Diabetic foot pathophysiology: Difference between revisions
| Line 22: | Line 22: | ||
**[[Alcohol abuse]]. | **[[Alcohol abuse]]. | ||
*Generalized [[Symmetry|symmetric]] distal [[neuropathy|polyneuropathy]] is the most common and widely recognized form of [[diabetic neuropathy]] that leads to [[diabetic foot]]. It may be either [[Sensory system|sensory]] or motor, and can involve small fibers, large fibers or both. | *Generalized [[Symmetry|symmetric]] distal [[neuropathy|polyneuropathy]] is the most common and widely recognized form of [[diabetic neuropathy]] that leads to [[diabetic foot]]. It may be either [[Sensory system|sensory]] or motor, and can involve small fibers, large fibers or both. | ||
**Motor nerve involvement: | |||
===Angiopathy=== | ===Angiopathy=== | ||
Revision as of 20:42, 4 February 2021
|
Diabetic foot Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Diabetic foot pathophysiology On the Web |
|
American Roentgen Ray Society Images of Diabetic foot pathophysiology |
|
Risk calculators and risk factors for Diabetic foot pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Vishnu Vardhan Serla M.B.B.S. [2]
Overview
Pathophysiology
Diabetic foot is an umbrella term for foot problems in patients with diabetes mellitus. There are numerous responsible pathogenesis, such as arterial abnormalities, diabetic neuropathy, delayed wound healing and being more vulnerable to infection or gangrene of the foot. The key components of diabetic foot are neuropathy, angiopathy and trauma. [1]
Neuropathy
- The most important cause of diabetic foot is neuropathy. Based on a study, more than 60% of cases of diabetic foot are due to neuropathy.[2]
- It involves roughly more than half of the patients with diabetes who are older than 60 years old.
- Peripheral neuropathy is usually profound at the point where it leads to formation of a foot ulcer.
- Some metabolic abnormalities due to hyperglycemia leads to ischemia of endoneurial microvessels. In a nutshell, these changes are most likely caused by a combination of factors listed below:
- High blood glucose
- Reactive oxygen species
- Vasculopathy
- Insufficient oxygenation of the nerves
- Presence of inflammation and autoimmunity due to diabetes
- Genetic factors
- Mechanical injury
- Smoking
- Alcohol abuse.
- Generalized symmetric distal polyneuropathy is the most common and widely recognized form of diabetic neuropathy that leads to diabetic foot. It may be either sensory or motor, and can involve small fibers, large fibers or both.
- Motor nerve involvement:
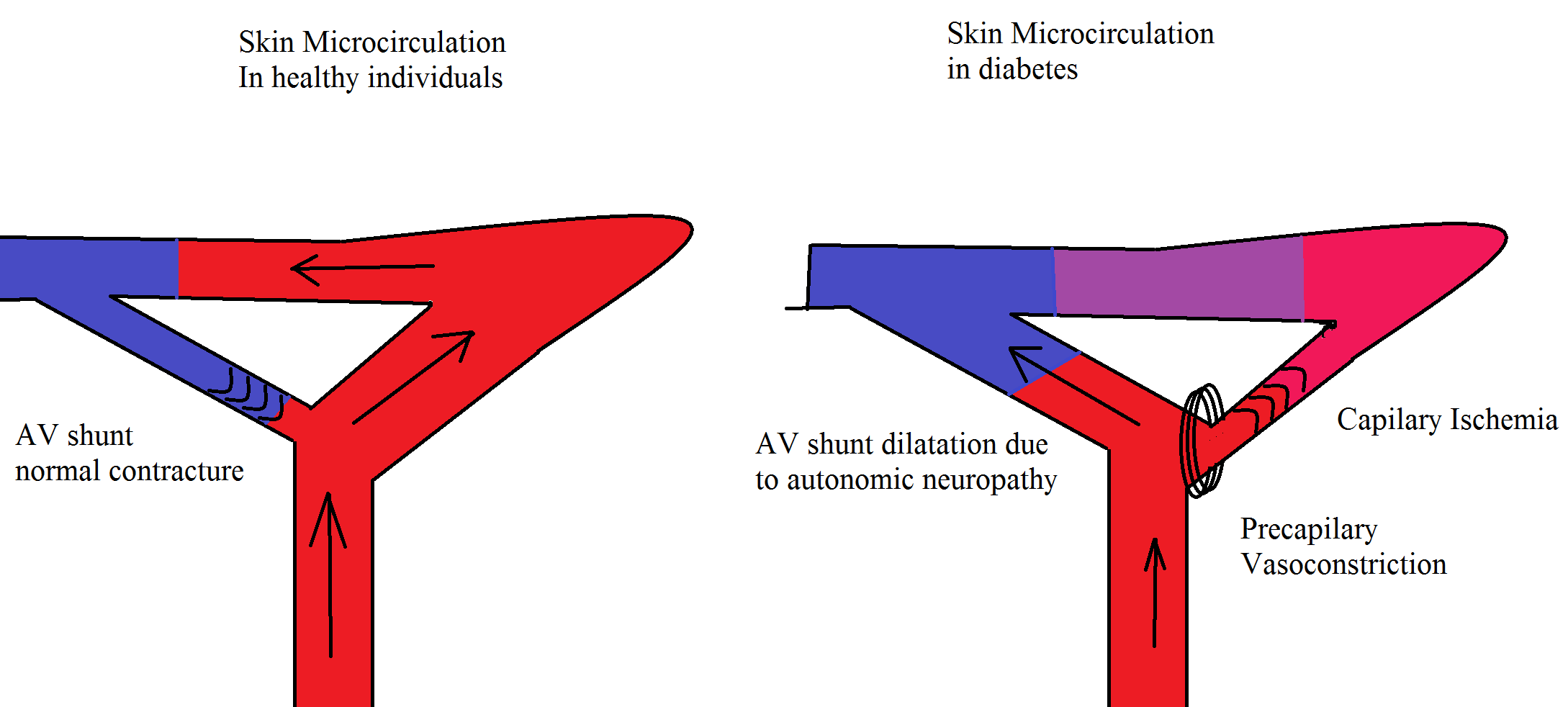
Angiopathy
Micro and macrovascular complications are the leading cause of diabetic complications. Atherosclerosis occurs due to inflammation and leads to the accumulation of foam cells. The vascular changes which are responsible for foot problems include stiff arteries due to calcification of the smooth muscle cells in the arterial wall (mediasclerosis). It is usually discovered by an impaired ankle brachial index (ABI). The resting ABI is the ratio of the blood pressure in the lower legs to the blood pressure in the arms. The ABI is calculated by dividing the systolic blood pressure at the ankle by the systolic blood pressures in the arm. It is a non-invasive method to assess the lower extremity arterial system and to detect the presence of arterial occlusion disease. In severe cases, it leads to ischemic foot problems, which the only treatment is vascular surgery. Even in neuropathic foot ulcers, the non healing wounds are the result of impaired blood supply to the tissue. Decreasing the central blood pressure by antihypertensive drugs may be deleterious for these patients[3]. Microvascular complications cause skin damage, infection and impaired wound healing. Once a foot ulcer develops, peripheral vascular disease is the most important factor which may contribute to adverse outcomes. Vascular complications are like a positive feedback which worsen the skin and nerve damage in diabetes [4]
Trauma
- Trauma to the foot is frequently the trigger of diabetic foot ulcer development and repetitive trauma and pressure to the area prevent [Wound healing|healing]].[5]
- Excessive plantar pressure is related to limited joint mobility and foot deformities (such as charcot foot and hammer toe). Limited joint mobility and abnormal foot biomechanisms have been associated to an increased risk of ulceration.[3]
- Poor vision and sensory neuropathy further put diabetic patients at risk of foot ulceration, as they not feel the pain, nor do they see the ulcer. Loss of balance can also make patients more susceptible to falls.[3]
Genetics
Associated Conditions
Conditions associated with [disease name] include:
- [Condition 1]
- [Condition 2]
- [Condition 3]
Gross Pathology
On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Microscopic Pathology
On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
References
- ↑ Assal JP, Mehnert H, Tritschler HJ, Sidorenko A, Keen H, Hellmut Mehnert Award Workshop Participants (2002). "On your feet! Workshop on the diabetic foot". J Diabetes Complications. 16 (2): 183–94. PMID 12039404.
- ↑ Grunfeld C (1992). "Diabetic foot ulcers: etiology, treatment, and prevention". Adv Intern Med. 37: 103–32. PMID 1557993.
- ↑ 3.0 3.1 3.2 Alexiadou K, Doupis J (2012). "Management of diabetic foot ulcers". Diabetes Ther. 3 (1): 4. doi:10.1007/s13300-012-0004-9. PMID 22529027.
- ↑ Venermo M, Vikatmaa P, Terasaki H, Sugano N (2012). "Vascular laboratory for critical limb ischaemia". Scand J Surg. 101 (2): 86–93. PMID 22623440.
- ↑ Noor S, Zubair M, Ahmad J (2015). "Diabetic foot ulcer--A review on pathophysiology, classification and microbial etiology". Diabetes Metab Syndr. 9 (3): 192–9. doi:10.1016/j.dsx.2015.04.007. PMID 25982677.