Wolff-Parkinson-White syndrome medical therapy: Difference between revisions
Rim Halaby (talk | contribs) |
Rim Halaby (talk | contribs) |
||
| Line 29: | Line 29: | ||
===Atrial Fibrillation=== | ===Atrial Fibrillation=== | ||
* | * WPW syndrome with [[atrial fibrillation]] should be suspected whenever the [[ECG]] reveals an irregular rhythm with absent [[P wave]] in the presence of a [[heart rate]] more than 220 beats per minute. In hemodynamically unstable patients, urgent [[direct current cardioversion should be performed. Hemodynamically stable patients should be administered either IV [[procainamide]] ([[ACC AHA guidelines classification scheme|Class I, Level of evidence C]]), [[ibutilide]] ([[ACC AHA guidelines classification scheme|Class I, Level of evidence C]]) or [[flecainide]] ([[ACC AHA guidelines classification scheme|Class IIa, Level of evidence B]]) among [[WPW syndrome]] patients who present with [[atrial fibrillation]] . Intravenous [[quinidine]], [[procainamide]], [[disopyramide]], [[ibutilide]], or [[amiodarone]] can also be considered ([[ACC AHA guidelines classification scheme|Class IIb, Level of evidence B]]).<ref name="pmid23545139">{{cite journal| author=American College of Cardiology Foundation. American Heart Association. European Society of Cardiology. Heart Rhythm Society. Wann LS, Curtis AB et al.| title=Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. | journal=Circulation | year= 2013 | volume= 127 | issue= 18 | pages= 1916-26 | pmid=23545139 | doi=10.1161/CIR.0b013e318290826d | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23545139 }} </ref> | ||
==Long Term Management== | ==Long Term Management== | ||
Revision as of 03:31, 17 April 2014
|
Wolff-Parkinson-White syndrome Microchapters |
|
Differentiating Wolff-Parkinson-White syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Wolff-Parkinson-White syndrome medical therapy On the Web |
|
Risk calculators and risk factors for Wolff-Parkinson-White syndrome medical therapy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Acutely, people with WPW who are experiencing a tachydysrhythmia may require electrical cardioversion if their condition is critical, or, if more stable, medical treatment may be used. Patients with atrial fibrillation and rapid ventricular response are often treated with amiodarone orprocainamide to stabilize their heart rate. Adenosine and other AV node blockers should be avoided in Atrial fibriliiatin with WPW; this inlcudes adenosine, diltiazem, verapamil,other calcium channel blockers and Beta-blockers. Patients with a rapid heart beat with narrow QRS complexes (circus movement tachycardias) may also be cardioverted, alternatively, adenosine may be administered if equipment for cardioversion is immediately available as a backup.
The definitive treatment of WPW syndrome is a destruction of the abnormal electrical pathway by radiofrequency catheter ablation. This procedure is performed almost exclusively by cardiac electrophysiologists. Radiofrequency catheter ablation is not performed in all individuals with WPW syndrome because there are inherent risks involved in the procedure. Adeosine is contraindicated for patients in atrial fibrillation or atrial flutter with a history of WPW
When performed by an experienced electrophysiologist, radiofrequency ablation has a high success rate.[1] If radiofrequency catheter ablation is successfully performed, the patient is generally considered cured. Recurrence rates are typically less than 5% after a successful ablation.[1] The one caveat is that individuals with underlying Ebstein's anomaly may develop additional accessory pathways during progression of their disease.
Acute Treatment
Atrioventricular Reentrant Tachycardia (AVRT)
- AVRT is one of the type of tachycardia that can occur in patients with WPW pattern. AVRT can be either orthodromic or antidromic, and the distinction between the two types is important because it dictates the choice of treatment.
- WPW syndrome patients with AVRT who are hemodynamically unstable, as reflected by hypotension, cold extremities, mottling or peripheral cyanosis, or those who present with ischemic chest pain or decompensated heart failure should urgently undergo direct current cardioversion. The shocks should be delivered as follows:
- Narrow regular rhythm: synchronized electrical cardioversion, 50-100 Joules
- Narrow irregular rhythm: synchronized electrical cardioversion, 120-200 Joules biphasic or 200 Joules monophasic
- Wide regular rhythm: synchronized electrical cardioversion, 100 Joules
- Wide irregular rhythm: unsynchronized electrical cardioversion, 200-360 J monophasic, or 100-200 J biphasic
- The management of WPW syndrome patients who are hemodynamically stable depends on the type of AVRT. When the findings suggest orthodromic AVRT, the patient should be managed similarly to patients with supreventricular tachycardia. The management should begin with vagal maneuvers such as carotid sinus massage and valsalva maneuver. If the patient's tachycardia does not resolve, the patient should be administered IV adenosine. In case of failure to improve, administration of verapamil must be considered followed by procainamide.
- Among patients with antidromic AVRT, AV nodal blocking agents should be avoided because the antegrade impulses are occurring through the accessory pathway and not through the AV node. In this case, the use of digoxin, calcium channel blockers, beta blockers and adenosine should be avoided. Patients should be treated with either procainamide, ibutlide or flecainide.
Atrial Fibrillation
- WPW syndrome with atrial fibrillation should be suspected whenever the ECG reveals an irregular rhythm with absent P wave in the presence of a heart rate more than 220 beats per minute. In hemodynamically unstable patients, urgent [[direct current cardioversion should be performed. Hemodynamically stable patients should be administered either IV procainamide (Class I, Level of evidence C), ibutilide (Class I, Level of evidence C) or flecainide (Class IIa, Level of evidence B) among WPW syndrome patients who present with atrial fibrillation . Intravenous quinidine, procainamide, disopyramide, ibutilide, or amiodarone can also be considered (Class IIb, Level of evidence B).[2]
Long Term Management
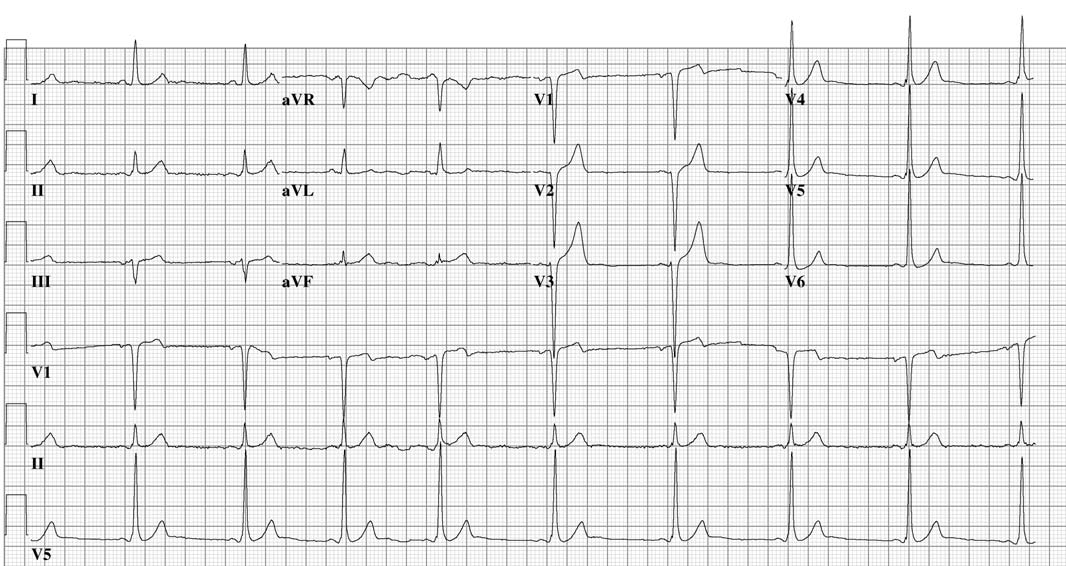
Shown below is an EKG of a 24 years old man with Mahaim type of preexcitation.

Shown below is an EKG of the same patient after Mahaim bundle ablation
References
- ↑ 1.0 1.1 Pappone C, Lamberti F, Santomauro M, Stabile G, De Simone A, Turco P, Pannain S, Loricchio ML, Rotunno R, Chiariello M (1993). "Ablation of paroxysmal tachycardia in Wolff-Parkinson-White syndrome". Cardiologia (in Italian). 38 (12 Suppl 1): 189–97. PMID 8020017.
- ↑ American College of Cardiology Foundation. American Heart Association. European Society of Cardiology. Heart Rhythm Society. Wann LS, Curtis AB; et al. (2013). "Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines". Circulation. 127 (18): 1916–26. doi:10.1161/CIR.0b013e318290826d. PMID 23545139.