ABO blood group system: Difference between revisions
No edit summary |
Matt Pijoan (talk | contribs) m (1 revision imported) |
||
| (7 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
{{ | {{Redirect|ABO}} | ||
{{Redirect|H substance|use in inflammation|histamine|hydrogen atom|hydrogen}} | |||
{{Use dmy dates|date=April 2014}} | |||
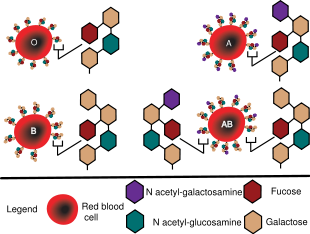
[[File:ABO blood type.svg|thumb|right|410px|ABO blood group [[antigen]]s present on [[red blood cell]]s and [[IgM]] [[antibodies]] present in the [[Blood serum|serum]]]] | |||
{{ | The '''ABO blood group system''' is used to denote the presence of one, both, or neither of the A and B [[antigen]]s on [[erythrocyte]]s.<ref name=britannica>{{cite web |url=https://www.britannica.com/science/ABO-blood-group-system |title=ABO blood group system |last=The Editors of Encyclopædia Britannica |date=2017-07-18 |website=Encyclopædia Britannica |publisher=Encyclopædia Britannica, Inc. |access-date=2017-10-26 |quote=}}</ref> In human [[blood transfusion]]s it is the most important of the 36 different [[blood type]] (or group) classification systems currently recognized.<ref name=ISBT16>{{cite journal |last1=Storry |first1=J. R. |last2=Castilho |first2=L. |last3=Chen |first3=Q. |last4=Daniels |first4=G. |last5=Denomme |first5=G. |last6=Flegel |first6=W. A. |last7=Gassner |first7=C. |last8=de Haas |first8=M. |last9=Hyland |first9=C. |last10=Keller |first10=M. |last11=Lomas-Francis |first11=C. |last12=Moulds |first12=J. M. |last13=Nogues |first13=N. |last14=Olsson |first14=M. L. |last15=Peyrard |first15=T. |last16=van der Schoot |first16=C. E. |last17=Tani |first17=Y. |last18=Thornton |first18=N. |last19=Wagner |first19=F. |last20=Wendel |first20=S. |last21=Westhoff |first21=C. |last22=Yahalom |first22=V. |title=International society of blood transfusion working party on red cell immunogenetics and terminology: report of the Seoul and London meetings |journal=ISBT Science Series |date=2016 |volume=11 |issue=2 |pages=118–122 |doi=10.1111/voxs.12280 |pmid=29093749 |pmc=5662010 |display-authors=8}}</ref> A very rare (in modern medicine) mismatch in this, or any other [[serotype]], can cause a serious, potentially fatal, [[Blood transfusion#Adverse effects|adverse reaction]] after a transfusion, or a contra-indicated immune response to an [[Organ transplantation|organ transplant]].<ref name="pmid11532188">{{cite journal |vauthors=Muramatsu M, Gonzalez HD, Cacciola R, Aikawa A, Yaqoob MM, Puliatti C | title=ABO incompatible renal transplants: Good or bad? | journal= World Journal of Transplantation | volume=4 | issue=1 | year=2014 | pages=18–29 | url=http://www.wjgnet.com/2220-3230/full/v4/i1/18.htm | doi=10.5500/wjt.v4.i1.18 | pmid=24669364 | pmc=3964193}}</ref> The associated anti-A and anti-B [[antibodies]] are usually [[IgM]] antibodies, which are produced in the first years of life by sensitization to environmental substances, such as food, bacteria, and viruses. | ||
The ABO blood types were discovered by [[Karl Landsteiner]] in 1901, for which he received the Nobel Prize in Physiology or Medicine in 1930. ABO blood types are also present in some other [[Blood type (non-human)|animals]] such as [[rodents]] and [[ape]]s, including [[chimpanzee]]s, [[bonobo]]s, and [[gorilla]]s.<ref>{{cite book| last1 = Maton|first1=Anthea| author2= Jean Hopkins| author3= Charles William McLaughlin| author4= Susan Johnson| author5= Maryanna Quon Warner| author6= David LaHart| author7= Jill D. Wright|title=Human Biology and Health|publisher=Prentice Hall|year = 1993|location = Englewood Cliffs, New Jersey, USA|isbn = 978-0-13-981176-0}}</ref> | |||
The | |||
== | == History== | ||
[[ | [[File:Karl Landsteiner, 1920s..jpg|thumb|right| Karl Landsteiner, discoverer of ABO blood system.]] | ||
The ABO blood types were first discovered by an Austrian Physician [[Karl Landsteiner]] working at the Pathological-Anatomical Institute of the University of Vienna (now [[Medical University of Vienna]]). In 1900, he found that blood sera from different persons would clump together ([[Agglutination (biology)|agglutinate]]) when mixed in test tubes, and not only that some human blood also agglutinated with animal blood.<ref>{{cite journal |author=Landsteiner K |title=Zur Kenntnis der antifermentativen, lytischen und agglutinierenden Wirkungen des Blutserums und der Lymphe |journal=Zentralblatt für Bakteriologie, Parasitenkunde und Infektionskrankheiten|volume=27 |issue= |pages=357–362 |year=1900}}</ref> He wrote a two-sentence footnote: | |||
{{Quote|The serum of healthy human beings not only agglutinates animal red cells, but also often those of human origin, from other individuals. It remains to be seen whether this appearance is related to inborn differences between individuals or it is the result of some damage of bacterial kind.<ref name=kantha>{{cite journal |last1=Kantha |first1=S.S. |title=The blood revolution initiated by the famous footnote of Karl Landsteiner's 1900 paper |journal=The Ceylon Medical Journal |date=1995 |volume=40 |issue=3 |pages=123–125 |pmid=8536328 |url=https://www1.gifu-u.ac.jp/~srikanth/srikantha_library/file/History%20of%20science/Landsteiner%20blood%20revolution%201995.pdf}}</ref>}} | |||
This was the first evidence that blood variation exists in humans – it was believed that all humans have similar blood. The next year, in 1901, he made a definitive observation that blood serum of an individual would agglutinate with only those of certain individuals. Based on this he classified human bloods into three groups, namely group A, group B, and group C. He defined that group A blood agglutinates with group B, but never with its own type. Similarly, group B blood agglutinates with group A. Group C blood is different in that it agglutinates with both A and B.<ref name=land01>{{cite journal |last1=Landsteiner |first1=Karl |title=On Agglutination of Normal Human Blood |journal=Transfusion |date=1961 |volume=1 |issue=1 |pages=5–8 |doi=10.1111/j.1537-2995.1961.tb00005.x |orig-year=1901 |pmid=13758692| postscript=Originally published in German in ''Wiener Klinische Wochenschrift'', '''46''', 1132–1134}}</ref> This was the discovery of blood groups for which Landsteiner was awarded the Nobel Prize in Physiology or Medicine in 1930. In his paper, he called the specific blood group interactions as isoagglutination, and also introduced the concept of agglutinins (antibodies), which is the actual basis of [[Antigen-antibody interaction|antigen-antibody reaction]] in ABO system.<ref name=durand>{{cite journal |last1=Durand |first1=J.K. |last2=Willis |first2=M.S. |title=Karl Landsteiner, MD: Transfusion Medicine |journal=Laboratory Medicine |date=2010 |volume=41 |issue=1 |pages=53–55 |doi=10.1309/LM0MICLH4GG3QNDC}}</ref> He asserted: | |||
{{Quote|[It] may be said that there exist at least two different types of agglutinins, one in A, another one in B, and both together | |||
in C. The red blood cells are inert to the agglutinins which are present in the same serum.<ref name=land01/>}} | |||
Thus, he discovered two antigens (agglutinogens A and B) and two antibodies (agglutinins - anti-A and anti-B). His third group (C) indicated absence of both A and B antigens, but contains anti-A and anti-B.<ref name=durand/> The following year, his students Adriano Sturli and Alfred von Decastello discovered the fourth type (but not naming it, and simply referred to it as "no particular type”).<ref>{{cite journal |last1=Von Decastello |first1=A. |last2=Sturli |first2=A. |title=Concerning isoagglutinins in serum of healthy and sick humans |journal=Munchener Medizinische Wochenschrift |date=1902 |volume=26 |pages=1090–1095}}</ref><ref name="Farr1979">{{cite journal |author=Farr AD |title=Blood group serology—the first four decades (1900–1939) |journal=Medical History |volume=23 |issue=2 |pages=215–26 |date=April 1979 |pmid=381816 |pmc=1082436 |doi=10.1017/s0025727300051383}}</ref> | |||
[[File:UkrArmyBloodGroupIII+2000s.jpg|thumb|[[Ukraine]] marine uniform imprint, showing the wearer's blood type as "B (III) Rh+".]] | |||
In 1910, [[Ludwik Hirszfeld]] and [[Emil Freiherr von Dungern]] introduced the term 0 (null) for the group Landsteiner designated as C, and AB for the type discovered by Sturli and von Decastello. They were also the first to explain the genetic inheritance of the blood groups.<ref name="farhud">{{cite journal |last1=Farhud |first1=D.D. |last2=Zarif Yeganeh |first2=M. |title=A brief history of human blood groups |journal=Iranian Journal of Public Health |date=2013 |volume=42 |issue=1 |pages=1–6 |pmid=23514954 |pmc=3595629}}</ref>) | |||
[[File:Jan Janský, 1902.jpg|thumb|upright|Jan Janský, who invented type I, II, III, IV system.]] | |||
Czech serologist [[Jan Janský]] independently introduced blood type classification in 1907 in a local journal.<ref name="Janský_1907">{{cite journal| author = Janský J.| title = Haematologick studie u. psychotiku | journal = Sborn. Klinick | language = Czech | year = 1907 | volume = 8 | pages = 85–139 | url= }}</ref> He used the Roman numerical I, II, III, and IV (corresponding to modern O, A, B, and AB). Unbeknown to Janský, an American physician William L. Moss devised a slightly different classification using the same numerical;<ref name=Moss_1910>{{cite journal| author = Moss W.L. | title = Studies on isoagglutinins and isohemolysins | journal = Bulletin of Johns Hopkins Hospital | year = 1910 | volume = 21 | pages = 63–70}}</ref> his I, II, III, and IV corresponding to modern AB, A, B, and O.<ref name="Farr1979"/> These two systems created confusion and potential danger in medical practice. Moss's system was adopted in Britain, France, and US, while Janský's was preferred in most European countries and some parts of US. To resolve the chaos, the [[American Association of Immunologists]], the [[American Society for Microbiology|Society of American Bacteriologists]], and the Association of Pathologists and Bacteriologists made a joint recommendation in 1921 that the Jansky classification be adopted based on priority.<ref>{{cite journal |last1=Doan |first1=C.A. |title=The Transfusion problem |journal=Physiological Reviews |date=1927 |volume=7 |issue=1 |pages=1–84 |doi=10.1152/physrev.1927.7.1.1}}</ref> But it was not followed particularly where Moss's system had been used. In 1927, Landsteiner, who had moved to the [[Rockefeller University|Rockefeller Institute for Medical Research]] in New York, and as a member of a committee of the [[National Research Council (United States)|National Research Council]] concerned with blood grouping suggested to substitute Janský's and Moss's systems with the letters 0, A, B, and AB. (There was another confusion on the use of figure 0 for German ''null'' as introduced by Hirszfeld and von Dungern, because others used the letter O for ''ohne'', meaning without or zero; Landsteiner chose the latter.<ref>{{cite journal |last1=Schmidt |first1=P. |last2=Okroi |first2=M. |title=Also sprach Landsteiner – Blood Group 'O' or Blood Group 'NULL' |journal=Transfusion Medicine and Hemotherapy |date=2001 |volume=28 |issue=4 |pages=206–208 |doi=10.1159/000050239}}</ref>) This classification was adopted by the National Research Council and became variously known as the National Research Council classification, the International classification, and most popularly the "new" Landsteiner classification. The new system was gradually accepted and by the early 1950s, it was universally followed.<ref>{{cite journal |last1=Garratty |first1=G. |last2=Dzik |first2=W. |last3=Issitt |first3=P.D. |last4=Lublin |first4=D.M. |last5=Reid |first5=M.E. |last6=Zelinski |first6=T. |title=Terminology for blood group antigens and genes-historical origins and guidelines in the new millennium |journal=Transfusion |date=2000 |volume=40 |issue=4 |pages=477–489 |doi=10.1046/j.1537-2995.2000.40040477.x |pmid=10773062}}</ref> | |||
= | The first practical use of blood typing in transfusion was by an American physician [[Reuben Ottenberg]] in 1907. And the large-scale application started during the First World War (1914-1915) when [[citric acid]] was developed as [[Anticoagulant|blood clot prevention]].<ref name=durand/> [[Felix Bernstein (mathematician)|Felix Bernstein]] demonstrated the correct blood group inheritance pattern of multiple [[allele]]s at one locus in 1924.<ref name="Crow">{{cite journal|author=Crow J |title=Felix Bernstein and the first human marker locus |journal=Genetics |volume=133 |issue=1 |pages=4–7 |year=1993 |pmid=8417988 |pmc=1205297}}</ref> Watkins and Morgan, in England, discovered that the ABO [[epitope]]s were conferred by sugars, to be specific, N-acetylgalactosamine for the A-type and galactose for the B-type.<ref>{{cite journal | last1 = Morgan | first1 = W. T. J. | last2 = Watkins | first2 = W. M | year = 1969 | title = Genetic and biochemical aspects of human blood-group A-, B-, H-, Le-a- and Le-b-specificity| url = | journal = Br. Med. Bull. | volume = 25 | issue = 1| pages = 30–34 | pmid = 5782756 }}</ref><ref>Watkins, W. M. ''Advances in Human Genetics'' Vol. 10 (eds Harris, H. & Hirschhorn, K.) 1–136 (Plenum, New York, 1980)</ref><ref>{{cite journal | last1 = Watkins | first1 = W. M. | last2 = Morgan | first2 = W. T. J. | year = 1959 | title = Possible Genetical Pathways for the Biosynthesis of Blood Group Mucopolysaccharides| doi = 10.1111/j.1423-0410.1959.tb04023.x | pmid = 13669421 | journal = Vox Sang. | volume = 4 | issue = 2| pages = 97–119 }}</ref> After much published literature claiming that the ABH substances were all attached to glycosphingolipids, Finne ''et al''. (1978) found that the human erythrocyte glycoproteins contain polylactosamine chains<ref>{{cite journal | last1 = Finne | last2 = Krusius | last3 = Rauvala | last4 = Kekomäki | last5 = Myllylä | year = 1978 | title = Alkali-stable blood group A- and B-active poly(glycosyl)-peptides from human erythrocyte membrane| doi = 10.1016/0014-5793(78)80534-1 | journal = FEBS Left. | volume = 89 | issue = | pages = 111–115 }}</ref> that contains ABH substances attached and represent the majority of the antigens.<ref>{{cite journal | last1 = Krusius | last2 = Finne | last3 = Rauvala | year = 1978 | title = The Poly(glycosyl) Chains of Glycoproteins.. Characterisation of a Novel Type of Glycoprotein Saccharides from Human Erythrocyte Membrane| url = | journal = Eur. J. Biochem. | volume = 92 | issue = 1| pages = 289–300 | doi=10.1111/j.1432-1033.1978.tb12747.x| pmid = 729592}}</ref><ref>{{cite journal | last1 = Järnefelt | last2 = Rush | last3 = Li | last4 = Laine | year = 1978 | title = Erythroglycan, a high molecular weight glycopeptide with the repeating structure [galactosyl-(1 leads to 4)-2-deoxy-2-acetamido-glucosyl(1 leads to 3)] comprising more than one-third of the protein-bound carbohydrate of human erythrocyte stroma| url = | journal = J. Biol. Chem. | volume = 253 | issue = 22| pages = 8006–8009 | pmid = 711733 }}</ref><ref>Laine and Rush in ''Molecular Immunology of Complex Carbohydrates'' (A. Wu, E. Kabat, Eds.) Plenum Publishing Corporation, N.Y. NY (1988)</ref> The main glycoproteins carrying the ABH antigens were identified to be the Band 3 and Band 4.5 proteins and glycophorin.<ref>{{cite journal | last1 = Finne | year = 1980 | title = Identification of the Blood-Group ABH-Active Glycoprotein Components of Human Erythrocyte Membrane| url = | journal = Eur. J. Biochem. | volume = 104 | issue = | pages = 181–189 | doi=10.1111/j.1432-1033.1980.tb04414.x}}</ref> Later, Yamamoto's group showed the precise glycosyl transferase set that confers the A, B and O epitopes.<ref>{{cite journal | last1 = Yamamoto | display-authors = etal | year = 1990 | title = Molecular genetic basis of the histo-blood group ABO system | url = | journal = Nature | volume = 345 | issue = 6272| pages = 229–233 | doi=10.1038/345229a0 | pmid=2333095| bibcode = 1990Natur.345..229Y}}</ref> | ||
[[ | |||
[[File:ABO blood group diagram.svg|thumb|right|310px|Diagram showing the carbohydrate chains that determine the ABO blood group]] | |||
{{cite journal | [[File:Type A blood.png|frame|Student blood test. Three drops of blood are mixed with anti-B (left) and anti-A (right) serum. | ||
[[Agglutination (biology)|Agglutination]] on the right side indicates blood type A.]] | |||
[[File:AP-Biology Final Project.svg|thumb|There are three basic variants of immunoglobulin antigens in humans that share a very similar chemical structure but are distinctly different. Red circles show where there are differences in chemical structure in the antigen-binding site (sometimes called the antibody-combining site) of human immunoglobulin. Notice the O-type antigen does not have a binding site.<ref>{{cite journal|last1=Hara|first1=Atsushi|last2=Imamura|first2=Akihiro|last3=Ando|first3=Hiromune|last4=Ishida|first4=Hideharu|last5=Kiso|first5=Makoto|title=A New Chemical Approach to Human ABO Histo-Blood Group Type 2 Antigens|journal=Molecules|date=31 December 2013|volume=19|issue=1|pages=414–437|doi=10.3390/molecules19010414|pmid=24384923}}<!--|accessdate=31 May 2016--></ref> | |||
]] | |||
</ref> | |||
== Genetics == | |||
[[File:ABO system codominance.svg|280px|thumb|left|A and B are [[Dominance relationship#Co-dominance|codominant]], giving the AB [[phenotype]].]] | |||
== | Blood groups are inherited from both parents. The ABO blood type is controlled by a single [[gene]] (the [[ABO (gene)|ABO gene]]) with three types of [[allele]]s inferred from [[classical genetics]]: ''i'', ''I<sup>A</sup>'', and ''I<sup>B</sup>''. The ''I'' designation stands for '''isoagglutinogen''', another term for [[antigen]].<ref>{{cite book|last1=Klug|first1=William S.|last2=Cummings|first2=Michael R.|title=Concepts of Genetics|date=1997|publisher=Prentice Hall|location=Upper Saddle River, NJ|isbn=978-0135310625|page=83|edition=5th}}</ref> The gene encodes a [[glycosyltransferase]]—that is, an [[enzyme]] that modifies the [[carbohydrate]] content of the [[red blood cell]] antigens. The gene is located on the long arm of the [[Chromosome 9 (human)|ninth chromosome]] (9q34). | ||
The ''I<sup>A</sup>'' allele gives type A, ''I<sup>B</sup>'' gives type B, and ''i'' gives type O. As both ''I<sup>A</sup>'' and ''I<sup>B</sup>'' are dominant over ''i'', only ''ii'' people have type O blood. Individuals with ''I<sup>A</sup>I<sup>A</sup>'' or ''I<sup>A</sup>i'' have type A blood, and individuals with ''I<sup>B</sup>I<sup>B</sup>'' or ''I<sup>B</sup>i'' have type B. ''I<sup>A</sup>I<sup>B</sup>'' people have both [[phenotype]]s, because A and B express a special dominance relationship: [[Dominance relationship#Co-dominance|codominance]], which means that type A and B parents can have an AB child. A couple with type A and type B can also have a type O child if they are both heterozygous (''I<sup>B</sup>i'',''I<sup>A</sup>i''). The ''[[Cis AB|cis-AB]]'' phenotype has a single enzyme that creates both A and B antigens. The resulting red blood cells do not usually express A or B antigen at the same level that would be expected on common group A<sub>1</sub> or B red blood cells, which can help solve the problem of an apparently genetically impossible blood group.<ref name="Yazer=2006">{{cite journal|vauthors=Yazer M, Olsson M, Palcic M |title=The cis-AB blood group phenotype: fundamental lessons in glycobiology |journal=Transfus Med Rev |volume=20 |issue=3 |pages=207–17 |year=2006 |pmid=16787828 |doi=10.1016/j.tmrv.2006.03.002}}</ref> | |||
== Inheritance == | {| class="wikitable" cellpadding="10" style="border:darkgrey; float:right; margin-left:20px; text-align:center;" | ||
|- | |||
| colspan="8" |'''Blood group inheritance''' | |||
|- | |||
! scope="col" style="width:100px; border-top:2px solid black; border-left:2px solid black;"|Blood type | |||
! scope="col" style="width:100px; border-top:2px solid black; border-bottom:2px solid black;"| | |||
! scope="col" style="width:100px; background:#aaa; border-top:2px solid black; border-bottom:2px solid black;"| '''O''' | |||
! scope="col" style="width:200px; background:#ff8888; border-top:2px solid black; border-bottom:2px solid black;" colspan="2"|'''A''' | |||
! scope="col" style="width:200px; background:#8888ff; border-top:2px solid black; border-bottom:2px solid black;" colspan="2"|'''B''' | |||
! scope="col" style="width:100px; background:#f0f; border-top:2px solid black; border-bottom:2px solid black; border-right:2px solid black;"| '''AB''' | |||
|- | |||
! style="border-left:2px solid black;border-right:2px solid black;" | | |||
! scope="col" style="width:100px;"|Genotype | |||
! scope="col" style="width:100px; background:#aaa; border-bottom:2px solid black;"|'''''ii'' <small>(OO)</small>''' | |||
! scope="col" style="width:100px; background:#ff8888; border-bottom:2px solid black;"|'''''I<sup>A</sup>i'' <small>(AO)</small>''' | |||
! scope="col" style="width:100px; background:red; border-bottom:2px solid black;"|'''''I<sup>A</sup>I<sup>A</sup>'' <small>(AA)</small>''' | |||
! scope="col" style="width:100px; background:#8888ff; border-bottom:2px solid black;"|'''''I<sup>B</sup>i'' <small>(BO)</small>''' | |||
! scope="col" style="width:100px; background:blue; border-bottom:2px solid black;"|'''''I<sup>B</sup>I<sup>B</sup>'' <small>(BB)</small>''' | |||
! scope="col" style="width:100px; background:#f0f; border-bottom:2px solid black; border-right:2px solid black;"|'''''I<sup>A</sup>I<sup>B</sup>'' <small>(AB)</small>''' | |||
|- | |||
| style="background:#aaa; border-left:2px solid black; border-right:2px solid black;"| '''O''' | |||
| style="background:#aaa; border-right:2px solid black;"| '''''ii'' <small>(OO)</small>''' | |||
| style="background:#aaa;"| O<br /><small>OO OO OO OO</small> | |||
| style="background:#ff8888;"| O or A<br /><small>AO OO AO OO</small> | |||
| style="background:#ff8888;"| A<br /><small>AO AO AO AO</small> | |||
| style="background:#8888ff;"| O or B<br /><small>BO OO BO OO</small> | |||
| style="background:#8888ff;"| B<br /><small>BO BO BO BO</small> | |||
| style="background:#ff88ff;"| A or B<br /><small>AO BO AO BO</small> | |||
|- | |||
| rowspan="2" style="background:#ff8888; border-left:2px solid black; border-right:2px solid black;"| '''A''' | |||
| style="background:#ff8888; border-right:2px solid black;"| '''''I<sup>A</sup>i'' <small>(AO)</small>''' | |||
| style="background:#ff8888;"| O or A<br /><small>AO AO OO OO</small> | |||
| style="background:#ff8888;"| O or A<br /><small>AA AO AO OO</small> | |||
| style="background:#ff8888;"| A<br /><small>AA AA AO AO</small> | |||
| style="background:#ff88ff;"| O, A, B or AB<br /><small>AB AO BO OO</small> | |||
| style="background:#ff88ff;"| B or AB<br /><small>AB AB BO BO</small> | |||
| style="background:#ff88ff;"| A, B or AB<br /><small>AA AB AO BO </small> | |||
|- | |||
| style="background:red; border-right:2px solid black;"| '''''I<sup>A</sup>I<sup>A</sup>'' <small>(AA)</small>''' | |||
| style="background:#ff8888;"| A<br /><small>AO AO AO AO</small> | |||
| style="background:#ff8888;"| A<br /><small>AA AO AA AO</small> | |||
| style="background:red;"| A<br /><small>AA AA AA AA</small> | |||
| style="background:#ff88ff;"| A or AB<br /><small>AB AO AB AO</small> | |||
| style="background:#f0f;"| AB<br /><small>AB AB AB AB</small> | |||
| style="background:#f0f;"| A or AB<br /><small>AA AB AA AB</small> | |||
|- | |||
| rowspan="2" style="background:#8888ff; border-left:2px solid black; border-right:2px solid black;"| '''B''' | |||
| style="background:#8888ff; border-right:2px solid black;"| '''''I<sup>B</sup>i'' <small>(BO)</small>''' | |||
| style="background:#8888ff;"| O or B<br /><small>BO BO OO OO</small> | |||
| style="background:#ff88ff;"| O, A, B or AB<br /><small>AB BO AO OO</small> | |||
| style="background:#ff88ff;"| A or AB<br /><small>AB AB AO AO</small> | |||
| style="background:#8888ff;"| O or B<br /><small>BB BO BO OO</small> | |||
| style="background:#8888ff;"| B<br /><small>BB BB BO BO</small> | |||
| style="background:#ff88ff;"| A, B or AB<br /><small>AB BB AO BO</small> | |||
|- | |||
| style="background:blue; border-right:2px solid black;"| '''''I<sup>B</sup>I<sup>B</sup>'' <small>(BB)</small>''' | |||
| style="background:#8888ff;"| B<br /><small>BO BO BO BO</small> | |||
| style="background:#ff88ff;"| B or AB<br /><small>AB BO AB BO</small> | |||
| style="background:#f0f;"| AB<br /><small>AB AB AB AB</small> | |||
| style="background:#8888ff;"| B<br /><small>BB BO BB BO</small> | |||
| style="background:blue;"| B<br /><small>BB BB BB BB</small> | |||
| style="background:#f0f;"| B or AB<br /><small>AB BB AB BB</small> | |||
|- | |||
| style="background:#f0f; border-left:2px solid black; border-right:2px solid black; border-bottom:2px solid black;"| '''AB''' | |||
| style="background:#f0f; border-right:2px solid black; border-bottom:2px solid black;"| '''''I<sup>A</sup>I<sup>B</sup>'' <small>(AB)</small>''' | |||
| style="background:#ff88ff;"| A or B<br /><small>AO AO BO BO</small> | |||
| style="background:#ff88ff;"| A, B or AB<br /><small>AA AO AB BO</small> | |||
| style="background:#f0f;"| A or AB<br /><small>AA AA AB AB</small> | |||
| style="background:#ff88ff;"| A, B or AB<br /><small>AB AO BB BO</small> | |||
| style="background:#f0f;"| B or AB<br /><small>AB AB BB BB</small> | |||
| style="background:#f0f;"| A, B, or AB<br /><small>AA AB AB BB</small> | |||
|} | |||
{{clear}} | |||
The table above summarizes the various blood groups that children may inherit from their parents.<ref name=arcbs>{{cite web|title=ABO inheritance patterns|url=http://www.transfusion.com.au/?q=node/77|work=Inheritance patterns of blood groups|publisher=Australian Red Cross Blood Service|accessdate=30 October 2013}}</ref><ref>{{cite web|url=http://abobloodtypes.webnode.com/ |title=ABO blood group system |publisher=Abobloodtypes.webnode.com |date= |accessdate=2015-02-02}}</ref> Genotypes are shown in the second column and in small print for the offspring: AO and AA both test as type A; BO and BB test as type B. The four possibilities represent the combinations obtained when one allele is taken from each parent; each has a 25% chance, but some occur more than once. | |||
{| class="wikitable" cellpadding="10" style="border:darkgrey; float:right; margin-left:20px; text-align:center;" | |||
|- | |||
{| class = " | | colspan="5" |'''Blood group inheritance by phenotype only''' | ||
| colspan="5"|'''Blood group inheritance''' | |- | ||
! scope="col" style="width:200px; border-top:2px solid black; border-left:2px solid black;"|Blood type | |||
! scope="col" style="width:100px; background:#aaa; border-top:2px solid black; border-bottom:2px solid black;"| '''O''' | |||
! scope="col" style="width:200px; background:#ff8888; border-top:2px solid black; border-bottom:2px solid black;"|'''A''' | |||
! scope="col" style="width:200px; background:#8888ff; border-top:2px solid black; border-bottom:2px solid black;"|'''B''' | |||
! scope="col" style="width:100px; background:#f0f; border-top:2px solid black; border-bottom:2px solid black; border-right:2px solid black;"| '''AB''' | |||
|- | |||
| style="background:#aaa; border-left:2px solid black; border-right:2px solid black;"| '''O''' | |||
| style="background:#aaa;"| O | |||
| style="background:#ff8888;"| O or A | |||
| style="background:#8888ff;"| O or B | |||
| style="background:#ff88ff;"| A or B | |||
|- | |- | ||
| style="background:#ff8888; border-left:2px solid black; border-right:2px solid black;"| '''A''' | |||
| style="background:#ff8888;"| O or A | |||
| style="background:#ff8888;"| O or A | |||
| style="background:#ff88ff;"| O, A, B or AB | |||
| style="background:#ff88ff;"| A, B or AB | |||
|- | |- | ||
| style=" | | style="background:#8888ff; border-left:2px solid black; border-right:2px solid black;"| '''B''' | ||
| style="background:#8888ff;"| O or B | |||
| style="background:#ff88ff;"| O, A, B or AB | |||
| style="background:#8888ff;"| O or B | |||
| style="background:#ff88ff;"| A, B or AB | |||
|- | |- | ||
| style=" | | style="background:#f0f; border-left:2px solid black; border-right:2px solid black; border-bottom:2px solid black;"| '''AB''' | ||
| style="background:#ff88ff;"| A or B | |||
| style="background:#ff88ff;"| A, B or AB | |||
| style="background:#ff88ff;"| A, B or AB | |||
| style="background:#f0f;"| A, B or AB | |||
|} | |||
{{clear}} | |||
Historically, ABO blood tests were used in [[DNA paternity testing|paternity testing]], but in 1957 only 50% of American men falsely accused were able to use them as evidence against paternity.<ref>Cited in {{cite web|url=http://www.childsupportanalysis.co.uk/analysis_and_opinion/choices_and_behaviours/misattributed_paternity.htm|title=Misattributed paternity rates and non-paternity rates}}</ref> Occasionally, the blood types of children are not consistent with expectations—for example, a type O child can be born to an AB parent—due to rare situations, such as [[Bombay phenotype]] and [[cis AB]].<ref>{{cite web|url=http://genetics.thetech.org/ask/ask221|title=Understanding genetics|publisher=Stanford}}</ref> | |||
=== Subgroups === | |||
The A blood type contains about 20 subgroups, of which A1 and A2 are the most common (over 99%). A1 makes up about 80% of all A-type blood, with A2 making up almost all of the rest.<!--remember the other 18 subgroups--><ref name="atype">[https://web.archive.org/web/20080802232301/http://www.owenfoundation.com/Health_Science/Blood_Group_A_Subtypes.html Blood Group A Suptypes], The Owen Foundation. Retrieved 1 July 2008.</ref> These two subgroups are not always interchangeable as far as transfusion is concerned, as some A2 individuals produce antibodies against the A1 antigen. Complications can sometimes arise in rare cases when typing the blood.<ref name="atype" /> | |||
With the development of [[DNA sequencing]], it has been possible to identify a much larger number of alleles at the ABO locus, each of which can be categorized as A, B, or O in terms of the reaction to transfusion, but which can be distinguished by variations in the [[DNA]] sequence. There are six common [[allele]]s in white individuals of the [[ABO gene]] that produce one's blood type:<ref>{{cite journal|vauthors=Seltsam A, Hallensleben M, Kollmann A, Blasczyk R |title=The nature of diversity and diversification at the ABO locus |journal=Blood |volume=102 |issue=8 |pages=3035–42 |year=2003 |pmid=12829588 |doi=10.1182/blood-2003-03-0955}}</ref><ref>{{cite journal|author=Ogasawara K |title=Extensive polymorphism of ABO blood group gene: three major lineages of the alleles for the common ABO phenotypes |journal=Human Genetics |volume=97 |issue=6 |pages=777–83 |year=1996 |pmid=8641696 |doi=10.1007/BF02346189|author2=Bannai M|author3=Saitou N|display-authors=3|last4=Yabe|first4=Ryuichi|last5=Nakata|first5=Kenichi|last6=Takenaka|first6=Michiko|last7=Fujisawa|first7=Kiyoshi|last8=Uchikawa|first8=Makoto|last9=Ishikawa|first9=Yoshihide}}</ref> | |||
{| class="wikitable" | |||
|- | |- | ||
! A !! B !! O | |||
|- | |- | ||
| | | valign="top"|''A101'' (A1)<br />''A201'' (A2) | ||
| valign="top"|''B101'' (B1) | |||
| valign="top"|''O01'' (O1)<br />''O02'' (O1v)<br />''O03'' (O2) | |||
|} | |} | ||
The same study also identified 18 rare alleles, which generally have a weaker glycosylation activity. People with weak alleles of A can sometimes express anti-A antibodies, though these are usually not clinically significant as they do not stably interact with the antigen at body temperature.<ref>{{cite journal|title=Imbalance in A2 and A2B phenotype frequency of ABO group in South India|journal=Blood Transfusion|date=October 2010|volume=8 |issue=4|pages=267–270|doi=10.2450/2010.0147-09|pmc=2957492|pmid = 20967168|author1=Shastry|first1=S|last2=Bhat|first2=S}}</ref> | |||
[[Cis AB]] is another rare variant, in which A and B genes are transmitted together from a single parent. | |||
=== Distribution and evolutionary history === | |||
{{Main|Blood type distribution by country}} | |||
The distribution of the blood groups A, B, O and AB varies across the world according to the population. There are also variations in blood type distribution within human subpopulations. | |||
In the UK, the distribution of blood type frequencies through the population still shows some correlation to the distribution of [[Toponymy|placenames]] and to the successive invasions and migrations including [[Norsemen]], [[Danes (Germanic tribe)|Danes]], [[Saxons]], [[Celts]], and [[Normans]] who contributed the [[morpheme]]s to the placenames and the [[gene]]s to the population.<ref name=Potts_1979>{{cite book|last= Potts |first= WTW |editor= Sawyer PH |title= English Medieval Settlement|year= 1979 |publisher= St. Martin's Press |isbn= 978-0-7131-6257-8 |chapter= History and Blood Groups in the British Isles}}</ref> | |||
The two common O alleles, O01 and O02, share their first 261 [[nucleotide]]s with the group A allele A01.<ref name=Cserti2007>{{cite journal | last1 = Cserti | first1 = CM | last2 = Dzik | first2 = WH | year = 2007 | title = The ABO blood group system and ''Plasmodium falciparum malaria'' | url = | journal = Blood | volume = 110 | issue = 7| pages = 2250–2258 | doi=10.1182/blood-2007-03-077602| pmid = 17502454 }}</ref> However, unlike the group A allele, a [[guanosine]] base is subsequently deleted. A premature [[stop codon]] results from this [[frame-shift mutation]]. This variant is found worldwide, and likely predates human migration from [[Africa]]. The O01 allele is considered to predate the O02 allele.{{citation needed|date=November 2013}} | |||
Some evolutionary biologists theorize that there are four main lineages of the ABO gene and that mutations creating type O have occurred at least three times in humans.<ref name="calafell">{{cite journal|last=Calafell |first=Francesc |title=Evolutionary dynamics of the human ''ABO'' gene |url=http://www.springerlink.com/content/yv4072vu67mv1166/fulltext.html |journal=Human Genetics |date=September 2008 |volume=124 |issue=2 |pages=123–135 |doi=10.1007/s00439-008-0530-8 |pmid=18629539 |accessdate=24 September 2008 |display-authors=etal}}</ref> From oldest to youngest, these lineages comprise the following alleles: ''A101/A201/O09'', ''B101'', ''O02'' and ''O01''. The continued presence of the O alleles is hypothesized to be the result of [[balancing selection]].<ref name="calafell" /> Both theories contradict the previously held theory that type O blood evolved first.{{citation needed|date=November 2013}} | |||
=== Origin theories === | |||
It is possible that food and environmental antigens (bacterial, viral, or plant antigens) have [[epitope]]s similar enough to A and B glycoprotein antigens. The antibodies created against these environmental antigens in the first years of life can cross-react with ABO-incompatible red blood cells that it comes in contact with during blood transfusion later in life. Anti-A antibodies are hypothesized to originate from immune response towards [[influenza virus]], whose epitopes are similar enough to the α-D-N-galactosamine on the A glycoprotein to be able to elicit a cross-reaction. Anti-B antibodies are hypothesized to originate from antibodies produced against [[Gram-negative bacteria]], such as ''[[Escherichia coli|E. coli]]'', cross-reacting with the α-D-galactose on the B glycoprotein.<ref>{{Cite journal|url=http://resources.metapress.com/pdf-preview.axd?code=l2206u8gj73x3251&size=largest|doi=10.1023/B:JOPC.0000039625.56296.6e|pmid=15517982|title=Letter to the Editor: "Natural" Versus Regular Antibodies|journal=The Protein Journal|volume=23|issue=6|pages=357; author reply 359–60|year=2004|last1=Jan Van Oss|first1=Carel|access-date=28 November 2009|archive-url=https://web.archive.org/web/20110714080342/http://resources.metapress.com/pdf-preview.axd?code=l2206u8gj73x3251&size=largest|archive-date=14 July 2011|dead-url=yes|df=dmy-all}}</ref> | |||
== | However, it is more likely that the force driving evolution of allele diversity is simply negative frequency-dependent selection; cells with rare variants of membrane antigens are more easily distinguished by the immune system from pathogens carrying antigens from other hosts. Thus, individuals possessing rare types are better equipped to detect pathogens. The high within-population diversity observed in human populations would, then, be a consequence of natural selection on individuals.<ref>{{Cite journal|pmc=1691687|pages=1065–1072|year=2004|author1=Seymour|first1=R. M.|title=Evolution of the human ABO polymorphism by two complementary selective pressures|journal=Proceedings of the Royal Society B: Biological Sciences|volume=271|issue=1543|last2=Allan|first2=M. J.|last3=Pomiankowski|first3=A|last4=Gustafsson|first4=K|doi=10.1098/rspb.2004.2674|pmid=15293861}}</ref> | ||
HIV can be neutralized in ''in vitro'' experiments using antibodies against blood group antigens specifically expressed on the HIV-producing cell lines.<ref>{{cite journal| last = Arendrup | first = M |author2=Hansen JE|author3=Clausen H|author4=Nielsen C|author5=Mathiesen LR|author6= Nielsen JO | title = Antibody to histo-blood group A antigen neutralizes HIV produced by lymphocytes from blood group A donors but not from blood group B or O donors | journal = AIDS | volume = 5 | issue = 4 | pages = 441–4 |date=April 1991 | doi =10.1097/00002030-199104000-00014 | pmid = 1711864}}</ref><ref>{{cite journal| last = Neil | first = SJ |author2=McKnight A|author3=Gustafsson K|author4=Weiss RA | title = HIV-1 incorporates ABO histo-blood group antigens that sensitize virions to complement-mediated inactivation | journal = Blood | volume = 105 | issue = 12 | pages = 4693–9 | date = 2005-06-15 | url = http://bloodjournal.hematologylibrary.org/cgi/content/full/105/12/4693 | doi =10.1182/blood-2004-11-4267 | pmid = 15728127}}</ref> | |||
== | == Clinical relevance == | ||
{{ | The carbohydrate molecules on the surfaces of red blood cells have roles in [[cell membrane]] integrity, [[cell adhesion]], membrane transportation of molecules, and acting as receptors for extracellular ligands, and enzymes. ABO antigens are found having similar roles on [[epithelial cell]]s as well as red blood cells.<ref>{{cite journal | doi = 10.1053/j.seminhematol.2004.01.001 | last1 = Reid | first1 = ME | last2 = Mohandas | first2 = N | title = Red blood cell blood group antigens: structure and function. | journal = Seminars in Hematology | volume = 41 | issue = 2 | pages = 93–117 | year = 2004 | pmid = 15071789 }}</ref><ref>{{cite journal | doi = 10.1097/01.moh.0000153000.09585.79 | last1 = Mohandas | first1 = N | last2 = Narla | first2 = A | title = Blood group antigens in health and disease. | journal = Current Opinion in Hematology | volume = 12 | issue = 2 | pages = 135–40 | year = 2005 | pmid = 15725904 }}</ref> | ||
=== Bleeding and thrombosis (von Willebrand factor) === | |||
The ABO antigen is also expressed on the [[von Willebrand factor]] (vWF) [[glycoprotein]],<ref>{{cite journal| last = Sarode | first = R |author2=Goldstein J|author3=Sussman II|author4=Nagel RL|author5= Tsai HM | title = Role of A and B blood group antigens in the expression of adhesive activity of von Willebrand factor | journal = Br J Haematol | volume = 109 | issue = 4 | pages = 857–64 |date=June 2000 | doi = 10.1046/j.1365-2141.2000.02113.x| pmid = 10929042}}</ref> which participates in [[hemostasis]] (control of bleeding). In fact, having type O blood predisposes to bleeding,<ref>{{cite journal| last = O'Donnell | first = J |author2= Laffan MA | title = The relationship between ABO histo-blood group, factor VIII and von Willebrand factor | journal = Transfus Med. | volume = 11 | issue = 4 | pages = 343–51 |date=August 2001 | doi = 10.1046/j.1365-3148.2001.00315.x | pmid = 11532189}}</ref> as 30% of the total genetic variation observed in plasma vWF is explained by the effect of the ABO blood group,<ref>{{cite journal| last = O'Donnell | first = J |author2=Boulton FE|author3=Manning RA|author4=Laffan MA | title = Amount of H antigen expressed on circulating von Willebrand factor is modifiedby ABO blood group genotype and is a major determinant of plasma von Willebrand factor antigen levels | journal = [[Arteriosclerosis, Thrombosis, and Vascular Biology|Arterioscler Thromb Vasc Biol]] | volume = 22 | issue = 2 | pages = 335–41 | date = 2002-02-01 | url = http://atvb.ahajournals.org/cgi/content/full/22/2/335 | doi = 10.1161/hq0202.103997| pmid = 11834538}}</ref> and individuals with group O blood normally have significantly lower plasma levels of vWF (and [[Factor VIII]]) than do non-O individuals.<ref>{{cite journal| last = Gill | first = JC |author2=Endres-Brooks J|author3=Bauer PJ|author4=Marks WJ|author5= Montgomery RR | title = The effect of ABO blood group on the diagnosis of von Willebrand disease | journal = Blood | volume = 69 | issue = 6 | pages = 1691–5 |date=June 1987 | url = http://www.bloodjournal.org/cgi/content/abstract/69/6/1691 | pmid = 3495304 | format = abstract}}</ref><ref>{{cite journal| last = Shima | first = M |author2= Fujimura Y | title = ABO blood group genotype and plasma von Willebrand factor in normal individuals | journal = Vox Sang | volume = 68 | issue = 4 | pages = 236–40 | year = 1995 | doi = 10.1111/j.1423-0410.1995.tb02579.x| pmid = 7660643| display-authors = 2| last3 = Nishiyama | first3 = Takayuki | last4 = Tsujiuchi | first4 = Tomomi | last5 = Narita | first5 = Nobuhiro | last6 = Matsui | first6 = Taei | last7 = Titani | first7 = Koiti | last8 = Katayama | first8 = Masahiko | last9 = Yamamoto | first9 = Fumi-Ichiro | last10 = Yoshioka | first10 = Akira }}</ref> In addition, vWF is degraded more rapidly due to the higher prevalence of blood group O with the Cys1584 variant of vWF (an amino acid [[Polymorphism (biology)|polymorphism]] in VWF):<ref>{{cite journal| last = Bowen | first = DJ |author2= Collins PW | title = The prevalence of the cysteine1584 variant of von Willebrand factor is increased in type 1 von Willebrand disease: co-segregation with increased susceptibility to ADAMTS13 proteolysis but not clinical phenotype | journal = Br J Haematol | volume = 128 | issue = 6 | pages = 830–6 |date=March 2005 | doi = 10.1111/j.1365-2141.2005.05375.x | pmid = 15755288| display-authors = 2| last3 = Lester | first3 = Will | last4 = Cumming | first4 = Anthony M. | last5 = Keeney | first5 = Steven | last6 = Grundy | first6 = Pamela | last7 = Enayat | first7 = Saad M. | last8 = Bolton-Maggs | first8 = Paula H. B. | last9 = Keeling | first9 = David M. | last10 = Khair | first10 = Kate | last11 = Campbell Tait | first11 = R. | last12 = Wilde | first12 = Jonathon T. | last13 = John Pasi | first13 = K. | last14 = Hill | first14 = Frank G. H. }}</ref> the gene for [[ADAMTS13]] (vWF-cleaving [[protease]]) maps to the [[Chromosome 9 (human)|ninth chromosome]] (9q34), the same [[Locus (genetics)|locus]] as ABO blood type. Higher levels of vWF are more common amongst people who have had [[ischemic stroke]] (from blood clotting) for the first time.<ref>{{cite journal| author = Bongers T | title = High von Willebrand factor levels increase the risk of first ischemic stroke: influence of ADAMTS13, inflammation, and genetic variability | journal = Stroke | volume = 37 | issue = 11 | pages = 2672–7 | year = 2006 | pmid = 16990571 | doi = 10.1161/01.STR.0000244767.39962.f7| author2 = de Maat M| author3 = van Goor M| display-authors = 3| last4 = Bhagwanbali| first4 = V.| last5 = Van Vliet| first5 = H. H.D.M.| last6 = Gomez Garcia| first6 = E. B.| last7 = Dippel| first7 = D. W.J.| last8 = Leebeek| first8 = F. W.G.}}</ref> The results of this study found that the occurrence was not affected by ADAMTS13 polymorphism, and the only significant genetic factor was the person's blood group. | |||
== | === Disease risks === | ||
Compared to O group individuals, non-O group (A, AB, and B) individuals have a 14% reduced risk of [[squamous cell carcinoma]] and 4% reduced risk of [[basal cell carcinoma]].<ref>{{cite journal | vauthors = Xie J, Qureshi AA, Li Y, Han J | year = 2010 | title = ABO Blood Group and Incidence of Skin Cancer | journal = PLoS ONE | volume = 5 | issue = 8| page = e11972 | doi = 10.1371/journal.pone.0011972 | pmid = 20694147 | pmc = 2915921 | bibcode = 2010PLoSO...511972X }}</ref> Conversely, type O blood is associated with a reduced risk of [[pancreatic cancer]].<ref>{{cite journal | last1 = Wolpin | first1 = B. M. | last2 = Kraft | first2 = P. | last3 = Gross | first3 = M. | last4 = Helzlsouer | first4 = K. | last5 = Bueno-De-Mesquita | first5 = H. B. | last6 = Steplowski | first6 = E. | last7 = Stolzenberg-Solomon | first7 = R. Z. | last8 = Arslan | first8 = A. A. | last9 = Jacobs | first9 = E. J. | last10 = Lacroix | first10 = A. | last11 = Petersen | first11 = G. | last12 = Zheng | first12 = W. | last13 = Albanes | first13 = D. | last14 = Allen | first14 = N. E. | last15 = Amundadottir | first15 = L. | last16 = Anderson | first16 = G. | last17 = Boutron-Ruault | first17 = M. -C. | last18 = Buring | first18 = J. E. | last19 = Canzian | first19 = F. | last20 = Chanock | first20 = S. J. | last21 = Clipp | first21 = S. | last22 = Gaziano | first22 = J. M. | last23 = Giovannucci | first23 = E. L. | last24 = Hallmans | first24 = G. | last25 = Hankinson | first25 = S. E. | last26 = Hoover | first26 = R. N. | last27 = Hunter | first28 = A. | first29 = K. | last30 = Kooperberg | first30 = C. | last28 = Hutchinson | last29 = Jacobs | first27 = D. J. | title = Pancreatic Cancer Risk and ABO Blood Group Alleles: Results from the Pancreatic Cancer Cohort Consortium | doi = 10.1158/0008-5472.CAN-09-2993 | journal = Cancer Research | volume = 70 | issue = 3 | pages = 1015–1023 | year = 2010 | pmid = 20103627| pmc =2943735 | |||
}}</ref><ref>{{cite journal | last1 = Amundadottir | first1 = L. | last2 = Kraft | first2 = P. | last3 = Stolzenberg-Solomon | first3 = R. Z. | last4 = Fuchs | first4 = C. S. | last5 = Petersen | first5 = G. M. | last6 = Arslan | first6 = A. A. | last7 = Bueno-De-Mesquita | first7 = H. B. | last8 = Gross | first8 = M. | last9 = Helzlsouer | first9 = K. | last10 = Jacobs | first10 = E. J. | last11 = Lacroix | first11 = A. | last12 = Zheng | first12 = W. | last13 = Albanes | first13 = D. | last14 = Bamlet | first14 = W. | last15 = Berg | first15 = C. D. | last16 = Berrino | first16 = F. | last17 = Bingham | first17 = S. | last18 = Buring | first18 = J. E. | last19 = Bracci | first19 = P. M. | last20 = Canzian | first20 = F. | last21 = Clavel-Chapelon | first21 = F. O. | last22 = Clipp | first22 = S. | last23 = Cotterchio | first23 = M. | last24 = De Andrade | first24 = M. | last25 = Duell | first25 = E. J. | last26 = Fox Jr | first26 = J. W. | last27 = Gallinger | first28 = J. M. | first29 = E. L. | last30 = Goggins | first30 = M. | last28 = Gaziano | last29 = Giovannucci | first27 = S. | title = Genome-wide association study identifies variants in the ABO locus associated with susceptibility to pancreatic cancer | doi = 10.1038/ng.429 | journal = Nature Genetics | volume = 41 | issue = 9 | pages = 986–990 | year = 2009 | pmid = 19648918| pmc =2839871 | |||
}}</ref> The B antigen links with increased risk of [[ovarian cancer]].<ref>{{cite journal | last1 = Gates | first1 = MA | last2 = Wolpin | first2 = BM | last3 = Cramer | first3 = DW | last4 = Hankinson | first4 = SE | last5 = Tworoger | first5 = SS | title = ABO blood group and incidence of epithelial ovarian cancer | journal = International Journal of Cancer | volume = 128 | pages = 482–486 | year = 2010 | pmid = 20309936 | pmc = 2946962 | doi = 10.1002/ijc.25339 | issue = 2 }}</ref> [[Gastric cancer]] has reported to be more common in blood group A and least in group O.<ref>{{cite journal | doi = 10.1136/bmj.1.4814.799 | last1 = Aird | first1 = I | last2 = Bentall | first2 = HH | last3 = Roberts | first3 = JA | title = A relationship between cancer of stomach and the ABO blood groups | journal = British Medical Journal | volume = 1 | issue = 4814 | pages = 799–801 | year = 1953 | pmid = 13032504 | pmc = 2015995 }}</ref> | |||
According to Glass, Holmgren, et al., those in the O blood group have an increased risk of infection with [[cholera]], and those O-group individuals who are infected have more severe infections. The mechanisms behind this association with cholera are unclear in the literature.<ref name=glass_et_al>{{cite journal|last1=Glass|first1=Roger|author2=Holmgren J|author3=Haley C|author4=Khan M.R.|author5=SVENERHOLM M|author6=STOLL B|author7=HOSSAIN K|author8=BLACK B|author9=Yunus M|author10=Barua D|title=Predisposition for cholera of individuals with O blood group. Possible evolutionary significance |journal=American Journal of Epidemiology|date=June 1985|volume=121|issue=6|pages=791–796|url=http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=4014172&retmode=ref&cmd=prlinks|accessdate=20 August 2012|pmid=4014172}}</ref> | |||
== | === ABO hemolytic disease of the newborn === | ||
{{Main|Hemolytic disease of the newborn (ABO)}} | |||
ABO blood group incompatibilities between the mother and child does not usually cause [[hemolytic disease of the newborn]] (HDN) because antibodies to the ABO blood groups are usually of the [[IgM]] type, which do not cross the placenta. However, in an O-type mother, '''IgG''' ABO antibodies are produced and the baby can potentially develop [[ABO hemolytic disease of the newborn]]. | |||
In the | === Clinical applications === | ||
In human cells, the ABO alleles and their encoded glycosyltransferases have been described in several oncologic conditions.<ref>{{Cite journal|last=Goldman|first=M|date=2016-10-10|title=Translational Mini-Review Series on Toll-like Receptors: Toll-like receptor ligands as novel pharmaceuticals for allergic disorders|journal=Clinical and Experimental Immunology|volume=147|issue=2|pages=208–216|doi=10.1111/j.1365-2249.2006.03296.x|issn=0009-9104| pmc=1810467|pmid=17223960}}</ref> Using anti-GTA/GTB monoclonal antibodies, it was demonstrated that a loss of these enzymes was correlated to malignant bladder and oral epithelia.<ref>{{Cite journal|last=Kay|first=H E|date=1982-11-06|title=Bone marrow transplantation: 1982.|journal=British Medical Journal (Clinical Research Ed.)|volume=285|issue=6351|pages=1296–1298|issn=0267-0623| pmc=1500229|doi=10.1136/bmj.285.6351.1296|pmid=6812684}}</ref><ref>{{Cite journal|authorlink=Sen-itiroh Hakomori|last=Hakomori|first=S.|date=1999-12-06|title=Antigen structure and genetic basis of histo-blood groups A, B and O: their changes associated with human cancer|journal=Biochimica et Biophysica Acta|volume=1473|issue=1|pages=247–266|issn=0006-3002|pmid=10580143|doi=10.1016/s0304-4165(99)00183-x}}</ref> Furthermore, the expression of ABO blood group antigens in normal human tissues is dependent the type of differentiation of the epithelium. In most human carcinomas, including oral carcinoma, a significant event as part of the underlying mechanism is decreased expression of the A and B antigens.<ref name="Dabelsteen 21–28">{{Cite journal|last=Dabelsteen|first=E.|last2=Gao|first2=S.|date=2005-01-01|title=ABO blood-group antigens in oral cancer|journal=Journal of Dental Research|volume=84|issue=1|pages=21–28|issn=0022-0345|pmid=15615870|doi=10.1177/154405910508400103}}</ref> Several studies have observed that a relative down-regulation of GTA and GTB occurs in oral carcinomas in association with tumor development.<ref name="Dabelsteen 21–28"/><ref>{{Cite journal|last=Dabelsteen|first=Erik|date=2002-02-01|title=ABO blood group antigens in oral mucosa. What is new?|journal=Journal of Oral Pathology & Medicine|volume=31|issue=2|pages=65–70|issn=0904-2512|pmid=11896825|doi=10.1046/j.0904-2512.2001.00004.x}}</ref> More recently, a genome wide association study (GWAS) has identified variants in the ABO locus associated with susceptibility to pancreatic cancer.<ref>{{Cite journal|last=Amundadottir|first=Laufey T.|date=2016-01-01|title=Pancreatic Cancer Genetics|journal=International Journal of Biological Sciences|volume=12|issue=3|pages=314–325|doi=10.7150/ijbs.15001|issn=1449-2288|pmid=26929738|pmc=4753160}}</ref> | |||
== | === Clinical marker === | ||
A multi-locus genetic risk score study based on a combination of 27 loci, including the ABO gene, identified individuals at increased risk for both incident and recurrent coronary artery disease events, as well as an enhanced clinical benefit from statin therapy. The study was based on a community cohort study (the Malmo Diet and Cancer study) and four additional randomized controlled trials of primary prevention cohorts (JUPITER and ASCOT) and secondary prevention cohorts (CARE and PROVE IT-TIMI 22).<ref>{{Cite journal|last=Mega|first=Jessica L.|last2=Stitziel|first2=Nathan O.|last3=Smith|first3=J. Gustav|last4=Chasman|first4=Daniel I.|last5=Caulfield|first5=Mark J.|last6=Devlin|first6=James J.|last7=Nordio|first7=Francesco|last8=Hyde|first8=Craig L.|last9=Cannon|first9=Christopher P.|date=2015-06-06|title=Genetic risk, coronary heart disease events, and the clinical benefit of statin therapy: an analysis of primary and secondary prevention trials|journal=Lancet|volume=385|issue=9984|pages=2264–2271|doi=10.1016/S0140-6736(14)61730-X|issn=1474-547X|pmid=25748612|pmc=4608367}}</ref> | |||
In April 2007 an international team of researchers announced in the journal ''[[Nature Biotechnology]]'' an inexpensive and efficient way to convert types A, B and AB blood into type O. <ref>{{cite journal | == Alteration of ABO antigens for transfusion == | ||
In April 2007, an international team of researchers announced in the journal ''[[Nature Biotechnology]]'' an inexpensive and efficient way to convert types A, B, and AB blood into type O.<ref>{{cite journal|last1=Liu|first1= QP|author2=Sulzenbacher G|author3=Yuan H|author4=Bennett EP|author5=Pietz G|author6=Saunders K|author7= Spence J|author8=Nudelman E|author9=Levery SB|author10=White T|author11= Neveu JM|author12=Lane WS|author13= Bourne Y|author14=Olsson ML|author15=Henrissat B|author16=Clausen H|date=April 2007|title=Bacterial glycosidases for the production of universal red blood cells|journal=Nat Biotechnol|volume=25|issue=4|pages=454–64|pmid = 17401360|doi=10.1038/nbt1298|url = http://www.nature.com/nbt/journal/v25/n4/abs/nbt1298.html}}</ref> This is done by using [[Glycoside hydrolase|glycosidase]] enzymes from specific bacteria to strip the blood group antigens from [[red blood cell]]s. The removal of A and B antigens still does not address the problem of the [[Rh blood group system|Rh]] blood group antigen on the blood cells of Rh positive individuals, and so blood from Rh negative donors must be used. Patient trials will be conducted before the method can be relied on in live situations. | |||
</ref> This | |||
Another approach to the blood antigen problem is the | Another approach to the blood antigen problem is the manufacture of [[artificial blood]], which could act as a substitute in emergencies.<ref>[http://news.bbc.co.uk/2/hi/uk_news/england/north_yorkshire/6645923.stm BBC]</ref> | ||
== | == Pseudoscience == | ||
During the 1930s, connecting [[blood types in Japanese culture|blood groups to personality types]] became popular in Japan and other areas of the world.<ref>{{cite journal| last = American Red Cross | first = Southern California Blood Services Region | year = n.d. | title = Answers to Commonly Asked Questions About Blood and Blood Banking | journal = Blood: The Basics | page = 4 | url = http://www.socalredcross.org/pdf/BloodThe.pdf |format=PDF | accessdate =16 November 2007 |archiveurl= https://web.archive.org/web/20071129152741/http://www.socalredcross.org/pdf/BloodThe.pdf| archivedate= 29 November 2007 <!--DASHBot-->| deadurl= no}}</ref> Studies of this association have yet to confirm its existence definitively.<ref>Sung Il Ryu, Young Woo Sohn (2007), ''A Review of Sociocultural, Behavioral, Biochemical Analyses on ABO Blood-Groups Typology'', The Korean Journal of Social and Personality Psychology.</ref><ref>{{cite journal | last1 = Hobgood | first1 = Donna K. | year = 2011 | title = Personality traits of aggression-submissiveness and perfectionism associate with ABO blood groups through catecholamine activities | url = http://www.sciencedirect.com/science/article/pii/S0306987711002106 | journal = Medical Hypotheses | volume = 77 | issue = 2| pages = 294–300 | doi=10.1016/j.mehy.2011.04.039 | pmid=21601990}}</ref> | |||
Other popular but unsupported ideas include the use of a [[blood type diet]], claims that group A causes severe [[hangover]]s, group O is associated with perfect teeth, and those with blood group A2 have the highest [[IQ]]s. Scientific evidence in support of these concepts is nonexistent.<ref>{{cite journal| last = Klein | first = Harvey G | date = 7 March 2005 | title = Why Do People Have Different Blood Types? | journal = Scientific American | url = http://www.sciam.com/article.cfm?id=why-do-people-have-differ | accessdate =16 November 2007}}</ref> | |||
</ref> | |||
==Data tables== | |||
{{Kang1997Table2}} | |||
== See also == | |||
* [[Kidd blood group]] | |||
== References == | == References == | ||
{{ | {{reflist|colwidth=30em}} | ||
== Further reading == | == Further reading == | ||
* {{cite web| author = Dean L | title = Chapter 5: The ABO blood group. | work = Blood Groups and Red Cell Antigens | url = https://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=rbcantigen.chapter.ch05ABO |year = 2005 | accessdate =24 March 2007}} | |||
* {{cite web | author = Dean L | title = Chapter 5: The ABO blood group. | work = Blood Groups and Red Cell Antigens | url = | * {{cite journal|author=Farr A |title=Blood group serology--the first four decades (1900--1939) |journal=Med Hist |volume=23 |issue=2 |pages=215–26 |date=1 April 1979| pmid=381816 |pmc=1082436 |doi=10.1017/s0025727300051383}} | ||
* {{cite journal |author=Farr A |title=Blood group serology--the first four decades (1900--1939) |journal=Med Hist |volume=23 |issue=2 |pages= | |||
== External links == | == External links == | ||
* [https://www.ncbi.nlm.nih.gov/gv/mhc/xslcgi.cgi?cmd=bgmut/systems_info&system=abo ABO] at [[BGMUT]] Blood Group Antigen Gene Mutation Database at [[National Center for Biotechnology Information|NCBI]], [[NIH]] | |||
* [ | * [https://www.youtube.com/watch?v=u7DxZmLWDII ABO blood groups, antibodies and antigens explained] YouTube educational video | ||
* [ | * [http://www.britannica.com/eb/article-9003372/ABO-blood-group-system Encyclopædia Britannica, ABO blood group system] | ||
* [http://www.britannica.com/eb/article-9003372/ABO-blood-group-system | * [https://web.archive.org/web/20070607182528/http://www.blood.co.uk/pages/world_blood.html National Blood Transfusion Service] | ||
* [http://www.blood.co.uk/pages/world_blood.html National Blood Transfusion Service] | * [http://abobloodgroup.googlepages.com/ Molecular Genetic Basis of ABO] | ||
* [http://abobloodgroup.googlepages.com/ Molecular Genetic Basis of | |||
{{transfusion medicine}} | {{transfusion medicine}} | ||
[[Category:Blood antigen systems]] | [[Category:Blood antigen systems]] | ||
[[Category: | [[Category:Transfusion medicine]] | ||
[[Category:Antigenic determinant]] | |||
[[Category:Hematopathology]] | |||
[[Category:Glycoproteins]] | |||
[[ | [[Category:Serology]] | ||
[[ | [[Category:Genes on human chromosome 9]] | ||
[[ | |||
[[ | |||
[[ | |||
Latest revision as of 07:45, 10 January 2019

The ABO blood group system is used to denote the presence of one, both, or neither of the A and B antigens on erythrocytes.[1] In human blood transfusions it is the most important of the 36 different blood type (or group) classification systems currently recognized.[2] A very rare (in modern medicine) mismatch in this, or any other serotype, can cause a serious, potentially fatal, adverse reaction after a transfusion, or a contra-indicated immune response to an organ transplant.[3] The associated anti-A and anti-B antibodies are usually IgM antibodies, which are produced in the first years of life by sensitization to environmental substances, such as food, bacteria, and viruses.
The ABO blood types were discovered by Karl Landsteiner in 1901, for which he received the Nobel Prize in Physiology or Medicine in 1930. ABO blood types are also present in some other animals such as rodents and apes, including chimpanzees, bonobos, and gorillas.[4]
History
The ABO blood types were first discovered by an Austrian Physician Karl Landsteiner working at the Pathological-Anatomical Institute of the University of Vienna (now Medical University of Vienna). In 1900, he found that blood sera from different persons would clump together (agglutinate) when mixed in test tubes, and not only that some human blood also agglutinated with animal blood.[5] He wrote a two-sentence footnote:
The serum of healthy human beings not only agglutinates animal red cells, but also often those of human origin, from other individuals. It remains to be seen whether this appearance is related to inborn differences between individuals or it is the result of some damage of bacterial kind.[6]
This was the first evidence that blood variation exists in humans – it was believed that all humans have similar blood. The next year, in 1901, he made a definitive observation that blood serum of an individual would agglutinate with only those of certain individuals. Based on this he classified human bloods into three groups, namely group A, group B, and group C. He defined that group A blood agglutinates with group B, but never with its own type. Similarly, group B blood agglutinates with group A. Group C blood is different in that it agglutinates with both A and B.[7] This was the discovery of blood groups for which Landsteiner was awarded the Nobel Prize in Physiology or Medicine in 1930. In his paper, he called the specific blood group interactions as isoagglutination, and also introduced the concept of agglutinins (antibodies), which is the actual basis of antigen-antibody reaction in ABO system.[8] He asserted:
[It] may be said that there exist at least two different types of agglutinins, one in A, another one in B, and both together
in C. The red blood cells are inert to the agglutinins which are present in the same serum.[7]
Thus, he discovered two antigens (agglutinogens A and B) and two antibodies (agglutinins - anti-A and anti-B). His third group (C) indicated absence of both A and B antigens, but contains anti-A and anti-B.[8] The following year, his students Adriano Sturli and Alfred von Decastello discovered the fourth type (but not naming it, and simply referred to it as "no particular type”).[9][10]
In 1910, Ludwik Hirszfeld and Emil Freiherr von Dungern introduced the term 0 (null) for the group Landsteiner designated as C, and AB for the type discovered by Sturli and von Decastello. They were also the first to explain the genetic inheritance of the blood groups.[11])
Czech serologist Jan Janský independently introduced blood type classification in 1907 in a local journal.[12] He used the Roman numerical I, II, III, and IV (corresponding to modern O, A, B, and AB). Unbeknown to Janský, an American physician William L. Moss devised a slightly different classification using the same numerical;[13] his I, II, III, and IV corresponding to modern AB, A, B, and O.[10] These two systems created confusion and potential danger in medical practice. Moss's system was adopted in Britain, France, and US, while Janský's was preferred in most European countries and some parts of US. To resolve the chaos, the American Association of Immunologists, the Society of American Bacteriologists, and the Association of Pathologists and Bacteriologists made a joint recommendation in 1921 that the Jansky classification be adopted based on priority.[14] But it was not followed particularly where Moss's system had been used. In 1927, Landsteiner, who had moved to the Rockefeller Institute for Medical Research in New York, and as a member of a committee of the National Research Council concerned with blood grouping suggested to substitute Janský's and Moss's systems with the letters 0, A, B, and AB. (There was another confusion on the use of figure 0 for German null as introduced by Hirszfeld and von Dungern, because others used the letter O for ohne, meaning without or zero; Landsteiner chose the latter.[15]) This classification was adopted by the National Research Council and became variously known as the National Research Council classification, the International classification, and most popularly the "new" Landsteiner classification. The new system was gradually accepted and by the early 1950s, it was universally followed.[16]
The first practical use of blood typing in transfusion was by an American physician Reuben Ottenberg in 1907. And the large-scale application started during the First World War (1914-1915) when citric acid was developed as blood clot prevention.[8] Felix Bernstein demonstrated the correct blood group inheritance pattern of multiple alleles at one locus in 1924.[17] Watkins and Morgan, in England, discovered that the ABO epitopes were conferred by sugars, to be specific, N-acetylgalactosamine for the A-type and galactose for the B-type.[18][19][20] After much published literature claiming that the ABH substances were all attached to glycosphingolipids, Finne et al. (1978) found that the human erythrocyte glycoproteins contain polylactosamine chains[21] that contains ABH substances attached and represent the majority of the antigens.[22][23][24] The main glycoproteins carrying the ABH antigens were identified to be the Band 3 and Band 4.5 proteins and glycophorin.[25] Later, Yamamoto's group showed the precise glycosyl transferase set that confers the A, B and O epitopes.[26]
Genetics
Blood groups are inherited from both parents. The ABO blood type is controlled by a single gene (the ABO gene) with three types of alleles inferred from classical genetics: i, IA, and IB. The I designation stands for isoagglutinogen, another term for antigen.[28] The gene encodes a glycosyltransferase—that is, an enzyme that modifies the carbohydrate content of the red blood cell antigens. The gene is located on the long arm of the ninth chromosome (9q34).
The IA allele gives type A, IB gives type B, and i gives type O. As both IA and IB are dominant over i, only ii people have type O blood. Individuals with IAIA or IAi have type A blood, and individuals with IBIB or IBi have type B. IAIB people have both phenotypes, because A and B express a special dominance relationship: codominance, which means that type A and B parents can have an AB child. A couple with type A and type B can also have a type O child if they are both heterozygous (IBi,IAi). The cis-AB phenotype has a single enzyme that creates both A and B antigens. The resulting red blood cells do not usually express A or B antigen at the same level that would be expected on common group A1 or B red blood cells, which can help solve the problem of an apparently genetically impossible blood group.[29]
| Blood group inheritance | |||||||
| Blood type | O | A | B | AB | |||
|---|---|---|---|---|---|---|---|
| Genotype | ii (OO) | IAi (AO) | IAIA (AA) | IBi (BO) | IBIB (BB) | IAIB (AB) | |
| O | ii (OO) | O OO OO OO OO |
O or A AO OO AO OO |
A AO AO AO AO |
O or B BO OO BO OO |
B BO BO BO BO |
A or B AO BO AO BO |
| A | IAi (AO) | O or A AO AO OO OO |
O or A AA AO AO OO |
A AA AA AO AO |
O, A, B or AB AB AO BO OO |
B or AB AB AB BO BO |
A, B or AB AA AB AO BO |
| IAIA (AA) | A AO AO AO AO |
A AA AO AA AO |
A AA AA AA AA |
A or AB AB AO AB AO |
AB AB AB AB AB |
A or AB AA AB AA AB | |
| B | IBi (BO) | O or B BO BO OO OO |
O, A, B or AB AB BO AO OO |
A or AB AB AB AO AO |
O or B BB BO BO OO |
B BB BB BO BO |
A, B or AB AB BB AO BO |
| IBIB (BB) | B BO BO BO BO |
B or AB AB BO AB BO |
AB AB AB AB AB |
B BB BO BB BO |
B BB BB BB BB |
B or AB AB BB AB BB | |
| AB | IAIB (AB) | A or B AO AO BO BO |
A, B or AB AA AO AB BO |
A or AB AA AA AB AB |
A, B or AB AB AO BB BO |
B or AB AB AB BB BB |
A, B, or AB AA AB AB BB |
The table above summarizes the various blood groups that children may inherit from their parents.[30][31] Genotypes are shown in the second column and in small print for the offspring: AO and AA both test as type A; BO and BB test as type B. The four possibilities represent the combinations obtained when one allele is taken from each parent; each has a 25% chance, but some occur more than once.
| Blood group inheritance by phenotype only | ||||
| Blood type | O | A | B | AB |
|---|---|---|---|---|
| O | O | O or A | O or B | A or B |
| A | O or A | O or A | O, A, B or AB | A, B or AB |
| B | O or B | O, A, B or AB | O or B | A, B or AB |
| AB | A or B | A, B or AB | A, B or AB | A, B or AB |
Historically, ABO blood tests were used in paternity testing, but in 1957 only 50% of American men falsely accused were able to use them as evidence against paternity.[32] Occasionally, the blood types of children are not consistent with expectations—for example, a type O child can be born to an AB parent—due to rare situations, such as Bombay phenotype and cis AB.[33]
Subgroups
The A blood type contains about 20 subgroups, of which A1 and A2 are the most common (over 99%). A1 makes up about 80% of all A-type blood, with A2 making up almost all of the rest.[34] These two subgroups are not always interchangeable as far as transfusion is concerned, as some A2 individuals produce antibodies against the A1 antigen. Complications can sometimes arise in rare cases when typing the blood.[34]
With the development of DNA sequencing, it has been possible to identify a much larger number of alleles at the ABO locus, each of which can be categorized as A, B, or O in terms of the reaction to transfusion, but which can be distinguished by variations in the DNA sequence. There are six common alleles in white individuals of the ABO gene that produce one's blood type:[35][36]
| A | B | O |
|---|---|---|
| A101 (A1) A201 (A2) |
B101 (B1) | O01 (O1) O02 (O1v) O03 (O2) |
The same study also identified 18 rare alleles, which generally have a weaker glycosylation activity. People with weak alleles of A can sometimes express anti-A antibodies, though these are usually not clinically significant as they do not stably interact with the antigen at body temperature.[37]
Cis AB is another rare variant, in which A and B genes are transmitted together from a single parent.
Distribution and evolutionary history
The distribution of the blood groups A, B, O and AB varies across the world according to the population. There are also variations in blood type distribution within human subpopulations.
In the UK, the distribution of blood type frequencies through the population still shows some correlation to the distribution of placenames and to the successive invasions and migrations including Norsemen, Danes, Saxons, Celts, and Normans who contributed the morphemes to the placenames and the genes to the population.[38]
The two common O alleles, O01 and O02, share their first 261 nucleotides with the group A allele A01.[39] However, unlike the group A allele, a guanosine base is subsequently deleted. A premature stop codon results from this frame-shift mutation. This variant is found worldwide, and likely predates human migration from Africa. The O01 allele is considered to predate the O02 allele.[citation needed]
Some evolutionary biologists theorize that there are four main lineages of the ABO gene and that mutations creating type O have occurred at least three times in humans.[40] From oldest to youngest, these lineages comprise the following alleles: A101/A201/O09, B101, O02 and O01. The continued presence of the O alleles is hypothesized to be the result of balancing selection.[40] Both theories contradict the previously held theory that type O blood evolved first.[citation needed]
Origin theories
It is possible that food and environmental antigens (bacterial, viral, or plant antigens) have epitopes similar enough to A and B glycoprotein antigens. The antibodies created against these environmental antigens in the first years of life can cross-react with ABO-incompatible red blood cells that it comes in contact with during blood transfusion later in life. Anti-A antibodies are hypothesized to originate from immune response towards influenza virus, whose epitopes are similar enough to the α-D-N-galactosamine on the A glycoprotein to be able to elicit a cross-reaction. Anti-B antibodies are hypothesized to originate from antibodies produced against Gram-negative bacteria, such as E. coli, cross-reacting with the α-D-galactose on the B glycoprotein.[41]
However, it is more likely that the force driving evolution of allele diversity is simply negative frequency-dependent selection; cells with rare variants of membrane antigens are more easily distinguished by the immune system from pathogens carrying antigens from other hosts. Thus, individuals possessing rare types are better equipped to detect pathogens. The high within-population diversity observed in human populations would, then, be a consequence of natural selection on individuals.[42]
HIV can be neutralized in in vitro experiments using antibodies against blood group antigens specifically expressed on the HIV-producing cell lines.[43][44]
Clinical relevance
The carbohydrate molecules on the surfaces of red blood cells have roles in cell membrane integrity, cell adhesion, membrane transportation of molecules, and acting as receptors for extracellular ligands, and enzymes. ABO antigens are found having similar roles on epithelial cells as well as red blood cells.[45][46]
Bleeding and thrombosis (von Willebrand factor)
The ABO antigen is also expressed on the von Willebrand factor (vWF) glycoprotein,[47] which participates in hemostasis (control of bleeding). In fact, having type O blood predisposes to bleeding,[48] as 30% of the total genetic variation observed in plasma vWF is explained by the effect of the ABO blood group,[49] and individuals with group O blood normally have significantly lower plasma levels of vWF (and Factor VIII) than do non-O individuals.[50][51] In addition, vWF is degraded more rapidly due to the higher prevalence of blood group O with the Cys1584 variant of vWF (an amino acid polymorphism in VWF):[52] the gene for ADAMTS13 (vWF-cleaving protease) maps to the ninth chromosome (9q34), the same locus as ABO blood type. Higher levels of vWF are more common amongst people who have had ischemic stroke (from blood clotting) for the first time.[53] The results of this study found that the occurrence was not affected by ADAMTS13 polymorphism, and the only significant genetic factor was the person's blood group.
Disease risks
Compared to O group individuals, non-O group (A, AB, and B) individuals have a 14% reduced risk of squamous cell carcinoma and 4% reduced risk of basal cell carcinoma.[54] Conversely, type O blood is associated with a reduced risk of pancreatic cancer.[55][56] The B antigen links with increased risk of ovarian cancer.[57] Gastric cancer has reported to be more common in blood group A and least in group O.[58]
According to Glass, Holmgren, et al., those in the O blood group have an increased risk of infection with cholera, and those O-group individuals who are infected have more severe infections. The mechanisms behind this association with cholera are unclear in the literature.[59]
ABO hemolytic disease of the newborn
ABO blood group incompatibilities between the mother and child does not usually cause hemolytic disease of the newborn (HDN) because antibodies to the ABO blood groups are usually of the IgM type, which do not cross the placenta. However, in an O-type mother, IgG ABO antibodies are produced and the baby can potentially develop ABO hemolytic disease of the newborn.
Clinical applications
In human cells, the ABO alleles and their encoded glycosyltransferases have been described in several oncologic conditions.[60] Using anti-GTA/GTB monoclonal antibodies, it was demonstrated that a loss of these enzymes was correlated to malignant bladder and oral epithelia.[61][62] Furthermore, the expression of ABO blood group antigens in normal human tissues is dependent the type of differentiation of the epithelium. In most human carcinomas, including oral carcinoma, a significant event as part of the underlying mechanism is decreased expression of the A and B antigens.[63] Several studies have observed that a relative down-regulation of GTA and GTB occurs in oral carcinomas in association with tumor development.[63][64] More recently, a genome wide association study (GWAS) has identified variants in the ABO locus associated with susceptibility to pancreatic cancer.[65]
Clinical marker
A multi-locus genetic risk score study based on a combination of 27 loci, including the ABO gene, identified individuals at increased risk for both incident and recurrent coronary artery disease events, as well as an enhanced clinical benefit from statin therapy. The study was based on a community cohort study (the Malmo Diet and Cancer study) and four additional randomized controlled trials of primary prevention cohorts (JUPITER and ASCOT) and secondary prevention cohorts (CARE and PROVE IT-TIMI 22).[66]
Alteration of ABO antigens for transfusion
In April 2007, an international team of researchers announced in the journal Nature Biotechnology an inexpensive and efficient way to convert types A, B, and AB blood into type O.[67] This is done by using glycosidase enzymes from specific bacteria to strip the blood group antigens from red blood cells. The removal of A and B antigens still does not address the problem of the Rh blood group antigen on the blood cells of Rh positive individuals, and so blood from Rh negative donors must be used. Patient trials will be conducted before the method can be relied on in live situations.
Another approach to the blood antigen problem is the manufacture of artificial blood, which could act as a substitute in emergencies.[68]
Pseudoscience
During the 1930s, connecting blood groups to personality types became popular in Japan and other areas of the world.[69] Studies of this association have yet to confirm its existence definitively.[70][71]
Other popular but unsupported ideas include the use of a blood type diet, claims that group A causes severe hangovers, group O is associated with perfect teeth, and those with blood group A2 have the highest IQs. Scientific evidence in support of these concepts is nonexistent.[72]
Data tables
| ABO allele frequencies in Korean, Japanese and German populations | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Population | |||||||||
| A(Pro) | A(Leu) | B | O(T) | O(A) | O2 | ||||
| Korean (n = 253) | 0.022a,c | 0.209c | 0.209c | 0.360a,e | 0.200b | 0d | |||
| Japanese1 (n = 520) | 0.071 | 0.216 | 0.178 | 0.273 | 0.262 | 0 | |||
| German2 (n = 169) | 0.213 | 0.077 | 0.047 | 0.426 | 0.216 | 0.021 | |||
| aKorean versus Japanese, p < 0.001. bKorean versus Japanese, p < 0.01. cKorean versus German, p < 0.001. dKorean versus German, p < 0.01. eKorean versus German, p < 0.05 (Fisher's exact probability test). 1Fukumori et al., 1996. 2Nishimukai et al., 1996. | |||||||||
See also
References
- ↑ The Editors of Encyclopædia Britannica (2017-07-18). "ABO blood group system". Encyclopædia Britannica. Encyclopædia Britannica, Inc. Retrieved 2017-10-26.
- ↑ Storry, J. R.; Castilho, L.; Chen, Q.; Daniels, G.; Denomme, G.; Flegel, W. A.; Gassner, C.; de Haas, M.; et al. (2016). "International society of blood transfusion working party on red cell immunogenetics and terminology: report of the Seoul and London meetings". ISBT Science Series. 11 (2): 118–122. doi:10.1111/voxs.12280. PMC 5662010. PMID 29093749.
- ↑ Muramatsu M, Gonzalez HD, Cacciola R, Aikawa A, Yaqoob MM, Puliatti C (2014). "ABO incompatible renal transplants: Good or bad?". World Journal of Transplantation. 4 (1): 18–29. doi:10.5500/wjt.v4.i1.18. PMC 3964193. PMID 24669364.
- ↑ Maton, Anthea; Jean Hopkins; Charles William McLaughlin; Susan Johnson; Maryanna Quon Warner; David LaHart; Jill D. Wright (1993). Human Biology and Health. Englewood Cliffs, New Jersey, USA: Prentice Hall. ISBN 978-0-13-981176-0.
- ↑ Landsteiner K (1900). "Zur Kenntnis der antifermentativen, lytischen und agglutinierenden Wirkungen des Blutserums und der Lymphe". Zentralblatt für Bakteriologie, Parasitenkunde und Infektionskrankheiten. 27: 357–362.
- ↑ Kantha, S.S. (1995). "The blood revolution initiated by the famous footnote of Karl Landsteiner's 1900 paper" (PDF). The Ceylon Medical Journal. 40 (3): 123–125. PMID 8536328.
- ↑ 7.0 7.1 Landsteiner, Karl (1961) [1901]. "On Agglutination of Normal Human Blood". Transfusion. 1 (1): 5–8. doi:10.1111/j.1537-2995.1961.tb00005.x. PMID 13758692Originally published in German in Wiener Klinische Wochenschrift, 46, 1132–1134
- ↑ 8.0 8.1 8.2 Durand, J.K.; Willis, M.S. (2010). "Karl Landsteiner, MD: Transfusion Medicine". Laboratory Medicine. 41 (1): 53–55. doi:10.1309/LM0MICLH4GG3QNDC.
- ↑ Von Decastello, A.; Sturli, A. (1902). "Concerning isoagglutinins in serum of healthy and sick humans". Munchener Medizinische Wochenschrift. 26: 1090–1095.
- ↑ 10.0 10.1 Farr AD (April 1979). "Blood group serology—the first four decades (1900–1939)". Medical History. 23 (2): 215–26. doi:10.1017/s0025727300051383. PMC 1082436. PMID 381816.
- ↑ Farhud, D.D.; Zarif Yeganeh, M. (2013). "A brief history of human blood groups". Iranian Journal of Public Health. 42 (1): 1–6. PMC 3595629. PMID 23514954.
- ↑ Janský J. (1907). "Haematologick studie u. psychotiku". Sborn. Klinick (in Czech). 8: 85–139.
- ↑ Moss W.L. (1910). "Studies on isoagglutinins and isohemolysins". Bulletin of Johns Hopkins Hospital. 21: 63–70.
- ↑ Doan, C.A. (1927). "The Transfusion problem". Physiological Reviews. 7 (1): 1–84. doi:10.1152/physrev.1927.7.1.1.
- ↑ Schmidt, P.; Okroi, M. (2001). "Also sprach Landsteiner – Blood Group 'O' or Blood Group 'NULL'". Transfusion Medicine and Hemotherapy. 28 (4): 206–208. doi:10.1159/000050239.
- ↑ Garratty, G.; Dzik, W.; Issitt, P.D.; Lublin, D.M.; Reid, M.E.; Zelinski, T. (2000). "Terminology for blood group antigens and genes-historical origins and guidelines in the new millennium". Transfusion. 40 (4): 477–489. doi:10.1046/j.1537-2995.2000.40040477.x. PMID 10773062.
- ↑ Crow J (1993). "Felix Bernstein and the first human marker locus". Genetics. 133 (1): 4–7. PMC 1205297. PMID 8417988.
- ↑ Morgan, W. T. J.; Watkins, W. M (1969). "Genetic and biochemical aspects of human blood-group A-, B-, H-, Le-a- and Le-b-specificity". Br. Med. Bull. 25 (1): 30–34. PMID 5782756.
- ↑ Watkins, W. M. Advances in Human Genetics Vol. 10 (eds Harris, H. & Hirschhorn, K.) 1–136 (Plenum, New York, 1980)
- ↑ Watkins, W. M.; Morgan, W. T. J. (1959). "Possible Genetical Pathways for the Biosynthesis of Blood Group Mucopolysaccharides". Vox Sang. 4 (2): 97–119. doi:10.1111/j.1423-0410.1959.tb04023.x. PMID 13669421.
- ↑ Finne; Krusius; Rauvala; Kekomäki; Myllylä (1978). "Alkali-stable blood group A- and B-active poly(glycosyl)-peptides from human erythrocyte membrane". FEBS Left. 89: 111–115. doi:10.1016/0014-5793(78)80534-1.
- ↑ Krusius; Finne; Rauvala (1978). "The Poly(glycosyl) Chains of Glycoproteins.. Characterisation of a Novel Type of Glycoprotein Saccharides from Human Erythrocyte Membrane". Eur. J. Biochem. 92 (1): 289–300. doi:10.1111/j.1432-1033.1978.tb12747.x. PMID 729592.
- ↑ Järnefelt; Rush; Li; Laine (1978). "Erythroglycan, a high molecular weight glycopeptide with the repeating structure [galactosyl-(1 leads to 4)-2-deoxy-2-acetamido-glucosyl(1 leads to 3)] comprising more than one-third of the protein-bound carbohydrate of human erythrocyte stroma". J. Biol. Chem. 253 (22): 8006–8009. PMID 711733.
- ↑ Laine and Rush in Molecular Immunology of Complex Carbohydrates (A. Wu, E. Kabat, Eds.) Plenum Publishing Corporation, N.Y. NY (1988)
- ↑ Finne (1980). "Identification of the Blood-Group ABH-Active Glycoprotein Components of Human Erythrocyte Membrane". Eur. J. Biochem. 104: 181–189. doi:10.1111/j.1432-1033.1980.tb04414.x.
- ↑ Yamamoto; et al. (1990). "Molecular genetic basis of the histo-blood group ABO system". Nature. 345 (6272): 229–233. Bibcode:1990Natur.345..229Y. doi:10.1038/345229a0. PMID 2333095.
- ↑ Hara, Atsushi; Imamura, Akihiro; Ando, Hiromune; Ishida, Hideharu; Kiso, Makoto (31 December 2013). "A New Chemical Approach to Human ABO Histo-Blood Group Type 2 Antigens". Molecules. 19 (1): 414–437. doi:10.3390/molecules19010414. PMID 24384923.
- ↑ Klug, William S.; Cummings, Michael R. (1997). Concepts of Genetics (5th ed.). Upper Saddle River, NJ: Prentice Hall. p. 83. ISBN 978-0135310625.
- ↑ Yazer M, Olsson M, Palcic M (2006). "The cis-AB blood group phenotype: fundamental lessons in glycobiology". Transfus Med Rev. 20 (3): 207–17. doi:10.1016/j.tmrv.2006.03.002. PMID 16787828.
- ↑ "ABO inheritance patterns". Inheritance patterns of blood groups. Australian Red Cross Blood Service. Retrieved 30 October 2013.
- ↑ "ABO blood group system". Abobloodtypes.webnode.com. Retrieved 2015-02-02.
- ↑ Cited in "Misattributed paternity rates and non-paternity rates".
- ↑ "Understanding genetics". Stanford.
- ↑ 34.0 34.1 Blood Group A Suptypes, The Owen Foundation. Retrieved 1 July 2008.
- ↑ Seltsam A, Hallensleben M, Kollmann A, Blasczyk R (2003). "The nature of diversity and diversification at the ABO locus". Blood. 102 (8): 3035–42. doi:10.1182/blood-2003-03-0955. PMID 12829588.
- ↑ Ogasawara K; Bannai M; Saitou N; et al. (1996). "Extensive polymorphism of ABO blood group gene: three major lineages of the alleles for the common ABO phenotypes". Human Genetics. 97 (6): 777–83. doi:10.1007/BF02346189. PMID 8641696.
- ↑ Shastry, S; Bhat, S (October 2010). "Imbalance in A2 and A2B phenotype frequency of ABO group in South India". Blood Transfusion. 8 (4): 267–270. doi:10.2450/2010.0147-09. PMC 2957492. PMID 20967168.
- ↑ Potts, WTW (1979). "History and Blood Groups in the British Isles". In Sawyer PH. English Medieval Settlement. St. Martin's Press. ISBN 978-0-7131-6257-8.
- ↑ Cserti, CM; Dzik, WH (2007). "The ABO blood group system and Plasmodium falciparum malaria". Blood. 110 (7): 2250–2258. doi:10.1182/blood-2007-03-077602. PMID 17502454.
- ↑ 40.0 40.1 Calafell, Francesc; et al. (September 2008). "Evolutionary dynamics of the human ABO gene". Human Genetics. 124 (2): 123–135. doi:10.1007/s00439-008-0530-8. PMID 18629539. Retrieved 24 September 2008.
- ↑ Jan Van Oss, Carel (2004). "Letter to the Editor: "Natural" Versus Regular Antibodies". The Protein Journal. 23 (6): 357, author reply 359–60. doi:10.1023/B:JOPC.0000039625.56296.6e. PMID 15517982. Archived from the original on 14 July 2011. Retrieved 28 November 2009.
- ↑ Seymour, R. M.; Allan, M. J.; Pomiankowski, A; Gustafsson, K (2004). "Evolution of the human ABO polymorphism by two complementary selective pressures". Proceedings of the Royal Society B: Biological Sciences. 271 (1543): 1065–1072. doi:10.1098/rspb.2004.2674. PMC 1691687. PMID 15293861.
- ↑ Arendrup, M; Hansen JE; Clausen H; Nielsen C; Mathiesen LR; Nielsen JO (April 1991). "Antibody to histo-blood group A antigen neutralizes HIV produced by lymphocytes from blood group A donors but not from blood group B or O donors". AIDS. 5 (4): 441–4. doi:10.1097/00002030-199104000-00014. PMID 1711864.
- ↑ Neil, SJ; McKnight A; Gustafsson K; Weiss RA (2005-06-15). "HIV-1 incorporates ABO histo-blood group antigens that sensitize virions to complement-mediated inactivation". Blood. 105 (12): 4693–9. doi:10.1182/blood-2004-11-4267. PMID 15728127.
- ↑ Reid, ME; Mohandas, N (2004). "Red blood cell blood group antigens: structure and function". Seminars in Hematology. 41 (2): 93–117. doi:10.1053/j.seminhematol.2004.01.001. PMID 15071789.
- ↑ Mohandas, N; Narla, A (2005). "Blood group antigens in health and disease". Current Opinion in Hematology. 12 (2): 135–40. doi:10.1097/01.moh.0000153000.09585.79. PMID 15725904.
- ↑ Sarode, R; Goldstein J; Sussman II; Nagel RL; Tsai HM (June 2000). "Role of A and B blood group antigens in the expression of adhesive activity of von Willebrand factor". Br J Haematol. 109 (4): 857–64. doi:10.1046/j.1365-2141.2000.02113.x. PMID 10929042.
- ↑ O'Donnell, J; Laffan MA (August 2001). "The relationship between ABO histo-blood group, factor VIII and von Willebrand factor". Transfus Med. 11 (4): 343–51. doi:10.1046/j.1365-3148.2001.00315.x. PMID 11532189.
- ↑ O'Donnell, J; Boulton FE; Manning RA; Laffan MA (2002-02-01). "Amount of H antigen expressed on circulating von Willebrand factor is modifiedby ABO blood group genotype and is a major determinant of plasma von Willebrand factor antigen levels". Arterioscler Thromb Vasc Biol. 22 (2): 335–41. doi:10.1161/hq0202.103997. PMID 11834538.
- ↑ Gill, JC; Endres-Brooks J; Bauer PJ; Marks WJ; Montgomery RR (June 1987). "The effect of ABO blood group on the diagnosis of von Willebrand disease" (abstract). Blood. 69 (6): 1691–5. PMID 3495304.
- ↑ Shima, M; Fujimura Y; et al. (1995). "ABO blood group genotype and plasma von Willebrand factor in normal individuals". Vox Sang. 68 (4): 236–40. doi:10.1111/j.1423-0410.1995.tb02579.x. PMID 7660643.
- ↑ Bowen, DJ; Collins PW; et al. (March 2005). "The prevalence of the cysteine1584 variant of von Willebrand factor is increased in type 1 von Willebrand disease: co-segregation with increased susceptibility to ADAMTS13 proteolysis but not clinical phenotype". Br J Haematol. 128 (6): 830–6. doi:10.1111/j.1365-2141.2005.05375.x. PMID 15755288.
- ↑ Bongers T; de Maat M; van Goor M; et al. (2006). "High von Willebrand factor levels increase the risk of first ischemic stroke: influence of ADAMTS13, inflammation, and genetic variability". Stroke. 37 (11): 2672–7. doi:10.1161/01.STR.0000244767.39962.f7. PMID 16990571.
- ↑ Xie J, Qureshi AA, Li Y, Han J (2010). "ABO Blood Group and Incidence of Skin Cancer". PLoS ONE. 5 (8): e11972. Bibcode:2010PLoSO...511972X. doi:10.1371/journal.pone.0011972. PMC 2915921. PMID 20694147.
- ↑ Wolpin, B. M.; Kraft, P.; Gross, M.; Helzlsouer, K.; Bueno-De-Mesquita, H. B.; Steplowski, E.; Stolzenberg-Solomon, R. Z.; Arslan, A. A.; Jacobs, E. J.; Lacroix, A.; Petersen, G.; Zheng, W.; Albanes, D.; Allen, N. E.; Amundadottir, L.; Anderson, G.; Boutron-Ruault, M. -C.; Buring, J. E.; Canzian, F.; Chanock, S. J.; Clipp, S.; Gaziano, J. M.; Giovannucci, E. L.; Hallmans, G.; Hankinson, S. E.; Hoover, R. N.; Hunter, D. J.; Hutchinson, A.; Jacobs, K.; Kooperberg, C. (2010). "Pancreatic Cancer Risk and ABO Blood Group Alleles: Results from the Pancreatic Cancer Cohort Consortium". Cancer Research. 70 (3): 1015–1023. doi:10.1158/0008-5472.CAN-09-2993. PMC 2943735. PMID 20103627.
- ↑ Amundadottir, L.; Kraft, P.; Stolzenberg-Solomon, R. Z.; Fuchs, C. S.; Petersen, G. M.; Arslan, A. A.; Bueno-De-Mesquita, H. B.; Gross, M.; Helzlsouer, K.; Jacobs, E. J.; Lacroix, A.; Zheng, W.; Albanes, D.; Bamlet, W.; Berg, C. D.; Berrino, F.; Bingham, S.; Buring, J. E.; Bracci, P. M.; Canzian, F.; Clavel-Chapelon, F. O.; Clipp, S.; Cotterchio, M.; De Andrade, M.; Duell, E. J.; Fox Jr, J. W.; Gallinger, S.; Gaziano, J. M.; Giovannucci, E. L.; Goggins, M. (2009). "Genome-wide association study identifies variants in the ABO locus associated with susceptibility to pancreatic cancer". Nature Genetics. 41 (9): 986–990. doi:10.1038/ng.429. PMC 2839871. PMID 19648918.
- ↑ Gates, MA; Wolpin, BM; Cramer, DW; Hankinson, SE; Tworoger, SS (2010). "ABO blood group and incidence of epithelial ovarian cancer". International Journal of Cancer. 128 (2): 482–486. doi:10.1002/ijc.25339. PMC 2946962. PMID 20309936.
- ↑ Aird, I; Bentall, HH; Roberts, JA (1953). "A relationship between cancer of stomach and the ABO blood groups". British Medical Journal. 1 (4814): 799–801. doi:10.1136/bmj.1.4814.799. PMC 2015995. PMID 13032504.
- ↑ Glass, Roger; Holmgren J; Haley C; Khan M.R.; SVENERHOLM M; STOLL B; HOSSAIN K; BLACK B; Yunus M; Barua D (June 1985). "Predisposition for cholera of individuals with O blood group. Possible evolutionary significance". American Journal of Epidemiology. 121 (6): 791–796. PMID 4014172. Retrieved 20 August 2012.
- ↑ Goldman, M (2016-10-10). "Translational Mini-Review Series on Toll-like Receptors: Toll-like receptor ligands as novel pharmaceuticals for allergic disorders". Clinical and Experimental Immunology. 147 (2): 208–216. doi:10.1111/j.1365-2249.2006.03296.x. ISSN 0009-9104. PMC 1810467. PMID 17223960.
- ↑ Kay, H E (1982-11-06). "Bone marrow transplantation: 1982". British Medical Journal (Clinical Research Ed.). 285 (6351): 1296–1298. doi:10.1136/bmj.285.6351.1296. ISSN 0267-0623. PMC 1500229. PMID 6812684.
- ↑ Hakomori, S. (1999-12-06). "Antigen structure and genetic basis of histo-blood groups A, B and O: their changes associated with human cancer". Biochimica et Biophysica Acta. 1473 (1): 247–266. doi:10.1016/s0304-4165(99)00183-x. ISSN 0006-3002. PMID 10580143.
- ↑ 63.0 63.1 Dabelsteen, E.; Gao, S. (2005-01-01). "ABO blood-group antigens in oral cancer". Journal of Dental Research. 84 (1): 21–28. doi:10.1177/154405910508400103. ISSN 0022-0345. PMID 15615870.
- ↑ Dabelsteen, Erik (2002-02-01). "ABO blood group antigens in oral mucosa. What is new?". Journal of Oral Pathology & Medicine. 31 (2): 65–70. doi:10.1046/j.0904-2512.2001.00004.x. ISSN 0904-2512. PMID 11896825.
- ↑ Amundadottir, Laufey T. (2016-01-01). "Pancreatic Cancer Genetics". International Journal of Biological Sciences. 12 (3): 314–325. doi:10.7150/ijbs.15001. ISSN 1449-2288. PMC 4753160. PMID 26929738.
- ↑ Mega, Jessica L.; Stitziel, Nathan O.; Smith, J. Gustav; Chasman, Daniel I.; Caulfield, Mark J.; Devlin, James J.; Nordio, Francesco; Hyde, Craig L.; Cannon, Christopher P. (2015-06-06). "Genetic risk, coronary heart disease events, and the clinical benefit of statin therapy: an analysis of primary and secondary prevention trials". Lancet. 385 (9984): 2264–2271. doi:10.1016/S0140-6736(14)61730-X. ISSN 1474-547X. PMC 4608367. PMID 25748612.
- ↑ Liu, QP; Sulzenbacher G; Yuan H; Bennett EP; Pietz G; Saunders K; Spence J; Nudelman E; Levery SB; White T; Neveu JM; Lane WS; Bourne Y; Olsson ML; Henrissat B; Clausen H (April 2007). "Bacterial glycosidases for the production of universal red blood cells". Nat Biotechnol. 25 (4): 454–64. doi:10.1038/nbt1298. PMID 17401360.
- ↑ BBC
- ↑ American Red Cross, Southern California Blood Services Region (n.d.). "Answers to Commonly Asked Questions About Blood and Blood Banking" (PDF). Blood: The Basics: 4. Archived (PDF) from the original on 29 November 2007. Retrieved 16 November 2007.
- ↑ Sung Il Ryu, Young Woo Sohn (2007), A Review of Sociocultural, Behavioral, Biochemical Analyses on ABO Blood-Groups Typology, The Korean Journal of Social and Personality Psychology.
- ↑ Hobgood, Donna K. (2011). "Personality traits of aggression-submissiveness and perfectionism associate with ABO blood groups through catecholamine activities". Medical Hypotheses. 77 (2): 294–300. doi:10.1016/j.mehy.2011.04.039. PMID 21601990.
- ↑ Klein, Harvey G (7 March 2005). "Why Do People Have Different Blood Types?". Scientific American. Retrieved 16 November 2007.
- ↑ Kang, Sung-ha et al. (1997). Distribution of ABO Genotypes and Allele Frequencies in a Korean Population. Japanese Journal of Human Genetics, 42(2), Page 333. doi: 10.1007/BF02766955 Retrieved July 24, 2017, from link to the article.
Further reading
- Dean L (2005). "Chapter 5: The ABO blood group". Blood Groups and Red Cell Antigens. Retrieved 24 March 2007.
- Farr A (1 April 1979). "Blood group serology--the first four decades (1900--1939)". Med Hist. 23 (2): 215–26. doi:10.1017/s0025727300051383. PMC 1082436. PMID 381816.
External links
- ABO at BGMUT Blood Group Antigen Gene Mutation Database at NCBI, NIH
- ABO blood groups, antibodies and antigens explained YouTube educational video
- Encyclopædia Britannica, ABO blood group system
- National Blood Transfusion Service
- Molecular Genetic Basis of ABO
- CS1 maint: Unrecognized language
- Use dmy dates from April 2014
- Articles with invalid date parameter in template
- Pages with broken file links
- All articles with unsourced statements
- Articles with unsourced statements from November 2013
- Blood antigen systems
- Transfusion medicine
- Antigenic determinant
- Hematopathology
- Glycoproteins
- Serology
- Genes on human chromosome 9