Zollinger-Ellison syndrome pathophysiology
|
Zollinger-Ellison syndrome Microchapters |
|
Differentiating Zollinger-Ellison syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Zollinger-Ellison syndrome pathophysiology On the Web |
|
American Roentgen Ray Society Images of Zollinger-Ellison syndrome pathophysiology |
|
Risk calculators and risk factors for Zollinger-Ellison syndrome pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Aravind Reddy Kothagadi M.B.B.S[2] Mohamad Alkateb, MBBCh [3]
Overview
Zollinger-Ellison syndrome results from increased levels of gastrin due to an existing gastrinoma in the duodenum or pancreas.
Pathogenesis
- Zollinger-Ellison syndrome is a disorder where the production of increased levels of gastrin causes the stomach to release excess amounts of hydrochloric acid. Gastrin then results in an excessive production of acid which often may lead to peptic ulcers (in almost 95% of patients).[1]
- Increased basal gastric acid output and hyyperplasia of the fundic parietal cells occur as a result of excessive amounts of gastrin that secreted by the gastrinoma tumor cells. The excessive gastric acid output overrides the mucosal defense of the gastric and duodenal wall thereby causing ulceration, and inactivation of pancreatic digestive enzymes which therefore results in fat malabsorption and diarrhea. Secretory nature of diarrhea is a result of the inhibition of absorption of sodium and water by the small intestine. [2]
- The pathophysiology of ZES is the stimulatory action of gastrin on the parietal cells of the gastric antrum resulting in hyper-secretory acid milieu. [3]
- Majority of patients with ZES also develop peptic ulcers which are large and multiple in number, usually in the distal duodenum and proximal jejunum (which usually would be an uncommon location for ulcers arising due to Helicobacter pylori or by the use of nonsteroidal anti-inflammatory drugs). [3]
Genetics
- The primary causative lesion is assumed to develop sporadically in approximately 80% of the cases and in the rest of the recorded cases, this entity exists as a part of MEN-1; an autosomal dominant disorder characterized by tumors of the pituitary, the parathyroid, and the pancreas. [4]
- ZES occurs in 20–30% of patients as part of the Multiple Endocrine Neoplasia-type 1 syndrome (MEN1 which is an an autosomal dominant disorder as a result of mutations in an 10-exon gene at 11q13. [5]
Associated Conditions
Gross Pathology
- Gross pathology presents as enlarged fundic mucosal folds with cerebriform pattern.
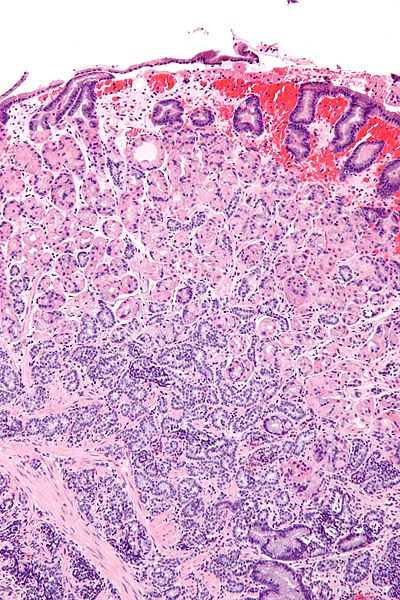
Microscopic Pathology
- A well-differentiated neuroendocrine tumor (NET) histologically typically shows an organ like arrangement of cells with nesting, trabecular, or gyriform patterns. [6]
- The tumor cells are usually round with regular bland nuclei which produce large number of secretory granules with diffuse immunoexpression of neuroendocrine markers.Where as, the poorly differentiated neuroendocrine tumor (NET) shows a atypical, sheet-like, diffuse and irregular nuclei, less cytoplasmic secretory granules, and limited biomarker immunoexpression. [6]
- Immunostaining for chromogranin A and synaptophysin is an important step in the diagnosis of neuroendocrine tumors. In order to differentiate from other neuroendocrine tumors gastrin immunostaining may be used. somatostatin scintigraphy is considered an effective localizing tool as gastrinomas tend to express a high density of somatostatin receptors. [6]
-
Well-differentiated neuroendocrine tumor of the duodenum.
-
Pancreatic neuroendocrine tumour.
-
Gastric neuroendocrine tumour - high magnification
-
Gastric neuroendocrine tumour - intermed_magnification
-
Gastric neuroendocrine tumour - low magnification
-
Gastrinoma
References
- ↑ wikipedia.2015.https://en.wikipedia.org/wiki/Zollinger%E2%80%93Ellison_syndrome
- ↑ "Gastrinoma - StatPearls - NCBI Bookshelf".
- ↑ 3.0 3.1 Epelboym I, Mazeh H (2014). "Zollinger-Ellison syndrome: classical considerations and current controversies". Oncologist. 19 (1): 44–50. doi:10.1634/theoncologist.2013-0369. PMC 3903066. PMID 24319020.
- ↑ Thakker RV, Newey PJ, Walls GV, Bilezikian J, Dralle H, Ebeling PR; et al. (2012). "Clinical practice guidelines for multiple endocrine neoplasia type 1 (MEN1)". J Clin Endocrinol Metab. 97 (9): 2990–3011. doi:10.1210/jc.2012-1230. PMID 22723327.
- ↑ Ito T, Igarashi H, Uehara H, Jensen RT (2013). "Pharmacotherapy of Zollinger-Ellison syndrome". Expert Opin Pharmacother. 14 (3): 307–21. doi:10.1517/14656566.2013.767332. PMC 3580316. PMID 23363383.
- ↑ 6.0 6.1 6.2 Cingam S, Karanchi H. PMID 28722872. Missing or empty
|title=(help)