Restrictive cardiomyopathy: Difference between revisions
| Line 234: | Line 234: | ||
===Neuromuscular=== | ===Neuromuscular=== | ||
* Neuromuscular examination of patients with | * Neuromuscular examination of patients with restrictive cardiomyopathy is usually normal. | ||
===Extremities=== | ===Extremities=== | ||
Revision as of 18:38, 10 December 2019
| https://https://www.youtube.com/watch?v=JONXrVH4jQU%7C350}} |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Infiltrative cardiomyopathy; RCM; stiff heart; stiffening of the heart; heart stiffening; stiffened heart
Overview
Historical Perspective
Classification
Pathophysiology
Causes
The main Causes of restrictive cardiomyopathy are enlisted below:[1][2]
- Amyloidosis (AL, ATTR, SSA)
- Sarcoidosis
- Hemochromatosis
- Eosinophilic myocardial disease
- Idiopathic RCM
- Progressive systemic sclerosis (scleroderma)
- Postradiation therapy (Hodgkin's lymphoma, breast cancer etc)
- Anderson Fabry disease
- Danon's disease
- Friedreich's ataxia
- Diabetic cardiomyopathy (restrictive phenotype)
- Drug induced (anthracycline toxicity, methysergide, ergotamine, mercurial agents, etc.)
- Mucopolysaccharidoses (Hurler's cardiomyopathy)
- Myocardial oxalosis
- Wegener's granulomatosis
- Metastatic malignancies
Differentiating restrictive cardiomyopathy from Other Diseases
Restrictive cardiomyopathy should be differentiated from dilated cardiomyopathy, hypertrophic cardiomyopathy, congestive heart failure ect [2],[1]
| Type of disease | History | Physical examination | Chest X-ray | ECG | 2D echo | Doppler echo | CT | MRI | Catheterization hemodynamics | Biopsy |
| Restrictive cardiomyopathy[2][3] | Systemic disease (e.g., sarcoidosis, hemochromatosis). | ± Kussmaul sign, S3 and S4 gallop, murmurs of mitral and tricuspid regurgitation | Atrial dilatation | Low QRS voltages (mainly amyloidosis), conduction disturbances, nonspecific ST abnormalities | ± Wall and valvular thickening, sparkling myocardium | Decreased variation in mitral and/or tricuspid inflow E velocity, increased hepatic vein inspiratory diastolic flow reversal, presence of mitral and tricuspid regurgitation | Normal pericardium | Measurement of iron overload, various types of LGE (late gadolinium enhancement) | LVEDP – RVEDP ≥ 5 mmHg
RVSP ≥ 55 mmHg RVEDP/RVSP ≤ 0.33 |
May reveal underlying cause. |
| Constrictive pericarditis | Prior history of pericarditis or conditions affecting the pericardium. | Pericardial knock | Pericardial calcification | Nonspecific ST and T abnormalities, low QRS voltage (<50%) | ± Pericardial thickening, respiratory ventricular septal shift. | Increased variation in mitral and/or tricuspid inflow E velocity, hepatic vein expiratory diastolic reversal ratio ≥ 0.79 medial e′/lateral e′ ≥ 0.91 (Annulus Reversus) | Thickened/calcified pericardium | Thickened pericardium | LVEDP – RVEDP < 5 mmHg
RVSP < 55 mmHg RVEDP/RVSP > 0.33 Inspiratory decrease in RAP < 5 mmHg Systolic area index > 1.1 (Ref CP in the modern era) Left ventricular height of rapid filling wave > 7 mmHg |
Normal myocardium |
| Hypertrophic cardiomyopathy(HCM)[4][5] | Commonly asymptomatic/minimally symptomatic. Exertional dyspnea or syncope. | In LVOT obstruction, a harsh, mid-systolic, Grade 3–4/6 murmur loudest between the apex and the left sternal border is usually audible. Precordial impulse is forceful and displaced leftward and the peripheral arterial pulses are brisk. | ||||||||
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications, and Prognosis
Diagnosis
Diagnostic Study of Choice
History and Symptoms
- The majority of patients with [disease name] are asymptomatic.
OR
- The hallmark of [disease name] is [finding]. A positive history of [finding 1] and [finding 2] is suggestive of [disease name]. The most common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3].
- Symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3].
History
Patients with [disease name]] may have a positive history of:
- [History finding 1]
- [History finding 2]
- [History finding 3]
Common Symptoms
Common symptoms of [disease] include:
- Dyspnea
- Fatigue
- Limited exercise capacity
- Palpitations
- Syncope
Less Common Symptoms
Less common symptoms of restrictive cardiomyopathy include
- Angina
Physical Examination
Physical examination of patients with [disease name] is usually normal.
OR
Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Appearance of the Patient
- Patients with [disease name] usually appear [general appearance].
Vital Signs
- High-grade / low-grade fever
- Hypothermia / hyperthermia may be present
- Tachycardia with regular pulse or (ir)regularly irregular pulse
- Bradycardia with regular pulse or (ir)regularly irregular pulse
- Tachypnea / bradypnea
- Kussmal respirations may be present in _____ (advanced disease state)
- Weak/bounding pulse / pulsus alternans / paradoxical pulse / asymmetric pulse
- High/low blood pressure with normal pulse pressure / wide pulse pressure / narrow pulse pressure
Skin
- Skin examination of patients with restrictive cardiomyopathy is usually normal.
HEENT
- HEENT examination of patients with restrictive cardiomyopathy is usually normal.
Neck
- Jugular venous distension is noted sometimes with kussmaul sign
- Hepatojugular reflux
Lungs
- Fine/coarse crackles upon auscultation of the lung bases/apices unilaterally/bilaterally
- Rhonchi
Heart
Abdomen
Back
- Back examination of patients with restrictive cardiomyopathy is usually normal.
Genitourinary
- Genitourinary examination of patients with restrictive cardiomyopathy is usually normal.
Neuromuscular
- Neuromuscular examination of patients with restrictive cardiomyopathy is usually normal.
Extremities
- Extremities examination of patients with [disease name] is usually normal.
OR
- Clubbing
- Cyanosis
- Pitting/non-pitting edema of the upper/lower extremities
- Muscle atrophy
- Fasciculations in the upper/lower extremity
Laboratory Findings
Electrocardiogram
X-ray
Echocardiography and Ultrasound
CT scan
MRI
Other Imaging Findings
Other Diagnostic Studies
Treatment
Medical Therapy
Interventions
Surgery
Primary Prevention
Secondary Prevention
References
- ↑ 1.0 1.1 Hong JA, Kim MS, Cho MS, Choi HI, Kang DH, Lee SE, Lee GY, Jeon ES, Cho JY, Kim KH, Yoo BS, Lee JY, Kim WJ, Kim KH, Chung WJ, Lee JH, Cho MC, Kim JJ (September 2017). "Clinical features of idiopathic restrictive cardiomyopathy: A retrospective multicenter cohort study over 2 decades". Medicine (Baltimore). 96 (36): e7886. doi:10.1097/MD.0000000000007886. PMC 6393124. PMID 28885342.
- ↑ 2.0 2.1 2.2 Rammos A, Meladinis V, Vovas G, Patsouras D (2017). "Restrictive Cardiomyopathies: The Importance of Noninvasive Cardiac Imaging Modalities in Diagnosis and Treatment-A Systematic Review". Radiol Res Pract. 2017: 2874902. doi:10.1155/2017/2874902. PMC 5705874. PMID 29270320.
- ↑ Mogensen J, Kubo T, Duque M, Uribe W, Shaw A, Murphy R, Gimeno JR, Elliott P, McKenna WJ (January 2003). "Idiopathic restrictive cardiomyopathy is part of the clinical expression of cardiac troponin I mutations". J. Clin. Invest. 111 (2): 209–16. doi:10.1172/JCI16336. PMC 151864. PMID 12531876.
- ↑ Kubo T, Gimeno JR, Bahl A, Steffensen U, Steffensen M, Osman E, Thaman R, Mogensen J, Elliott PM, Doi Y, McKenna WJ (June 2007). "Prevalence, clinical significance, and genetic basis of hypertrophic cardiomyopathy with restrictive phenotype". J. Am. Coll. Cardiol. 49 (25): 2419–26. doi:10.1016/j.jacc.2007.02.061. PMID 17599605.
- ↑ Marian AJ, Braunwald E (September 2017). "Hypertrophic Cardiomyopathy: Genetics, Pathogenesis, Clinical Manifestations, Diagnosis, and Therapy". Circ. Res. 121 (7): 749–770. doi:10.1161/CIRCRESAHA.117.311059. PMC 5654557. PMID 28912181.
Overview
Restrictive cardiomyopathy is the least common cardiomyopathy. It is called this because it restricts the heart from stretching and filling with blood properly. Rhythmicity and contractility of the heart may be normal, but the stiff walls of the heart chambers (atria and ventricles) keep them from adequately filling. So blood flow is reduced, and blood that would normally enter the heart is backed up in the circulatory system. In time, restrictive cardiomyopathy patients develop heart failure.
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated. There are no known life threatening causes of restrictive cardiomyopathy that may result in death within 24 hours if not treated.
Common Causes
Causes by Organ System
Causes in Alphabetical Order
Diagnosis
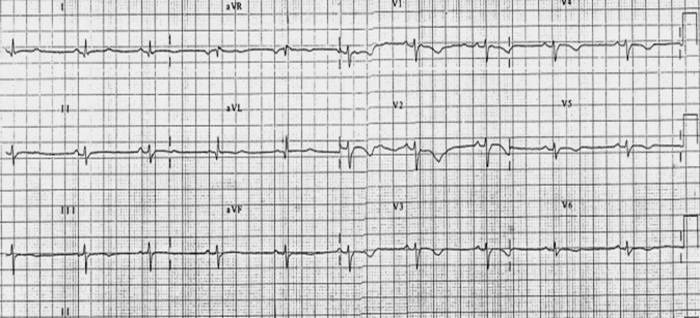
Electrocardiogram
Shown below is an example of restrictive cardiomyopathy with low voltage and flipped anterior T waves.