Lower gastrointestinal bleeding pathophysiology: Difference between revisions
Iqra Qamar (talk | contribs) |
Iqra Qamar (talk | contribs) |
||
| Line 67: | Line 67: | ||
:*[[Mesenteric ischemia]] results when there is inadequate blood supply at the level of the [[small intestine]].<ref name="pmid9146726">{{cite journal |vauthors=Krupski WC, Selzman CH, Whitehill TA |title=Unusual causes of mesenteric ischemia |journal=Surg. Clin. North Am. |volume=77 |issue=2 |pages=471–502 |year=1997 |pmid=9146726 |doi= |url=}}</ref><ref name="pmid21326562">{{cite journal |vauthors=Walker TG |title=Mesenteric ischemia |journal=Semin Intervent Radiol |volume=26 |issue=3 |pages=175–83 |year=2009 |pmid=21326562 |pmc=3036494 |doi=10.1055/s-0029-1225662 |url=}}</ref><ref name="pmid18625147">{{cite journal |vauthors=Berland T, Oldenburg WA |title=Acute mesenteric ischemia |journal=Curr Gastroenterol Rep |volume=10 |issue=3 |pages=341–6 |year=2008 |pmid=18625147 |doi= |url=}}</ref><ref name="pmid26909235">{{cite journal |vauthors=Mastoraki A, Mastoraki S, Tziava E, Touloumi S, Krinos N, Danias N, Lazaris A, Arkadopoulos N |title=Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities |journal=World J Gastrointest Pathophysiol |volume=7 |issue=1 |pages=125–30 |year=2016 |pmid=26909235 |pmc=4753178 |doi=10.4291/wjgp.v7.i1.125 |url=}}</ref> | :*[[Mesenteric ischemia]] results when there is inadequate blood supply at the level of the [[small intestine]].<ref name="pmid9146726">{{cite journal |vauthors=Krupski WC, Selzman CH, Whitehill TA |title=Unusual causes of mesenteric ischemia |journal=Surg. Clin. North Am. |volume=77 |issue=2 |pages=471–502 |year=1997 |pmid=9146726 |doi= |url=}}</ref><ref name="pmid21326562">{{cite journal |vauthors=Walker TG |title=Mesenteric ischemia |journal=Semin Intervent Radiol |volume=26 |issue=3 |pages=175–83 |year=2009 |pmid=21326562 |pmc=3036494 |doi=10.1055/s-0029-1225662 |url=}}</ref><ref name="pmid18625147">{{cite journal |vauthors=Berland T, Oldenburg WA |title=Acute mesenteric ischemia |journal=Curr Gastroenterol Rep |volume=10 |issue=3 |pages=341–6 |year=2008 |pmid=18625147 |doi= |url=}}</ref><ref name="pmid26909235">{{cite journal |vauthors=Mastoraki A, Mastoraki S, Tziava E, Touloumi S, Krinos N, Danias N, Lazaris A, Arkadopoulos N |title=Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities |journal=World J Gastrointest Pathophysiol |volume=7 |issue=1 |pages=125–30 |year=2016 |pmid=26909235 |pmc=4753178 |doi=10.4291/wjgp.v7.i1.125 |url=}}</ref> | ||
:*2 or more vessels ([[Celiac artery|celiac]], [[Superior mesenteric artery|SMA]], or [[Inferior mesenteric artery|IMA]]) must be involved for bleeding to occur. | :*2 or more vessels ([[Celiac artery|celiac]], [[Superior mesenteric artery|SMA]], or [[Inferior mesenteric artery|IMA]]) must be involved for bleeding to occur. | ||
:*Non occlusive | :*Non occlusive [[mesenteric ischemia]] affects critically ill patients who are [[vasopressor]]-dependent. | ||
:*[[Venous thrombosis]] of the visceral vessels can also precipitate an acute ischemic event. | :*[[Venous thrombosis]] of the [[visceral]] [[vessels]] can also precipitate an [[acute]] [[ischemic]] event. | ||
:*Decreased blood flow leads to transmural infarction with [[necrosis]] and [[perforation]]. | :*Decreased blood flow leads to transmural [[infarction]] with [[necrosis]] and [[perforation]]. | ||
:*Associated mucosal sloughing results in bleeding. | :*Associated [[mucosal]] sloughing results in bleeding. | ||
*'''<u>[[Ischemic colitis|Ischemic Colitis]]</u>''' | *'''<u>[[Ischemic colitis|Ischemic Colitis]]</u>''' | ||
:*[[Ischemic colitis]] is caused by poor [[perfusion]] of the [[colon]], which results in the inability of that area of the colon to meet its metabolic demands.<ref name="pmid26034405">{{cite journal |vauthors=FitzGerald JF, Hernandez Iii LO |title=Ischemic colitis |journal=Clin Colon Rectal Surg |volume=28 |issue=2 |pages=93–8 |year=2015 |pmid=26034405 |pmc=4442720 |doi=10.1055/s-0035-1549099 |url=}}</ref><ref name="pmid19109863">{{cite journal |vauthors=Theodoropoulou A, Koutroubakis IE |title=Ischemic colitis: clinical practice in diagnosis and treatment |journal=World J. Gastroenterol. |volume=14 |issue=48 |pages=7302–8 |year=2008 |pmid=19109863 |pmc=2778113 |doi= |url=}}</ref><ref name="pmid25504381">{{cite journal |vauthors=Rania H, Mériam S, Rym E, Hyafa R, Amine A, Najet BH, Lassad G, Mohamed TK |title=Ischemic colitis in five points: an update 2013 |journal=Tunis Med |volume=92 |issue=5 |pages=299–303 |year=2014 |pmid=25504381 |doi= |url=}}</ref> | :*[[Ischemic colitis]] is caused by poor [[perfusion]] of the [[colon]], which results in the inability of that area of the [[colon]] to meet its [[metabolic]] demands.<ref name="pmid26034405">{{cite journal |vauthors=FitzGerald JF, Hernandez Iii LO |title=Ischemic colitis |journal=Clin Colon Rectal Surg |volume=28 |issue=2 |pages=93–8 |year=2015 |pmid=26034405 |pmc=4442720 |doi=10.1055/s-0035-1549099 |url=}}</ref><ref name="pmid19109863">{{cite journal |vauthors=Theodoropoulou A, Koutroubakis IE |title=Ischemic colitis: clinical practice in diagnosis and treatment |journal=World J. Gastroenterol. |volume=14 |issue=48 |pages=7302–8 |year=2008 |pmid=19109863 |pmc=2778113 |doi= |url=}}</ref><ref name="pmid25504381">{{cite journal |vauthors=Rania H, Mériam S, Rym E, Hyafa R, Amine A, Najet BH, Lassad G, Mohamed TK |title=Ischemic colitis in five points: an update 2013 |journal=Tunis Med |volume=92 |issue=5 |pages=299–303 |year=2014 |pmid=25504381 |doi= |url=}}</ref> | ||
:*It can be [[gangrenous]] or nongangrenous, acute, transient | :*It can be [[gangrenous]] or nongangrenous, acute or chronic, transient or permanent. | ||
:*The [[Colon (anatomy)|left colon]] is predominantly affected, with the [[splenic flexure]] having increased susceptibility. | :*The [[Colon (anatomy)|left colon]] is predominantly affected, with the [[splenic flexure]] having increased susceptibility. | ||
:*Intraluminal [[hemorrhage]] occurs as the [[mucosa]] becomes [[necrotic]], sloughs, and bleeds. | :*Intraluminal [[hemorrhage]] occurs as the [[mucosa]] becomes [[necrotic]], sloughs, and bleeds. | ||
:*Damage to the tissue is caused both with the ischemic insult as well as [[reperfusion injury]]. | :*Damage to the tissue is caused both with the [[ischemic]] insult as well as [[reperfusion injury]]. | ||
*'''<u>Inflammatory Bowel Disease</u>'''<ref name="pmid28261018">{{cite journal |vauthors=Kim DH, Cheon JH |title=Pathogenesis of Inflammatory Bowel Disease and Recent Advances in Biologic Therapies |journal=Immune Netw |volume=17 |issue=1 |pages=25–40 |year=2017 |pmid=28261018 |pmc=5334120 |doi=10.4110/in.2017.17.1.25 |url=}}</ref><ref name="pmid11781268">{{cite journal |vauthors=Hendrickson BA, Gokhale R, Cho JH |title=Clinical aspects and pathophysiology of inflammatory bowel disease |journal=Clin. Microbiol. Rev. |volume=15 |issue=1 |pages=79–94 |year=2002 |pmid=11781268 |pmc=118061 |doi= |url=}}</ref> | *'''<u>Inflammatory Bowel Disease</u>'''<ref name="pmid28261018">{{cite journal |vauthors=Kim DH, Cheon JH |title=Pathogenesis of Inflammatory Bowel Disease and Recent Advances in Biologic Therapies |journal=Immune Netw |volume=17 |issue=1 |pages=25–40 |year=2017 |pmid=28261018 |pmc=5334120 |doi=10.4110/in.2017.17.1.25 |url=}}</ref><ref name="pmid11781268">{{cite journal |vauthors=Hendrickson BA, Gokhale R, Cho JH |title=Clinical aspects and pathophysiology of inflammatory bowel disease |journal=Clin. Microbiol. Rev. |volume=15 |issue=1 |pages=79–94 |year=2002 |pmid=11781268 |pmc=118061 |doi= |url=}}</ref> | ||
**'''[[Crohn's disease]]''' | **'''[[Crohn's disease]]''' | ||
***In [[Crohn's disease]] [[T cell]] activation stimulates [[Interleukin 12|interleukin (IL)-12]] and [[Tumor necrosis factor alpha|tumor necrosis factor (TNF)-α]], | ***In [[Crohn's disease]], [[T cell]] activation stimulates [[Interleukin 12|interleukin (IL)-12]] and [[Tumor necrosis factor alpha|tumor necrosis factor (TNF)-α]], resulting in [[chronic]] [[inflammation]] and tissue injury.<ref name="pmid4447044">{{cite journal |vauthors=Woźniak-Parnowska W, Werakso B |title=[Comparative studies of microbiological purity of ointments by the direct culture method and use of membrane filters] |language=Polish |journal=Acta Pol Pharm |volume=31 |issue=6 |pages=819–23 |year=1974 |pmid=4447044 |doi= |url=}}</ref><ref name="pmid24395894">{{cite journal |vauthors=Mazal J |title=Crohn disease: pathophysiology, diagnosis, and treatment |journal=Radiol Technol |volume=85 |issue=3 |pages=297–316; quiz 317–20 |year=2014 |pmid=24395894 |doi= |url=}}</ref><ref name="pmid2694136">{{cite journal |vauthors=Jewell DP |title=Aetiology and pathogenesis of ulcerative colitis and Crohn's disease |journal=Postgrad Med J |volume=65 |issue=768 |pages=718–9 |year=1989 |pmid=2694136 |pmc=2429831 |doi= |url=}}</ref><ref name="pmid16819502">{{cite journal |vauthors=Sartor RB |title=Mechanisms of disease: pathogenesis of Crohn's disease and ulcerative colitis |journal=Nat Clin Pract Gastroenterol Hepatol |volume=3 |issue=7 |pages=390–407 |year=2006 |pmid=16819502 |doi=10.1038/ncpgasthep0528 |url=}}</ref><ref name="pmid15656711">{{cite journal |vauthors=Head K, Jurenka JS |title=Inflammatory bowel disease. Part II: Crohn's disease--pathophysiology and conventional and alternative treatment options |journal=Altern Med Rev |volume=9 |issue=4 |pages=360–401 |year=2004 |pmid=15656711 |doi= |url=}}</ref><ref name="pmid24415861">{{cite journal |vauthors=Zhang YZ, Li YY |title=Inflammatory bowel disease: pathogenesis |journal=World J. Gastroenterol. |volume=20 |issue=1 |pages=91–9 |year=2014 |pmid=24415861 |pmc=3886036 |doi=10.3748/wjg.v20.i1.91 |url=}}</ref> | ||
***Initially, [[inflammation]] starts focally around the [[Crypts of Lieberkühn|crypts]], followed by superficial [[ulceration]] of the [[mucosa]]. | ***Initially, [[inflammation]] starts focally around the [[Crypts of Lieberkühn|crypts]], followed by superficial [[ulceration]] of the [[mucosa]]. | ||
***The deep mucosal layers are then invaded in a noncontinuous fashion, and noncaseating granulomas form, which can invade through the entire thickness of the bowel and into the mesentery and surrounding structures resulting in bleeding | ***The deep [[mucosal]] layers are then invaded in a noncontinuous fashion, and noncaseating [[granulomas]] form, which can invade through the entire thickness of the bowel wall and into the [[mesentery]] and surrounding structures resulting in bleeding. | ||
:* '''<u>Ulcerative colitis</u>''' | :* '''<u>Ulcerative colitis</u>''' | ||
:** In [[ulcerative colitis]] [[T cells]] [[cytotoxic]] to the colonic epithelium accumulate in the [[lamina propria]], accompanied by [[B cells]] that secrete [[immunoglobulin G]] ([[Immunoglobulin G|IgG]]) and [[Immunoglobulin E|IgE]].<ref name="pmid16819502">{{cite journal |vauthors=Sartor RB |title=Mechanisms of disease: pathogenesis of Crohn's disease and ulcerative colitis |journal=Nat Clin Pract Gastroenterol Hepatol |volume=3 |issue=7 |pages=390–407 |year=2006 |pmid=16819502 |doi=10.1038/ncpgasthep0528 |url=}}</ref><ref name="pmid27914657">{{cite journal |vauthors=Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF |title=Ulcerative colitis |journal=Lancet |volume=389 |issue=10080 |pages=1756–1770 |year=2017 |pmid=27914657 |doi=10.1016/S0140-6736(16)32126-2 |url=}}</ref><ref name="pmid11830216">{{cite journal |vauthors=Farrell RJ, Peppercorn MA |title=Ulcerative colitis |journal=Lancet |volume=359 |issue=9303 |pages=331–40 |year=2002 |pmid=11830216 |doi=10.1016/S0140-6736(02)07499-8 |url=}}</ref><ref name="pmid1516252">{{cite journal |vauthors=Rönnblom LE, Janson ET, Perers A, Oberg KE, Alm GV |title=Characterization of anti-interferon-alpha antibodies appearing during recombinant interferon-alpha 2a treatment |journal=Clin. Exp. Immunol. |volume=89 |issue=3 |pages=330–5 |year=1992 |pmid=1516252 |pmc=1554468 |doi= |url=}}</ref> | :** In [[ulcerative colitis]], [[T cells]], [[cytotoxic]] to the colonic epithelium, accumulate in the [[lamina propria]], accompanied by [[B cells]] that secrete [[immunoglobulin G]] ([[Immunoglobulin G|IgG]]) and [[Immunoglobulin E|IgE]].<ref name="pmid16819502">{{cite journal |vauthors=Sartor RB |title=Mechanisms of disease: pathogenesis of Crohn's disease and ulcerative colitis |journal=Nat Clin Pract Gastroenterol Hepatol |volume=3 |issue=7 |pages=390–407 |year=2006 |pmid=16819502 |doi=10.1038/ncpgasthep0528 |url=}}</ref><ref name="pmid27914657">{{cite journal |vauthors=Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF |title=Ulcerative colitis |journal=Lancet |volume=389 |issue=10080 |pages=1756–1770 |year=2017 |pmid=27914657 |doi=10.1016/S0140-6736(16)32126-2 |url=}}</ref><ref name="pmid11830216">{{cite journal |vauthors=Farrell RJ, Peppercorn MA |title=Ulcerative colitis |journal=Lancet |volume=359 |issue=9303 |pages=331–40 |year=2002 |pmid=11830216 |doi=10.1016/S0140-6736(02)07499-8 |url=}}</ref><ref name="pmid1516252">{{cite journal |vauthors=Rönnblom LE, Janson ET, Perers A, Oberg KE, Alm GV |title=Characterization of anti-interferon-alpha antibodies appearing during recombinant interferon-alpha 2a treatment |journal=Clin. Exp. Immunol. |volume=89 |issue=3 |pages=330–5 |year=1992 |pmid=1516252 |pmc=1554468 |doi= |url=}}</ref> | ||
:** This results in [[inflammation]] of the [[crypts of Lieberkuhn]], with [[abscesses]] and [[pseudopolyps]] along with rupturing of minute blood vessels in mucosa resulting in bleeding. | :** This results in [[inflammation]] of the [[crypts of Lieberkuhn]], with [[abscesses]] and [[pseudopolyps]] along with rupturing of minute [[blood vessels]] in [[mucosa]] resulting in bleeding. | ||
*'''<u>Neoplasia</u>''' | *'''<u>Neoplasia</u>''' | ||
:*Mutations of multiple genes are required for the formation of [[Colon cancer|adenocarcinoma]], including the [[APC (gene)|APC gene]], Kras, DCC, and [[P53 (protein)|p53]].<ref name="pmid12702969">{{cite journal |vauthors=Itzkowitz S |title=Colon carcinogenesis in inflammatory bowel disease: applying molecular genetics to clinical practice |journal=J. Clin. Gastroenterol. |volume=36 |issue=5 Suppl |pages=S70–4; discussion S94–6 |year=2003 |pmid=12702969 |doi= |url=}}</ref><ref name="pmid21530747">{{cite journal |vauthors=Ullman TA, Itzkowitz SH |title=Intestinal inflammation and cancer |journal=Gastroenterology |volume=140 |issue=6 |pages=1807–16 |year=2011 |pmid=21530747 |doi=10.1053/j.gastro.2011.01.057 |url=}}</ref><ref name="pmid19589728">{{cite journal |vauthors=Kraus S, Arber N |title=Inflammation and colorectal cancer |journal=Curr Opin Pharmacol |volume=9 |issue=4 |pages=405–10 |year=2009 |pmid=19589728 |doi=10.1016/j.coph.2009.06.006 |url=}}</ref> | :*Mutations of multiple genes are required for the formation of [[Colon cancer|adenocarcinoma]], including the [[APC (gene)|APC gene]], Kras, DCC, and [[P53 (protein)|p53]].<ref name="pmid12702969">{{cite journal |vauthors=Itzkowitz S |title=Colon carcinogenesis in inflammatory bowel disease: applying molecular genetics to clinical practice |journal=J. Clin. Gastroenterol. |volume=36 |issue=5 Suppl |pages=S70–4; discussion S94–6 |year=2003 |pmid=12702969 |doi= |url=}}</ref><ref name="pmid21530747">{{cite journal |vauthors=Ullman TA, Itzkowitz SH |title=Intestinal inflammation and cancer |journal=Gastroenterology |volume=140 |issue=6 |pages=1807–16 |year=2011 |pmid=21530747 |doi=10.1053/j.gastro.2011.01.057 |url=}}</ref><ref name="pmid19589728">{{cite journal |vauthors=Kraus S, Arber N |title=Inflammation and colorectal cancer |journal=Curr Opin Pharmacol |volume=9 |issue=4 |pages=405–10 |year=2009 |pmid=19589728 |doi=10.1016/j.coph.2009.06.006 |url=}}</ref> | ||
Revision as of 17:08, 21 December 2017
|
Lower gastrointestinal bleeding Microchapters |
|
Differentiating Lower gastrointestinal bleeding from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Management |
|
Surgery |
|
Case Studies |
|
Lower gastrointestinal bleeding pathophysiology On the Web |
|
American Roentgen Ray Society Images of Lower gastrointestinal bleeding pathophysiology |
|
Risk calculators and risk factors for Lower gastrointestinal bleeding pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aditya Ganti M.B.B.S. [2]
Overview
Superior mesenteric artery and inferior mesenteric artery are the two major blood vessels that supply lower gastrointestinal tract. Disruption of blood vessel junction, formed by these two vessels, by any of the disease process results in bleeding. Diverticulosis is the most common etiology of lower GI bleeding accounting for 30% of all cases, followed by ano-rectal disease, ischemia of bowel, inflammatory bowel disease (IBD), neoplasia, and arteriovenous (AV) malformations. The characteristic gross and microscopic findings of lower gastrointestinal tracts depends upon the underlying pathology.
Pathophysiology
Blood supply
- Superior mesenteric artery and inferior mesenteric artery are the two major blood vessels that supply lower gastrointestinal tract.[1][2][3]
- The superior mesenteric artery and inferior mesenteric artery are interconnected through a branch of anastomosis between various branches which are collectively called as marginal artery of Drummond.
- This vascular arcade runs in the mesentery close to the bowel.
| Lower GI Tract | Arterial Supply | Venous Drainage | |
|---|---|---|---|
| Midgut | |||
| Hindgut |
|
||
| ɸ -Except lower rectum, which drains into the systemic circulation. | |||

Source: By Anpol42 (Own work) [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons
Pathogenesis
The pathogenesis of lower gastrointestinal bleeding can be discussed based on the etiology. Diverticulosis is the most common etiology of lower GI bleeding accounting for 30% of all cases, followed by anorectal disease, ischemia, inflammatory bowel disease (IBD), neoplasia, and arteriovenous (AV) malformations.
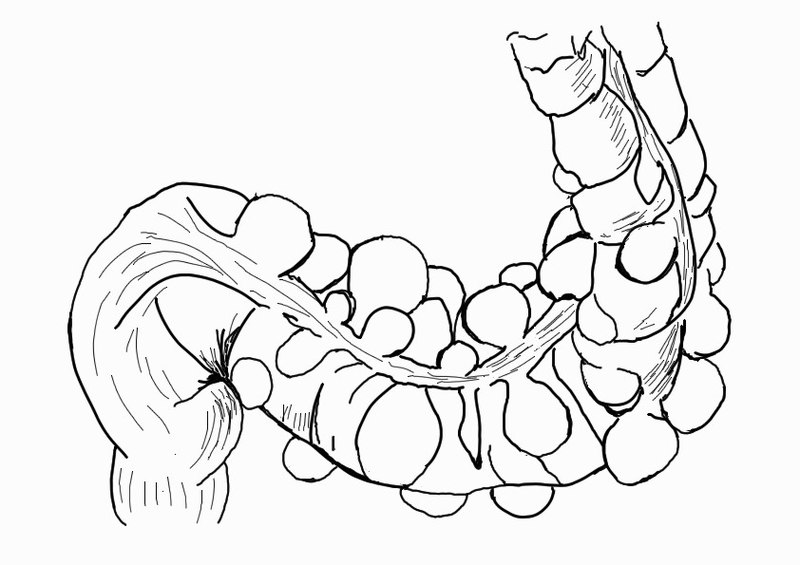
- Diverticulosis
- The colonic wall weakens with age and results in the formation of sac-like protrusions known as diverticula.[4][5][6][7]
- These protrusions generally occur at the junction of blood vessel penetrating through the mucosa and circular muscle fibers of the colon.
- Hemorrhage results from rupture of the intramural branches (vasa recta) of the marginal artery at the dome of a diverticulum and can give rise to a massive, life-threatening LGIB.
- Despite the majority of diverticula being on the left side of the colon, diverticular bleeding originates from the right side of the colon in 50% to 90% of instances.
Source:By Anpol42 (Own work) [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons
- Anorectal disease
- Hemorrhoids are engorged vessels in the normal anal cushions. When swollen, this tissue is very friable and susceptible to trauma, which leads to painless, bright red bleeding.[8][9][8]
- Anal fissures are defined as a tear in the anal mucosa. With the passage of stool, the mucosa continues to tear and leads to bright red bleeding. [10]
- Mesenteric ischemia results when there is inadequate blood supply at the level of the small intestine.[11][12][13][14]
- 2 or more vessels (celiac, SMA, or IMA) must be involved for bleeding to occur.
- Non occlusive mesenteric ischemia affects critically ill patients who are vasopressor-dependent.
- Venous thrombosis of the visceral vessels can also precipitate an acute ischemic event.
- Decreased blood flow leads to transmural infarction with necrosis and perforation.
- Associated mucosal sloughing results in bleeding.
- Ischemic colitis is caused by poor perfusion of the colon, which results in the inability of that area of the colon to meet its metabolic demands.[15][16][17]
- It can be gangrenous or nongangrenous, acute or chronic, transient or permanent.
- The left colon is predominantly affected, with the splenic flexure having increased susceptibility.
- Intraluminal hemorrhage occurs as the mucosa becomes necrotic, sloughs, and bleeds.
- Damage to the tissue is caused both with the ischemic insult as well as reperfusion injury.
- Inflammatory Bowel Disease[18][19]
- Crohn's disease
- In Crohn's disease, T cell activation stimulates interleukin (IL)-12 and tumor necrosis factor (TNF)-α, resulting in chronic inflammation and tissue injury.[20][21][22][23][24][25]
- Initially, inflammation starts focally around the crypts, followed by superficial ulceration of the mucosa.
- The deep mucosal layers are then invaded in a noncontinuous fashion, and noncaseating granulomas form, which can invade through the entire thickness of the bowel wall and into the mesentery and surrounding structures resulting in bleeding.
- Crohn's disease
- Ulcerative colitis
- In ulcerative colitis, T cells, cytotoxic to the colonic epithelium, accumulate in the lamina propria, accompanied by B cells that secrete immunoglobulin G (IgG) and IgE.[23][26][27][28]
- This results in inflammation of the crypts of Lieberkuhn, with abscesses and pseudopolyps along with rupturing of minute blood vessels in mucosa resulting in bleeding.
- Ulcerative colitis
- Neoplasia
- Mutations of multiple genes are required for the formation of adenocarcinoma, including the APC gene, Kras, DCC, and p53.[29][30][31]
- Certain hereditary syndromes are also classified by defects in DNA mismatch repair genes and microsatellite instability.
- As tumor grows it invades the surrounding tissue disrupting the normal vasculature along with it
- Therefore tumors tend to bleed slowly, and patients present with hemocult positive stools and microcytic anemia.
- AV Malformation/Angiodysplasia
- In AV malformation direct connections between arteries and veins occur in the colonic submucosa.[32][33][34][35][36]
- The lack of capillary buffers causes high pressure blood to enter directly into the venous system, making these vessels at high risk of rupture into the bowel lumen.
- In Angiodysplasia over time, previously healthy blood vessels of the cecum and ascending colon degenerate and become prone to bleeding.
Associated Conditions
Other diseases that are commonly associated with lower gastrointestinal bleeding include:
- Aortoenteric fistula
- Abdominal aortic aneurysms
- Peutz-Jeghers syndrome
- Klippel-Trenaunay-Weber syndrome
- Hereditary hemorrhagic telangiectasia
- Neurofibromatosis
- Blue rubber bleb syndrome
Gross and Microscopic Pathology
| Disease | Gross Pathology | Microscopic Pathology |
|---|---|---|
| Diverticulosis[37] |
|
|
| Angiodysplasia[38] |
|
|
| Hemorrhoids[8] |
|
|
| Mesenteric ischemia [39] |
|
|
| Ischemic colitis[39] |
|
|
| Crohn's disease[40][41] |
|
|
| Ulcerative colitis[42] |
|
|
References
- ↑ Geboes K, Geboes KP, Maleux G (2001). "Vascular anatomy of the gastrointestinal tract". Best Pract Res Clin Gastroenterol. 15 (1): 1–14. doi:10.1053/bega.2000.0152. PMID 11355897.
- ↑ Granger DN, Holm L, Kvietys P (2015). "The Gastrointestinal Circulation: Physiology and Pathophysiology". Compr Physiol. 5 (3): 1541–83. doi:10.1002/cphy.c150007. PMID 26140727.
- ↑ "The Gastrointestinal Circulation - NCBI Bookshelf".
- ↑ Hobson KG, Roberts PL (2004). "Etiology and pathophysiology of diverticular disease". Clin Colon Rectal Surg. 17 (3): 147–53. doi:10.1055/s-2004-832695. PMC 2780060. PMID 20011269.
- ↑ Maykel JA, Opelka FG (2004). "Colonic diverticulosis and diverticular hemorrhage". Clin Colon Rectal Surg. 17 (3): 195–204. doi:10.1055/s-2004-832702. PMC 2780065. PMID 20011276.
- ↑ Comparato G, Pilotto A, Franzè A, Franceschi M, Di Mario F (2007). "Diverticular disease in the elderly". Dig Dis. 25 (2): 151–9. doi:10.1159/000099480. PMID 17468551.
- ↑ Matrana MR, Margolin DA (2009). "Epidemiology and pathophysiology of diverticular disease". Clin Colon Rectal Surg. 22 (3): 141–6. doi:10.1055/s-0029-1236157. PMC 2780269. PMID 20676256.
- ↑ 8.0 8.1 8.2 Lohsiriwat V (2012). "Hemorrhoids: from basic pathophysiology to clinical management". World J. Gastroenterol. 18 (17): 2009–17. doi:10.3748/wjg.v18.i17.2009. PMC 3342598. PMID 22563187.
- ↑ Sanchez C, Chinn BT (2011). "Hemorrhoids". Clin Colon Rectal Surg. 24 (1): 5–13. doi:10.1055/s-0031-1272818. PMC 3140328. PMID 22379400.
- ↑ Holland RA, Rimes AF, Comis A, Tyndale-Biscoe CH (1988). "Oxygen carriage and carbonic anhydrase activity in the blood of a marsupial, the Tammar wallaby (Macropus eugenii), during early development". Respir Physiol. 73 (1): 69–86. PMID 3140330.
- ↑ Krupski WC, Selzman CH, Whitehill TA (1997). "Unusual causes of mesenteric ischemia". Surg. Clin. North Am. 77 (2): 471–502. PMID 9146726.
- ↑ Walker TG (2009). "Mesenteric ischemia". Semin Intervent Radiol. 26 (3): 175–83. doi:10.1055/s-0029-1225662. PMC 3036494. PMID 21326562.
- ↑ Berland T, Oldenburg WA (2008). "Acute mesenteric ischemia". Curr Gastroenterol Rep. 10 (3): 341–6. PMID 18625147.
- ↑ Mastoraki A, Mastoraki S, Tziava E, Touloumi S, Krinos N, Danias N, Lazaris A, Arkadopoulos N (2016). "Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities". World J Gastrointest Pathophysiol. 7 (1): 125–30. doi:10.4291/wjgp.v7.i1.125. PMC 4753178. PMID 26909235.
- ↑ FitzGerald JF, Hernandez Iii LO (2015). "Ischemic colitis". Clin Colon Rectal Surg. 28 (2): 93–8. doi:10.1055/s-0035-1549099. PMC 4442720. PMID 26034405.
- ↑ Theodoropoulou A, Koutroubakis IE (2008). "Ischemic colitis: clinical practice in diagnosis and treatment". World J. Gastroenterol. 14 (48): 7302–8. PMC 2778113. PMID 19109863.
- ↑ Rania H, Mériam S, Rym E, Hyafa R, Amine A, Najet BH, Lassad G, Mohamed TK (2014). "Ischemic colitis in five points: an update 2013". Tunis Med. 92 (5): 299–303. PMID 25504381.
- ↑ Kim DH, Cheon JH (2017). "Pathogenesis of Inflammatory Bowel Disease and Recent Advances in Biologic Therapies". Immune Netw. 17 (1): 25–40. doi:10.4110/in.2017.17.1.25. PMC 5334120. PMID 28261018.
- ↑ Hendrickson BA, Gokhale R, Cho JH (2002). "Clinical aspects and pathophysiology of inflammatory bowel disease". Clin. Microbiol. Rev. 15 (1): 79–94. PMC 118061. PMID 11781268.
- ↑ Woźniak-Parnowska W, Werakso B (1974). "[Comparative studies of microbiological purity of ointments by the direct culture method and use of membrane filters]". Acta Pol Pharm (in Polish). 31 (6): 819–23. PMID 4447044.
- ↑ Mazal J (2014). "Crohn disease: pathophysiology, diagnosis, and treatment". Radiol Technol. 85 (3): 297–316, quiz 317–20. PMID 24395894.
- ↑ Jewell DP (1989). "Aetiology and pathogenesis of ulcerative colitis and Crohn's disease". Postgrad Med J. 65 (768): 718–9. PMC 2429831. PMID 2694136.
- ↑ 23.0 23.1 Sartor RB (2006). "Mechanisms of disease: pathogenesis of Crohn's disease and ulcerative colitis". Nat Clin Pract Gastroenterol Hepatol. 3 (7): 390–407. doi:10.1038/ncpgasthep0528. PMID 16819502.
- ↑ Head K, Jurenka JS (2004). "Inflammatory bowel disease. Part II: Crohn's disease--pathophysiology and conventional and alternative treatment options". Altern Med Rev. 9 (4): 360–401. PMID 15656711.
- ↑ Zhang YZ, Li YY (2014). "Inflammatory bowel disease: pathogenesis". World J. Gastroenterol. 20 (1): 91–9. doi:10.3748/wjg.v20.i1.91. PMC 3886036. PMID 24415861.
- ↑ Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF (2017). "Ulcerative colitis". Lancet. 389 (10080): 1756–1770. doi:10.1016/S0140-6736(16)32126-2. PMID 27914657.
- ↑ Farrell RJ, Peppercorn MA (2002). "Ulcerative colitis". Lancet. 359 (9303): 331–40. doi:10.1016/S0140-6736(02)07499-8. PMID 11830216.
- ↑ Rönnblom LE, Janson ET, Perers A, Oberg KE, Alm GV (1992). "Characterization of anti-interferon-alpha antibodies appearing during recombinant interferon-alpha 2a treatment". Clin. Exp. Immunol. 89 (3): 330–5. PMC 1554468. PMID 1516252.
- ↑ Itzkowitz S (2003). "Colon carcinogenesis in inflammatory bowel disease: applying molecular genetics to clinical practice". J. Clin. Gastroenterol. 36 (5 Suppl): S70–4, discussion S94–6. PMID 12702969.
- ↑ Ullman TA, Itzkowitz SH (2011). "Intestinal inflammation and cancer". Gastroenterology. 140 (6): 1807–16. doi:10.1053/j.gastro.2011.01.057. PMID 21530747.
- ↑ Kraus S, Arber N (2009). "Inflammation and colorectal cancer". Curr Opin Pharmacol. 9 (4): 405–10. doi:10.1016/j.coph.2009.06.006. PMID 19589728.
- ↑ Foutch PG (1993). "Angiodysplasia of the gastrointestinal tract". Am. J. Gastroenterol. 88 (6): 807–18. PMID 8389094.
- ↑ Dodda G, Trotman BW (1997). "Gastrointestinal angiodysplasia". J Assoc Acad Minor Phys. 8 (1): 16–9. PMID 9048468.
- ↑ Kheterpal S (1991). "Angiodysplasia: a review". J R Soc Med. 84 (10): 615–8. PMC 1295562. PMID 1744847.
- ↑ Athanasoulis CA, Galdabini JJ, Waltman AC, Novelline RA, Greenfield AJ, Ezpeleta ML (1977). "Angiodysplasia of the colon: a cause of rectal bleeding". Cardiovasc Radiol. 1 (1): 3–13. PMID 311247.
- ↑ Sami SS, Al-Araji SA, Ragunath K (2014). "Review article: gastrointestinal angiodysplasia - pathogenesis, diagnosis and management". Aliment. Pharmacol. Ther. 39 (1): 15–34. doi:10.1111/apt.12527. PMID 24138285.
- ↑ West AB, Losada M (2004). "The pathology of diverticulosis coli". J. Clin. Gastroenterol. 38 (5 Suppl 1): S11–6. PMID 15115923.
- ↑ Stamm B, Heer M, Bühler H, Ammann R (1985). "Mucosal biopsy of vascular ectasia (angiodysplasia) of the large bowel detected during routine colonoscopic examination". Histopathology. 9 (6): 639–46. PMID 4029903.
- ↑ 39.0 39.1 Mitsudo S, Brandt LJ (1992). "Pathology of intestinal ischemia". Surg. Clin. North Am. 72 (1): 43–63. PMID 1731389.
- ↑ Price AB, Morson BC (1975). "Inflammatory bowel disease: the surgical pathology of Crohn's disease and ulcerative colitis". Hum. Pathol. 6 (1): 7–29. PMID 1089084.
- ↑ Wright CL, Riddell RH (1998). "Histology of the stomach and duodenum in Crohn's disease". Am. J. Surg. Pathol. 22 (4): 383–90. PMID 9537465.
- ↑ DeRoche TC, Xiao SY, Liu X (2014). "Histological evaluation in ulcerative colitis". Gastroenterol Rep (Oxf). 2 (3): 178–92. doi:10.1093/gastro/gou031. PMC 4124271. PMID 24942757.