Cardiac arrest resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Rim Halaby; Vidit Bhargava, M.B.B.S [2]
Synonyms and keywords: cardiorespiratory arrest, cardiopulmonary arrest, circulatory arrest, Advanced life support, ACLS, Basic life support, BLS
Overview
A cardiac arrest is the abrupt cessation of normal blood flow circulation due to the failure of the heart to contract effectively during systole.[1]
Causes
Life Threatening Causes
Cardiac arrest is a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
Reversible Causes
H's
- Hypovolemia
- Hypoxia
- Hydrogen ions (acidosis)
- Hyperkalemia or Hypokalemia
- Hypothermia
- Hypoglycemia or Hyperglycemia
T's
- Tablets or Toxins (tricyclic antidepressants, phenothiazines, beta blockers, calcium channel blockers, cocaine, digoxin, aspirin, acetominophen)
- Cardiac Tamponade
- Tension pneumothorax
- Thrombosis (myocardial infarction)
- Trauma (hypovolemia)
Management
Cardiac Arrest Care: Algorithm 1
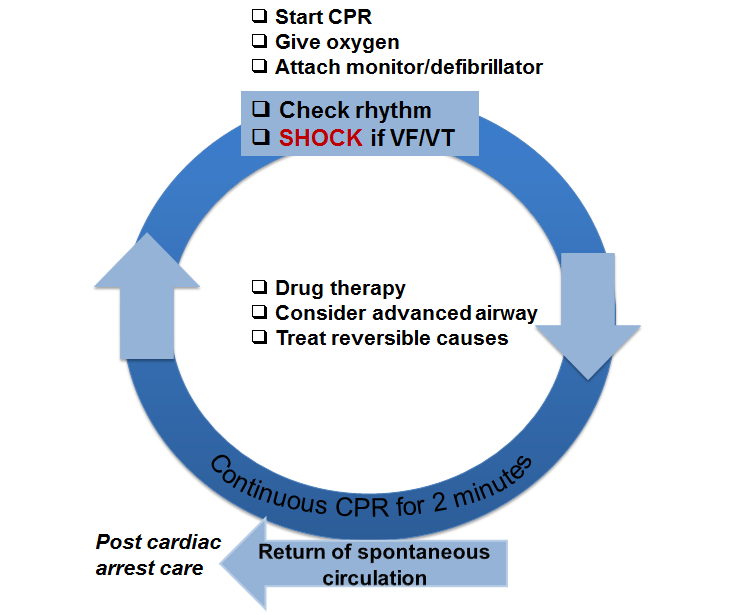 | High Quality CPR: Compressions:
Ventilation:
Drug therapy:
Advanced airway:
Reversible causes:
Shock energy:
Return of Spontaneous Circulation (ROSC):
| ||||||||||||
Adapted from 2010 AHA guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 8.[2]
Cardiac Arrest Care: Algorithm 2
| Adult Cardiac Arrest | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Shout for help ❑ Activate emergency response | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Rhythm shockable? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| VF/VT | Asystole / PEA | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Shock | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Box A: ❑ CPR 2 min ❑ Obtain IV/IO access | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Rhythm shockable? | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Shock | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Box B: | Box C: ❑ CPR 2 min ❑ ObtaimIV/IO access ❑ Administer Epinephrine every 3-5 min ❑ Consider advanced airway and capnography | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Rhythm shockable? | No | Rhythm shockable? | Yes | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Shock | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Box D: ❑ CPR 2 min ❑ Treat reversible causes | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Go back to box A | No | Rhythm shockable? | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Shock Then, go to box A or box B | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If no signs of return of spontaneous circulation: Go to box C or box D If return of spontaneous circulation: Start post cardiac arrest care | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Adapted from 2010 AHA guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 8.[2]
Acute Immediate Post-Cardiac Arrest Care
| Return of spontaneous circulation (ROSC) | |||||||||||||||||||||||||||
Optimize ventilation and oxygenation ❑ Maintain oxygen saturation ≥ 94% ❑ Consider advanced airway and waveform capnography ❑ Do not hyperventilate
| |||||||||||||||||||||||||||
Treat hypotension (SBP<90 mmHg) ❑ IV/IO bolus
❑ Vasopressor infusion
❑ Consider treatable causes ❑ 12-Lead ECG | |||||||||||||||||||||||||||
| Follow commands? | |||||||||||||||||||||||||||
| No | Yes | ||||||||||||||||||||||||||
| ❑ Consider induced hypothermia | |||||||||||||||||||||||||||
| STEMI Or High suspicion of AMI | |||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||
| ❑ Coronary reperfusion | |||||||||||||||||||||||||||
| Advanced critical care | |||||||||||||||||||||||||||
Adapted from 2010 AHA guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 9.[3]
Do's
- Chronotropic drug infusions are recommended as an alternative to pacing in symptomatic and unstable bradycardia.
- Adenosine is recommended as a safe and potentially effective therapy in the initial management of stable undifferentiated regular monomorphic wide-complex tachycardia.
- If using bag and mask ventilation, use adult mask to deliver at least 600 ml of tidal volume, sufficient to produce chest rise, over at least 1 second.
- Perform a head tilt-chin lift maneuver to open the airway, and ensure there is an airtight seal when using bag mask ventilation.
- Oropharyngeal and nasopharyngeal airways may be used to assist in bag and mask ventilation in unconscious patients.
- Continuous waveform capnography is recommended to confirm the placement of endotracehal tube.
- If the cardiac rhythm changes, shift to the appropriate rhythm based strategy.
- If you are not sure of the defibrillator's recommended energy levels, use maximum output level.
Dont's
- Do not use atropine in the management of pulseless electrical activity (PEA)/asystole.
- Do not interrupt the compressions or the use of defibrillator to place an advanced airway, secure IV/IO access or deliver drugs.
- Do not hyperventilate the patient.
- Do not use femoral pulse to assess return of spontaneous circulation (ROSC). The pause in compressions should be used to assess pulse.
References
- ↑ Harrison's Principles of Internal Medicine 16th Edition, The McGraw-Hill Companies, ISBN 0-07-140235-7
- ↑ 2.0 2.1 Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW; et al. (2010). "Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 122 (18 Suppl 3): S729–67. doi:10.1161/CIRCULATIONAHA.110.970988. PMID 20956224.
- ↑ Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M; et al. (2010). "Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 122 (18 Suppl 3): S768–86. doi:10.1161/CIRCULATIONAHA.110.971002. PMID 20956225.