administered initially, while Warfarin therapy is commenced (this may take several days, usually while the patient is in hospital).
Warfarin therapy often requires frequent dose adjustment and monitoring of the INR. In PE, INRs between 2.0 and 3.0 are generally considered ideal.
If another episode of PE occurs under warfarin treatment
- The INR window may be increased to e.g. 2.5-3.5 (unless there are contraindications) or
- Anticoagulation may be changed to a different anticoagulant e.g. low molecular weight heparin.
In patients with an underlying malignancy, low molecular weight heparin is favored over warfarin based on the results of the CLOT trial.[2]
Similarly, pregnant women are often maintained on low molecular weight heparin to avoid the known teratogenic effects of warfarin.
Warfarin therapy is usually continued for 3-6 months, or "lifelong" if there have been previous DVTs or PEs, or none of the usual risk factors is present. An abnormal D-dimer level at the end of treatment might signal the need for continued treatment among patients with a first unprovoked pulmonary embolus.[3]
Inferior vena cava filter
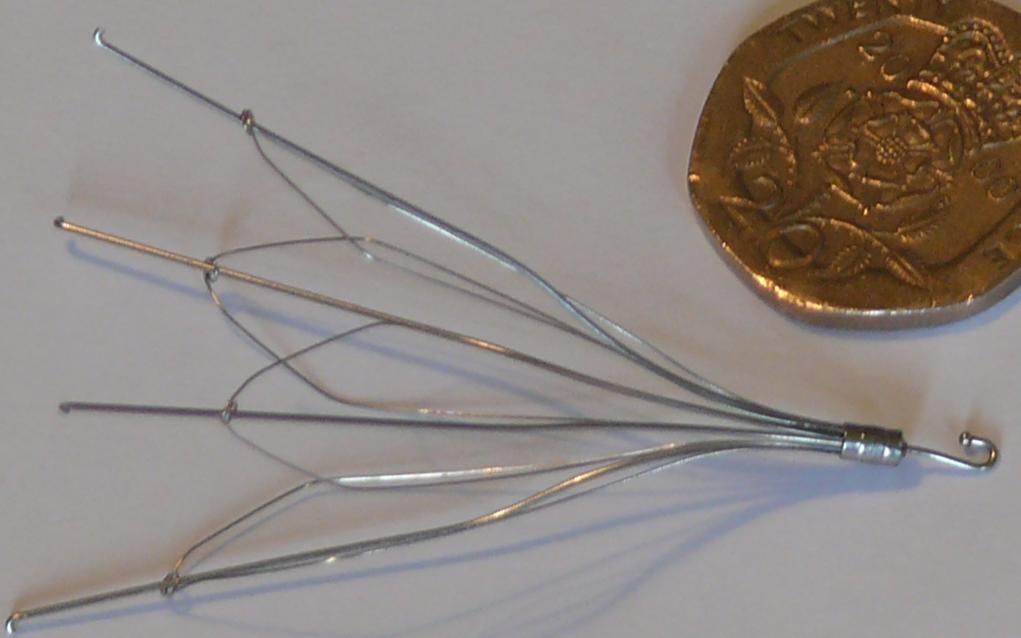
If anticoagulant therapy is contraindicated and/or ineffective an inferior vena cava filter may be implanted.[4]
Thrombolysis
Thrombolysis can be given for severe PEs when surgery is not immediately available or possible (e.g. periarrest or during cardiac arrest). The only trial that addressed this issue had 8 patients; the four receiving thrombolysis survived, while the four who received only heparin died.[5]
The use of thrombolysis in moderate PEs is still debatable. The aim of the therapy is to dissolve the clot, but there is an attendant risk of bleeding or stroke.[6]
References
- ↑ Goldhaber SZ. Pulmonary embolism. Lancet 2004;363:1295-305. PMID 15094276.
- ↑ Lee AY, Levine MN, Baker RI, Bowden C, Kakkar AK, Prins M, Rickles FR, Julian JA, Haley S, Kovacs MJ, Gent M (2003). "Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer". N Engl J Med. 349 (2): 146–53. PMID 12853587.
- ↑ Palareti G, Cosmi B, Legnani C; et al. (2006). "D-dimer testing to determine the duration of anticoagulation therapy". N. Engl. J. Med. 355 (17): 1780–9. doi:10.1056/NEJMoa054444. PMID 17065639.
- ↑ Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, Laporte S, Faivre R, Charbonnier B, Barral F, Huet Y, Simonneau G (1998). "A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group". N Engl J Med. 338 (7): 409–15. PMID 9459643.
- ↑ Jerjes-Sanchez C, Ramirez-Rivera A, de Lourdes Garcia M, Arriaga-Nava R, Valencia S, Rosado-Buzzo A, Pierzo JA, Rosas E. Streptokinase and Heparin versus Heparin Alone in Massive Pulmonary Embolism: A Randomized Controlled Trial. J Thromb Thrombolysis 1995;2:227-229. PMID 10608028.
- ↑ Dong B, Jirong Y, Liu G, Wang Q, Wu T. Thrombolytic therapy for pulmonary embolism. Cochrane Database Syst Rev 2006;(2):CD004437. PMID 16625603.