Tricuspid atresia pathophysiology
|
Tricuspid atresia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenarios |
|
Case Studies |
|
Tricuspid atresia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Tricuspid atresia pathophysiology |
|
Risk calculators and risk factors for Tricuspid atresia pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Keri Shafer, M.D. [2] Priyamvada Singh, MBBS [3]; Assistant Editor-In-Chief: Kristin Feeney, B.S. [4]
Historical perspective
Tricuspid atresia was first discovered by friedrich ludwig kreysig in 1817, a German physician who found the obstruction between right atrium and right ventricle in the autopsy of cyanotic infants. .
The classic term of tricuspid atresia was used firstly by schuberg in 1861.
Pathophysiology
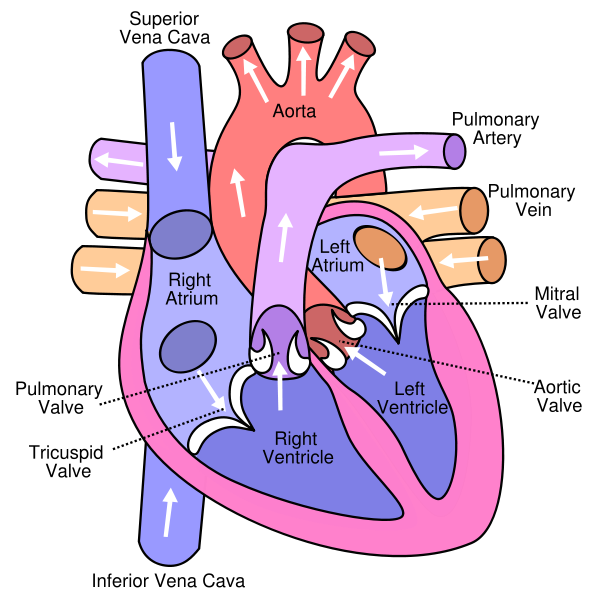
Normal Human Heart
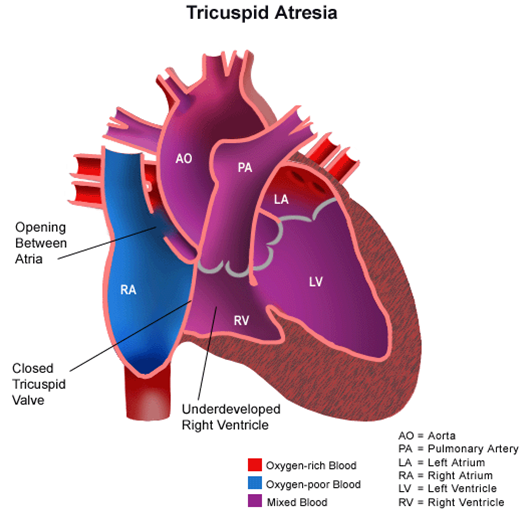
Tricuspid Atresia
{{#ev:youtube|BsvdUEbHyDE}}
In tricuspid atresia, there is no continuity between the right atrium and right ventricle.
Inferior vena cava and superior vena cava collect venous non oxygenated blood into right atrium.
Through ASD blood reaches into left atrium,then left ventricle and aorta. This blood is the mixture of saturated and unsaturated O2.
If there is a VSD, this mixed blood in left ventricle flows into right ventricle , then via pulmonary artery reaches pulmonary bed and becomes oxygenated ,then returns back into left atrium.
In deminished pulmonary blood flow whether the flow is dependent on PDA, the mixed blood in aorta flows from this passage into pulmonary artery and pulmonary bed.
In the presence of normal positioning of great arteries cyanosis is more prominent and is affected by the size of VSD .
Transpositioning great arteries (TGA) and subaortic stenosis are others associated anomalies.
This defect occurs during prenatal development. Because of the lack of an A-V connection, an atrial septal defect (ASD) must be present to maintain blood flow. Also, since there is a lack of a right ventricle there must be a way to pump blood into the pulmonary arteries, and this is accomplished by a ventricular septal defect (VSD). Blood is mixed in the left atrium. Because the only way the pulmonary circulation receives blood is through the VSD, a patent ductus arteriosus is usually also formed to increase pulmonary flow.
Associated Conditions
Classification
Tricuspid atresia is classified according to connection between ventricles with great arteries(aorta, pulmonary) into two subgroups:
- Normal connection between ventricles with aorta and pulmonary artery . this type is much more common and consistence 70%-80% of cases.Most patients are cyanotic.
- Aorta originated from small right ventricle and pulmonary artery comes from left ventricle. Heart failure and pulmonary hypertension are common and patients are not cyanotic. Flow in aorta is dependent on VSD size . Subaortic stenosis and aortic arch anomalies are common.