COVID-19-associated meningitis: Difference between revisions
No edit summary |
|||
| (87 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
'''For COVID-19 frequently asked outpatient questions, click [[COVID-19 frequently asked outpatient questions|here]]'''. | |||
'''For COVID-19 frequently asked inpatient questions, click [[COVID-19 frequently asked inpatient questions|here]]'''. | |||
'''For COVID-19 patient information, click [[COVID-19 (patient information)|here]]'''. | |||
__NOTOC__ | __NOTOC__ | ||
{{ | {{SI}} | ||
{{CMG}}; {{AE}} {{Wd}}, {{MAH}} [[User:Tayebah Chaudhry|Tayebah Chaudhry]][mailto:dr.thch@yahoo.com] {{Fs}}, {{sali}} | |||
==Overview== | ==Overview== | ||
Covid-19 associated meningitis was first discovered by Moriguchi T. et al. a Japanese [[critical care]] [[physician]] in late February 2020 during the [[pandemic]] of [[SARS-CoV-2]]. Duong L et. reported a case of a young female with COVID-19 who developed [[meningoencephalitis]] without [[respiratory failure]] in Downtown Los Angeles in early April, 2020. Bernard-Valnet R et al. reported two cases of [[meningoencephalitis]] in [[patients]] with concomitant [[SARS-CoV-2]] infection. There is no established system for the classification of [[SARS-CoV-2]] related meningitis. There are three mechanisms proposed for pathophysiology of COVID-19-associated meningitis. [[SARS-CoV-2]] directly reaches brain through [[cribriform plate]] which is located in close proximity to [[olfactory bulb]]. This is supported by the facts that some [[patients]] of [[COVID-19]] present with [[anosmia]] and [[hyposmia]]. Viral interaction with [[ACE|ACE2]] expressed on [[neurons]] lead to damage to [[neurons]] and inflamation ([[encephalitis]]) and [[inflammation]] of [[Meninges|brain membranes]] ([[meningitis]]). [[SARS-CoV-2]] can reach [[brain]] via anterograde or retrograde transport with the help of motor proteins [[kinesin]] and [[dynein]] via sensory nerve endings, especially afferent [[Nerve ending|nerve endings]] of [[vagus nerve]] from [[Lung|lungs]]. | |||
==Historical Perspective== | ==Historical Perspective== | ||
* | *[[Neurological]] [[symptoms]] in [[COVID-19]] patients were first reported in February 2020 in a retrospective case series study by Mao L. et al. in hospitalized COVID-19 patients in Wuhan. | ||
* | *Ling Mao from Tongji Medical College in Wuhan, and his group reviewed the data retrospectively from January 16, 2020, to February 19, 2020. | ||
* Duong L et. reported a case of a young female with COVID-19 who developed [[meningoencephalitis]] without respiratory failure in Downtown Los Angeles in early April, 2020 <ref name="pmid32305574">{{cite journal| author=Duong L, Xu P, Liu A| title=Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in Downtown Los Angeles, early April 2020. | journal=Brain Behav Immun | year= 2020 | volume= 87 | issue= | pages= 33 | pmid=32305574 | doi=10.1016/j.bbi.2020.04.024 | pmc=7162766 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32305574 }}</ref>. | *One third of the 214 hospitalized laboratory- confirmed [[COVID-19]] patients included in this study reported at least one [[neurological]] [[symptom]]. | ||
* Bernard-Valnet R et al. reported two cases of meningoencephalitis in patients with concomitant SARS-CoV-2 infection <ref name="pmid32383343">{{cite journal| author=Bernard-Valnet R, Pizzarotti B, Anichini A, Demars Y, Russo E, Schmidhauser M | display-authors=etal| title=Two patients with acute meningoencephalitis concomitant with SARS-CoV-2 infection. | journal=Eur J Neurol | year= 2020 | volume= | issue= | pages= | pmid=32383343 | doi=10.1111/ene.14298 | pmc=7267660 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32383343 }}</ref> | * Covid-19 associated meningitis was first discovered by Moriguchi T. et al. a Japanese [[critical care]] [[physician]] in late February 2020 during the [[pandemic]] of [[SARS]]-[[Coronavirus]]-2: [[SARS-CoV-2]] <ref name="pmid32251791">{{cite journal| author=Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J | display-authors=etal| title=A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. | journal=Int J Infect Dis | year= 2020 | volume= 94 | issue= | pages= 55-58 | pmid=32251791 | doi=10.1016/j.ijid.2020.03.062 | pmc=7195378 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32251791 }}</ref>. | ||
* Duong L et. reported a case of a young female with COVID-19 who developed [[meningoencephalitis]] without [[Respiratory failure CT|respiratory failure]] in Downtown Los Angeles in early April, 2020 <ref name="pmid32305574">{{cite journal| author=Duong L, Xu P, Liu A| title=Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in Downtown Los Angeles, early April 2020. | journal=Brain Behav Immun | year= 2020 | volume= 87 | issue= | pages= 33 | pmid=32305574 | doi=10.1016/j.bbi.2020.04.024 | pmc=7162766 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32305574 }}</ref>. | |||
* Bernard-Valnet R et al. reported two cases of [[meningoencephalitis]] in patients with concomitant [[SARS-CoV-2]] infection.<ref name="pmid32383343">{{cite journal| author=Bernard-Valnet R, Pizzarotti B, Anichini A, Demars Y, Russo E, Schmidhauser M | display-authors=etal| title=Two patients with acute meningoencephalitis concomitant with SARS-CoV-2 infection. | journal=Eur J Neurol | year= 2020 | volume= | issue= | pages= | pmid=32383343 | doi=10.1111/ene.14298 | pmc=7267660 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32383343 }}</ref> | |||
==Classification== | ==Classification== | ||
There is no established system for the classification of | |||
* There is no established system for the classification of COVID-19-associated meningitis. | |||
== Pathophysiology == | == Pathophysiology == | ||
The exact pathogenesis of COVID-19-associated meningitis is not fully understood. | |||
* Severe acute respiratory syndrome ([[Severe acute respiratory syndrome|SARS]]) and Middle East respiratory Syndrome ([[MERS]]) caused some neurological manifestations in 2002 and 2012 respectively<ref name="pmid16252612">{{cite journal| author=Tsai LK, Hsieh ST, Chang YC| title=Neurological manifestations in severe acute respiratory syndrome. | journal=Acta Neurol Taiwan | year= 2005 | volume= 14 | issue= 3 | pages= 113-9 | pmid=16252612 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16252612 }}</ref>. | |||
*As [[neucleic acid]] of [[SARS-CoV]] and [[MERS-CoV]] was found in [[cerebrospinal fluid]] and later on the [[autopsy]] of brain<ref name="pmid311330312">{{cite journal| author=Schoeman D, Fielding BC| title=Coronavirus envelope protein: current knowledge. | journal=Virol J | year= 2019 | volume= 16 | issue= 1 | pages= 69 | pmid=31133031 | doi=10.1186/s12985-019-1182-0 | pmc=6537279 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31133031 }}</ref>. | |||
*[[SARS-CoV-2]] is 79% identical to SARS-CoV and 50% to [[MERS-CoV]]. <ref name="pmid32007145">{{cite journal| author=Lu R, Zhao X, Li J, Niu P, Yang B, Wu H | display-authors=etal| title=Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. | journal=Lancet | year= 2020 | volume= 395 | issue= 10224 | pages= 565-574 | pmid=32007145 | doi=10.1016/S0140-6736(20)30251-8 | pmc=7159086 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32007145 }}</ref> Due to structural [[homology]] it is safe to say that SARS-CoV-2 causes neurological problems by the same mechanism as caused by [[SARS-CoV]] and [[MERS-CoV]]. | |||
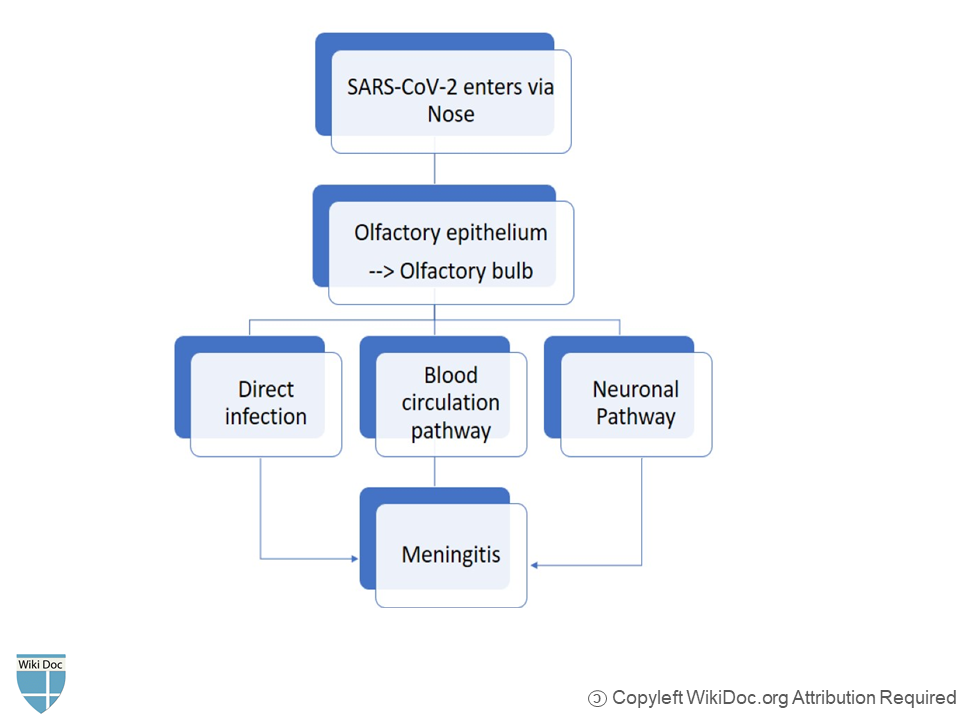
The proposed pathophysiology of COVID-19-associated meningitis is by following three mechanisms; | |||
'''1.Direct pathway''' | |||
* [[SARS-CoV-2]] directly reaches brain through [[cribriform plate]] which is located in close proximity to [[olfactory bulb]]<ref name="pmid32167747">{{cite journal| author=Baig AM, Khaleeq A, Ali U, Syeda H| title=Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms. | journal=ACS Chem Neurosci | year= 2020 | volume= 11 | issue= 7 | pages= 995-998 | pmid=32167747 | doi=10.1021/acschemneuro.0c00122 | pmc=7094171 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32167747 }}</ref>. | |||
* This is supported by the facts that some [[patients]] of COVID-19 present with [[anosmia]] and [[hyposmia]]. | |||
'''2. Blood circulation pathway''' | '''2. Blood circulation pathway''' | ||
* Angiotensin converting enzyme-2 (ACE2) is the functional receptor of the SARS-CoV-2<ref name="pmid24172901">{{cite journal| author=Ge XY, Li JL, Yang XL, Chmura AA, Zhu G, Epstein JH | display-authors=etal| title=Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor. | journal=Nature | year= 2013 | volume= 503 | issue= 7477 | pages= 535-8 | pmid=24172901 | doi=10.1038/nature12711 | pmc=5389864 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24172901 }}</ref> | *[[Angiotensin converting enzyme|Angiotensin converting enzyme-2]] (ACE2) is the functional receptor of the [[SARS-CoV-2]]. <ref name="pmid24172901">{{cite journal| author=Ge XY, Li JL, Yang XL, Chmura AA, Zhu G, Epstein JH | display-authors=etal| title=Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor. | journal=Nature | year= 2013 | volume= 503 | issue= 7477 | pages= 535-8 | pmid=24172901 | doi=10.1038/nature12711 | pmc=5389864 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24172901 }}</ref> [[ACE|ACE2]] is expressed on [[Glial cell|glial tissue]], [[neurons]] and [[brain]] vasculature. <ref name="pmid15165741">{{cite journal| author=Turner AJ, Hiscox JA, Hooper NM| title=ACE2: from vasopeptidase to SARS virus receptor. | journal=Trends Pharmacol Sci | year= 2004 | volume= 25 | issue= 6 | pages= 291-4 | pmid=15165741 | doi=10.1016/j.tips.2004.04.001 | pmc=7119032 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15165741 }}</ref> | ||
* SARS-CoV-2 binds with ACE2 precsent on vascular endothelial cells and glial tissues with the help of spike S protein.<ref name="pmid32075877">{{cite journal| author=Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O | display-authors=etal| title=Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. | journal=Science | year= 2020 | volume= 367 | issue= 6483 | pages= 1260-1263 | pmid=32075877 | doi=10.1126/science.abb2507 | pmc=7164637 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32075877 }}</ref> | *[[SARS-CoV-2]] binds with [[ACE|ACE2]] precsent on vascular [[endothelial cells]] and [[Glial cell|glial tissues]] with the help of spike S protein.<ref name="pmid32075877">{{cite journal| author=Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O | display-authors=etal| title=Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. | journal=Science | year= 2020 | volume= 367 | issue= 6483 | pages= 1260-1263 | pmid=32075877 | doi=10.1126/science.abb2507 | pmc=7164637 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32075877 }}</ref> | ||
* Subsequent viral budding from endothelial cells and resultant damage to capillary [[endothelium]] favors viral entry into milieu of brain<ref name="pmid321677472">{{cite journal| author=Baig AM, Khaleeq A, Ali U, Syeda H| title=Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms. | journal=ACS Chem Neurosci | year= 2020 | volume= 11 | issue= 7 | pages= 995-998 | pmid=32167747 | doi=10.1021/acschemneuro.0c00122 | pmc=7094171 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32167747 }}</ref>. | * Subsequent viral budding from endothelial cells and resultant damage to capillary [[endothelium]] favors viral entry into milieu of brain<ref name="pmid321677472">{{cite journal| author=Baig AM, Khaleeq A, Ali U, Syeda H| title=Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms. | journal=ACS Chem Neurosci | year= 2020 | volume= 11 | issue= 7 | pages= 995-998 | pmid=32167747 | doi=10.1021/acschemneuro.0c00122 | pmc=7094171 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32167747 }}</ref>. | ||
* Viral interaction with ACE2 expressed on neurons lead to damage to neurons and inflamation (encephalitis) and inflammation of brain membranes (meningitis) | * Viral interaction with [[Angiotensin-converting enzyme|ACE2]] expressed on [[Neuron|neurons]] lead to damage to [[Neuron|neurons]] and [[inflamation]] ([[encephalitis]]) and [[inflammation]] of [[Meninges|brain membranes]] ([[meningitis]]). | ||
'''3. Neuronal Pathway''' | '''3. Neuronal Pathway''' | ||
* SARS-CoV-2 can reach brain via anterograde or retrograde transoport with the help of motor proteins [[kinesin]] and [[dynein]] via sensory nerve endings, especially afferent nerve | *[[SARS-CoV-2]] can reach [[brain]] via anterograde or retrograde transoport with the help of motor proteins [[kinesin]] and [[dynein]] via sensory [[Nerve ending|nerve endings]], especially afferent [[nerve ending]]<nowiki/>s of [[vagus nerve]] from [[Lung|lungs]].<ref name="pmid25681709">{{cite journal| author=Swanson PA, McGavern DB| title=Viral diseases of the central nervous system. | journal=Curr Opin Virol | year= 2015 | volume= 11 | issue= | pages= 44-54 | pmid=25681709 | doi=10.1016/j.coviro.2014.12.009 | pmc=4456224 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25681709 }}</ref> | ||
* SARS-CoV-2 causes some gastrointestinal problems in COVID-19 patients and can reach CNS from enteric nerve and sympathetic afferent via neuronal pathway.<ref name="pmid32215956">{{cite journal| author=Wong SH, Lui RN, Sung JJ| title=Covid-19 and the digestive system. | journal=J Gastroenterol Hepatol | year= 2020 | volume= 35 | issue= 5 | pages= 744-748 | pmid=32215956 | doi=10.1111/jgh.15047 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32215956 }}</ref> | *[[SARS-CoV-2]] causes some [[gastrointestinal]] problems in COVID-19 [[Patient|patients]] and can reach [[CNS]] from enteric nerve and sympathetic afferent via neuronal pathway.<ref name="pmid32215956">{{cite journal| author=Wong SH, Lui RN, Sung JJ| title=Covid-19 and the digestive system. | journal=J Gastroenterol Hepatol | year= 2020 | volume= 35 | issue= 5 | pages= 744-748 | pmid=32215956 | doi=10.1111/jgh.15047 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32215956 }}</ref> | ||
* Exosomal cellular transport is also a pathway for SARS-CoV-2 systemic dissemination and spread to CNS.<ref name="pmid26393640">{{cite journal| author=Alenquer M, Amorim MJ| title=Exosome Biogenesis, Regulation, and Function in Viral Infection. | journal=Viruses | year= 2015 | volume= 7 | issue= 9 | pages= 5066-83 | pmid=26393640 | doi=10.3390/v7092862 | pmc=4584306 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26393640 }}</ref> | * Exosomal cellular transport is also a pathway for [[SARS-CoV-2]] systemic dissemination and spread to [[CNS]].<ref name="pmid26393640">{{cite journal| author=Alenquer M, Amorim MJ| title=Exosome Biogenesis, Regulation, and Function in Viral Infection. | journal=Viruses | year= 2015 | volume= 7 | issue= 9 | pages= 5066-83 | pmid=26393640 | doi=10.3390/v7092862 | pmc=4584306 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26393640 }}</ref> | ||
[[File:Meningitis Pathophysiology.png|center|600x600px]] | |||
<br /> | <br /> | ||
==Causes== | ==Causes== | ||
Meningitis in COVID-19 patients is caused by SARS-CoV-2 virus. | |||
* [[Meningitis]] in [[COVID-19]] patients is caused by [[SARS-CoV-2]] [[virus]]. | |||
==Differentiating COVID-19-associated meningitis from other Diseases== | ==Differentiating COVID-19-associated meningitis from other Diseases== | ||
* For further information about the differential diagnosis, [[COVID-19-associated meningitis differential diagnosis|click here]]. | |||
* To view the differential diagnosis of COVID-19, [[COVID-19 differential diagnosis|click here]]. | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
* More data is needed to establish the understanding of the [[epidemiology]] of COVID-19 associated meningitis<ref name="pmid32565914">{{cite journal |vauthors=Tsivgoulis G, Palaiodimou L, Katsanos AH, Caso V, Köhrmann M, Molina C, Cordonnier C, Fischer U, Kelly P, Sharma VK, Chan AC, Zand R, Sarraj A, Schellinger PD, Voumvourakis KI, Grigoriadis N, Alexandrov AV, Tsiodras S |title=Neurological manifestations and implications of COVID-19 pandemic |journal=Ther Adv Neurol Disord |volume=13 |issue= |pages=1756286420932036 |date=2020 |pmid=32565914 |pmc=7284455 |doi=10.1177/1756286420932036 |url=}}</ref>. | |||
* However, direct [[infection]] of the [[Neurology|neurological system]] appears to be extremely rare. | |||
* To view [[epidemiology]] and [[demographics]] for COVID-19, [[COVID-19 epidemiology and demographics|click here]]. | |||
[ | |||
[ | |||
==Risk Factors== | ==Risk Factors== | ||
* [[Risk factors]] for this [[disease]] are the same as for [[COVID-19]]. | |||
* To view the risk factors of COVID-19, [[COVID-19 risk factors|click here]]. | |||
== Screening == | |||
* There is insufficient evidence to recommend routine [[screening]] for COVID-19-associated meningitis. | |||
* To view screening for COVID-19, [[COVID-19 screening|click here]]. | |||
==Natural History, Complications, and Prognosis== | ==Natural History, Complications, and Prognosis== | ||
'''History''' | |||
* If left untreated, COVID-19-associated meningitis may cause long term neurological [[Complication (medicine)|complications]]. | |||
* To view Natural History for COVID-19, [[COVID-19 natural history, complications and prognosis|click here]].<br /> | |||
'''Complications''' | |||
If left untreated, meningitis in COVID-19 patients may develop following [[complications]]. | |||
* [[Encephalitis]] | |||
* [[Encephalopathy]] | |||
* [[Psychomotor]] changes | |||
* Uncontrolled [[Seizure|seizures]] | |||
* [[Cerebral vasculitis]] | |||
* [[Cranial nerves]] involvement | |||
* [[Sepsis]] (However more common in [[bacterial meningitis]], sepsis can be caused by viral meningitis) | |||
* [[Herniation]] of swollen brain tissue | |||
* [[Hydrocephalus]] | |||
* [[coma]]/ death | |||
* To view Complications for COVID-19, [[COVID-19 natural history, complications and prognosis|click here]].<br /> | |||
Prognosis is | '''Prognosis''' | ||
* Exact [[prognosis]] of COVID-19 associated meningitis is not known. | |||
*However, treating the underlying cause i.e., [[COVID-19]], including treatment with [[steroids]], have shown improvement in meningitis symptoms in a COVID-19 patient. | |||
* To view Prognosis for COVID-19, [[COVID-19 natural history, complications and prognosis|click here]]. | |||
==Diagnosis== | ==Diagnosis== | ||
===Diagnostic Study of Choice=== | ===Diagnostic Study of Choice=== | ||
The diagnostic study of choice for meningitis | * The diagnostic study of choice for meningitis in COVID-19 patients is [[CSF analysis]] and ruling out other causes of meningitis (e.g., other viruses, bacteria, fungi). | ||
===History and Symptoms=== | ===History and Symptoms=== | ||
'''History''' | |||
* The disease course of 5 cases of COVID-19 associated meningitis include: | |||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center; | ! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Patient No.</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center; | ! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Early symptoms</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center; | ! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Late symptoms</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center; | ! colspan="3" style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>CSF analysis</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center; | ! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Viral panel (HSV,VZV, enterovirus)</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" colspan="2" |<small>SARS-CoV-2 analysis</small> | ! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Bacterial panel | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center; | ! colspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>SARS-CoV-2 analysis</small> | ||
! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Imaging CT/MRI</small> | |||
|- | |- | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Protein</small> | ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Protein</small>(mg/L) | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Glucose</small> | ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Glucose</small>(CSF:serum ratio) | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Cells< | ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Cells (mm<sup>3</sup>)</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>RT-PCR CSF</small> | ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>RT-PCR CSF</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>RT-PCR Nasopharyngeal swab</small> | ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>RT-PCR Nasopharyngeal swab</small> | ||
|- | |- | ||
| | | | ||
| Line 245: | Line 206: | ||
anosmia | anosmia | ||
|Severe headache | |Severe headache | ||
neck | neck stiffness | ||
confusion | confusion | ||
| Line 276: | Line 237: | ||
|NA | |NA | ||
|positive | |positive | ||
|CT head without contrast was | |CT head without contrast was normal | ||
| | |- | ||
|} | |} | ||
'''Common Symptoms''' | |||
*[[Fever]] | |||
*[[Headache]] | |||
*[[Nausea]]/ [[vomiting]] | |||
*[[Irritability]] | |||
*[[Malaise]] | |||
*[[Neck stiffness]] | |||
* Light sensitivity/ [[photophobia]] | |||
Common | '''Less Common Symptoms''' | ||
*[[Myalgias]] | |||
*[[Confusion]] | |||
*[[Seizures]] (with concomitant [[encephalitis]]) | |||
===Physical Examination=== | |||
'''Vitals:''' | |||
*[[Fever]] | |||
* [[Tachycardia]] | |||
* Increased [[respiratory rate]] | |||
'''Neuromuscular:''' | |||
* [[Altered mental status]] | |||
* [[Photophobia]] | |||
*[[Neck stiffness|Neck rigidity]] | |||
* Positive [[Kernig's sign|Kernig sign]] | |||
* Positive [[Brudzinski's sign]] | |||
===Laboratory Findings=== | ===Laboratory Findings=== | ||
* [[Blood test]] including [[C-reactive protein]], [[Complete Blood Count]], and [[blood culture]] may determine the cause of meningitis. <ref name="pmid15494903">{{cite journal |vauthors=Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM, Whitley RJ |title=Practice guidelines for the management of bacterial meningitis |journal=Clin. Infect. Dis. |volume=39 |issue=9 |pages=1267–84 |date=November 2004 |pmid=15494903 |doi=10.1086/425368 |url=}}</ref> <ref name="pmid18582342">{{cite journal |vauthors=Chaudhuri A, Martinez-Martin P, Martin PM, Kennedy PG, Andrew Seaton R, Portegies P, Bojar M, Steiner I |title=EFNS guideline on the management of community-acquired bacterial meningitis: report of an EFNS Task Force on acute bacterial meningitis in older children and adults |journal=Eur. J. Neurol. |volume=15 |issue=7 |pages=649–59 |date=July 2008 |pmid=18582342 |doi=10.1111/j.1468-1331.2008.02193.x |url=}}</ref> | |||
*[[Lumbar puncture|Lumbar Puncture]] may show [[lymphocyte]]-predominant [[CSF]] with normal [[Glucose-1-phosphatase|glucose]] and normal to high [[protein]]. <ref name="pmid15494903">{{cite journal |vauthors=Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM, Whitley RJ |title=Practice guidelines for the management of bacterial meningitis |journal=Clin. Infect. Dis. |volume=39 |issue=9 |pages=1267–84 |date=November 2004 |pmid=15494903 |doi=10.1086/425368 |url=}}</ref> | |||
* COVID-19 meningitis is differentiated from other causes of [[meningitis]] by the following [[CSF]] findings:<ref name="pmid23717798">{{cite journal| author=Le Rhun E, Taillibert S, Chamberlain MC| title=Carcinomatous meningitis: Leptomeningeal metastases in solid tumors. | journal=Surg Neurol Int | year= 2013 | volume= 4 | issue= Suppl 4 | pages= S265-88 | pmid=23717798 | doi=10.4103/2152-7806.111304 | pmc=3656567 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23717798 }}</ref><ref name="pmid24326618">{{cite journal| author=Chow E, Troy SB| title=The differential diagnosis of hypoglycorrhachia in adult patients. | journal=Am J Med Sci | year= 2014 | volume= 348 | issue= 3 | pages= 186-90 | pmid=24326618 | doi=10.1097/MAJ.0000000000000217 | pmc=4065645 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24326618 }}</ref><ref name="pmid22880096">{{cite journal| author=Leen WG, Willemsen MA, Wevers RA, Verbeek MM| title=Cerebrospinal fluid glucose and lactate: age-specific reference values and implications for clinical practice. | journal=PLoS One | year= 2012 | volume= 7 | issue= 8 | pages= e42745 | pmid=22880096 | doi=10.1371/journal.pone.0042745 | pmc=3412827 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22880096 }}</ref><ref name="pmid10654948">{{cite journal| author=Negrini B, Kelleher KJ, Wald ER| title=Cerebrospinal fluid findings in aseptic versus bacterial meningitis. | journal=Pediatrics | year= 2000 | volume= 105 | issue= 2 | pages= 316-9 | pmid=10654948 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10654948 }}</ref><ref name="pmid20610819">{{cite journal| author=Brouwer MC, Tunkel AR, van de Beek D| title=Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis. | journal=Clin Microbiol Rev | year= 2010 | volume= 23 | issue= 3 | pages= 467-92 | pmid=20610819 | doi=10.1128/CMR.00070-09 | pmc=2901656 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20610819 }}</ref> | |||
{| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | |||
! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF|Cerebrospinal fluid level}} | |||
! style="background: #4479BA; width: 350px;" |{{fontcolor|#FFF|Normal level}} | |||
[ | ! style="background: #4479BA; width: 350px;" |{{fontcolor|#FFF|Bacterial meningitis}}<ref name="pmid10654948">{{cite journal| author=Negrini B, Kelleher KJ, Wald ER| title=Cerebrospinal fluid findings in aseptic versus bacterial meningitis. | journal=Pediatrics | year= 2000 | volume= 105 | issue= 2 | pages= 316-9 | pmid=10654948 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10654948 }} </ref> | ||
! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF|SARS-CoV-2 meningitis}} | |||
! style="background: #4479BA; width: 350px;" |{{fontcolor|#FFF|Viral meningitis}}<ref name="pmid10654948">{{cite journal| author=Negrini B, Kelleher KJ, Wald ER| title=Cerebrospinal fluid findings in aseptic versus bacterial meningitis. | journal=Pediatrics | year= 2000 | volume= 105 | issue= 2 | pages= 316-9 | pmid=10654948 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10654948 }} </ref> | |||
! style="background: #4479BA; width: 350px;" |{{fontcolor|#FFF|Fungal meningitis}} | |||
! style="background: #4479BA; width: 350px;" |{{fontcolor|#FFF|Tuberculous meningitis}}<ref name="pmid20146981">{{cite journal| author=Caudie C, Tholance Y, Quadrio I, Peysson S| title=[Contribution of CSF analysis to diagnosis and follow-up of tuberculous meningitis]. | journal=Ann Biol Clin (Paris) | year= 2010 | volume= 68 | issue= 1 | pages= 107-11 | pmid=20146981 | doi=10.1684/abc.2010.0407 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20146981 }}</ref> | |||
! style="background: #4479BA; width: 350px;" |{{fontcolor|#FFF|Malignant meningitis}}<ref name="pmid23717798">{{cite journal| author=Le Rhun E, Taillibert S, Chamberlain MC| title=Carcinomatous meningitis: Leptomeningeal metastases in solid tumors. | journal=Surg Neurol Int | year= 2013 | volume= 4 | issue= Suppl 4 | pages= S265-88 | pmid=23717798 | doi=10.4103/2152-7806.111304 | pmc=3656567 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23717798 }} </ref> | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" |'''Cells/ul''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" |< 5 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |>300 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |10-1000 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |10-1000 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |10-500 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |50-500 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |>4 | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" |'''Cells''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" |Lymphos:Monos 7:3 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |Gran. > Lymph | |||
| style="padding: 5px 5px; background: #F5F5F5;" |predominantly [[Lymphocyte|lymphocytes]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" |Lymph. > Gran. | |||
| style="padding: 5px 5px; background: #F5F5F5;" |Lympho.>Gran | |||
| style="padding: 5px 5px; background: #F5F5F5;" |[[Lymphocyte|Lymphocytes]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" |Lymphocytes | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" |'''Total protein (mg/dl)''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" |45-60 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |Typically 100-500 | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Normal or slightly high | |||
| style="padding: 5px 5px; background: #F5F5F5;" |Normal or slightly high | |||
| style="padding: 5px 5px; background: #F5F5F5;" |High | |||
| style="padding: 5px 5px; background: #F5F5F5;" |Typically 100-200 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |>50 | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" |'''Glucose ratio (CSF/plasma)<ref name="pmid24326618">{{cite journal| author=Chow E, Troy SB| title=The differential diagnosis of hypoglycorrhachia in adult patients. | journal=Am J Med Sci | year= 2014 | volume= 348 | issue= 3 | pages= 186-90 | pmid=24326618 | doi=10.1097/MAJ.0000000000000217 | pmc=4065645 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24326618 }} </ref>''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" |> 0.5 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |< 0.3 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |> 0.6 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |> 0.6 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |<0.3 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |< 0.5 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |<0.5 | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" |'''Lactate (mmols/l)<ref name="pmid22880096">{{cite journal| author=Leen WG, Willemsen MA, Wevers RA, Verbeek MM| title=Cerebrospinal fluid glucose and lactate: age-specific reference values and implications for clinical practice. | journal=PLoS One | year= 2012 | volume= 7 | issue= 8 | pages= e42745 | pmid=22880096 | doi=10.1371/journal.pone.0042745 | pmc=3412827 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22880096 }} </ref>''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" |< 2.1 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |> 2.1 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |N/A | |||
| style="padding: 5px 5px; background: #F5F5F5;" |< 2.1 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |>3.2 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |> 2.1 | |||
| style="padding: 5px 5px; background: #F5F5F5;" |>2.1 | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" |'''Others''' | |||
| style="padding: 5px 5px; background: #F5F5F5;" |ICP:6-12 (cm H2O) | |||
| style="padding: 5px 5px; background: #F5F5F5;" |[[CSF]] [[Gram staining|gram stain]], [[CSF]] culture, [[CSF]] bacterial antigen | |||
| style="padding: 5px 5px; background: #F5F5F5;" |[[RT-PCR]] for [[SARS-CoV-2]] [[RNA]] in [[CSF]] (still not approved by FDA) | |||
| style="padding: 5px 5px; background: #F5F5F5;" |[[Polymerase chain reaction|PCR]] of [[Herpes simplex virus|HSV]]-[[DNA]], [[VZV]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" |[[CSF]] [[Gram staining|gram stain]], [[CSF]] india ink | |||
| style="padding: 5px 5px; background: #F5F5F5;" |PCR of TBC-DNA | |||
| style="padding: 5px 5px; background: #F5F5F5;" |CSF tumour markers such as alpha fetoproteins, CEA | |||
|- | |||
|} | |||
===Electrocardiogram=== | ===Electrocardiogram=== | ||
* To view the [[electrocardiogram]] findings on COVID-19, [[COVID-19 electrocardiogram|click here]]. | |||
*There are no [[ECG]] findings associated with COVID-19-associated meningitis | |||
===X-ray=== | ===X-ray=== | ||
There are no x-ray findings associated with | * There are no [[X-rays|x-ray]] findings associated with COVID-19-associated meningitis. | ||
* To view the [[x-ray]] finidings on COVID-19, [[COVID-19 x ray|click here]]. | |||
===Echocardiography or Ultrasound=== | ===Echocardiography or Ultrasound=== | ||
There are no | *There are no [[Echocardiography and ultrasound|echocardiography]]/[[ultrasound]] findings associated with COVID-19-associated meningitis. | ||
* To view the [[Echocardiography|echocardiographic]] findings on COVID-19, [[COVID-19 echocardiography and ultrasound|click here]]. | |||
Echocardiography | |||
===CT scan=== | ===CT scan=== | ||
*[[CT scan]] of the [[brain]] may detect brain [[inflammation]]. | |||
* To view the [[CT scan]] findings on COVID-19, [[COVID-19 CT scan|click here]]. | |||
===MRI=== | ===MRI=== | ||
*[[MRI]] of [[brain]] may show hyperintense areas due to brain inflammation. | |||
* To view other imaging findings on [[COVID-19]], [[COVID-19 other imaging findings|click here]].<br /> | |||
[ | |||
===Other Imaging Findings=== | ===Other Imaging Findings=== | ||
* There are no other imaging findings associated with COVID-19 associated meningitis. | |||
===Other Diagnostic Studies=== | ===Other Diagnostic Studies=== | ||
* There are no other diagnostic studies associated with COVID-19 associated meningitis. | |||
==Treatment== | ==Treatment== | ||
===Medical Therapy=== | === Medical Therapy=== | ||
The mainstays of [[medical]] [[therapy]] for viral meningitis are:<ref name="pmid322517913">{{cite journal| author=Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J | display-authors=etal| title=A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. | journal=Int J Infect Dis | year= 2020 | volume= 94 | issue= | pages= 55-58 | pmid=32251791 | doi=10.1016/j.ijid.2020.03.062 | pmc=7195378 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32251791 }}</ref><ref name="pmid32043983">{{cite journal |vauthors=Russell CD, Millar JE, Baillie JK |title=Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury |journal=Lancet |volume=395 |issue=10223 |pages=473–475 |date=February 2020 |pmid=32043983 |pmc=7134694 |doi=10.1016/S0140-6736(20)30317-2 |url=}}</ref><ref name="pmid32256705">{{cite journal| author=Russell B, Moss C, George G, Santaolalla A, Cope A, Papa S | display-authors=etal| title=Associations between immune-suppressive and stimulating drugs and novel COVID-19-a systematic review of current evidence. | journal=Ecancermedicalscience | year= 2020 | volume= 14 | issue= | pages= 1022 | pmid=32256705 | doi=10.3332/ecancer.2020.1022 | pmc=7105343 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32256705 }}</ref><ref name="pmid25174548">{{cite journal |vauthors=Ueda R, Saito Y, Ohno K, Maruta K, Matsunami K, Saiki Y, Sokota T, Sugihara S, Nishimura Y, Tamasaki A, Narita A, Imamura A, Maegaki Y |title=Effect of levetiracetam in acute encephalitis with refractory, repetitive partial seizures during acute and chronic phase |journal=Brain Dev. |volume=37 |issue=5 |pages=471–7 |date=May 2015 |pmid=25174548 |doi=10.1016/j.braindev.2014.08.003 |url=}}</ref><ref name="pmid32479911">{{cite journal| author=Efe IE, Aydin OU, Alabulut A, Celik O, Aydin K| title=COVID-19-Associated Encephalitis Mimicking Glial Tumor. | journal=World Neurosurg | year= 2020 | volume= 140 | issue= | pages= 46-48 | pmid=32479911 | doi=10.1016/j.wneu.2020.05.194 | pmc=7256557 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32479911 }}</ref><ref name="urlA Study to Evaluate the Efficacy and Safety of Tocilizumab in Hospitalized Participants With COVID-19 Pneumonia - Full Text View - ClinicalTrials.gov">{{cite web |url=+https://clinicaltrials.gov/ct2/show/NCT04372186 |title=A Study to Evaluate the Efficacy and Safety of Tocilizumab in Hospitalized Participants With COVID-19 Pneumonia - Full Text View - ClinicalTrials.gov |format= |work= |accessdate=}}</ref><ref name="pmid32234467">{{cite journal| author=Zhang C, Wu Z, Li JW, Zhao H, Wang GQ| title=Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality. | journal=Int J Antimicrob Agents | year= 2020 | volume= 55 | issue= 5 | pages= 105954 | pmid=32234467 | doi=10.1016/j.ijantimicag.2020.105954 | pmc=7118634 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32234467 }}</ref> | |||
=====Symptomatic treatments:===== | |||
*[[Anti-inflammatory]] drugs like [[steroids]] are helpful to decrease brain [[inflammation]] in COVID-19 associated meningitis. | |||
*[[Corticosteroids]] ([[methylprednisolone]] 300 mg/day) in severe [[COVID-19]] patients are shown to reduce [[mortality]]. | |||
* If a [[COVID-19]] patient with [[meningitis]] develops [[seizures]] [[anti-epileptic drugs]] like [[levetiracetam]] (50-60 mg/kg/day) may be necessary.. | |||
*[[Tocilizumab]] (8mg/kg/dose) is IL-6 anatgonist, that reduces cytokine storm syndrome responsible for neurological manifestations in a COVID-19 patient. | |||
*[[Intubation]] and [[mechanical ventilation]] may be needed . | |||
* To see treatment protocol to manage the underlying cause i.e., COVID-19, [[COVID-19 medical therapy|click here]].<br /> | |||
[ | |||
[ | |||
===Surgery=== | ===Surgery=== | ||
* In case of [[brain]] [[parenchyma]] involvement surgery can be done <ref name="pmid32479911" />. | |||
===Primary Prevention=== | ===Primary Prevention=== | ||
* There are no established measures for the [[primary prevention]] of [[COVID-19]] associated [[meningitis]]. | |||
* To view primary prevention for COVID-19 [[COVID-19 primary prevention|click here]].<br /> | |||
===Secondary Prevention=== | ===Secondary Prevention=== | ||
*There are no established measures for the [[secondary prevention]] of [[COVID-19]] associated [[meningitis]]. | |||
* To view secondary prevention for COVID-19 [[COVID-19 secondary prevention|click here]].<br /> | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Up-To-Date]] | |||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Latest revision as of 23:47, 12 December 2020
For COVID-19 frequently asked outpatient questions, click here.
For COVID-19 frequently asked inpatient questions, click here.
For COVID-19 patient information, click here.
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Wajeeha Aiman, M.D.[2], Muhammad Adnan Haider, M.B.B.S.[3] Tayebah Chaudhry[4] Fahimeh Shojaei, M.D., Syed Musadiq Ali M.B.B.S.[5]
Overview
Covid-19 associated meningitis was first discovered by Moriguchi T. et al. a Japanese critical care physician in late February 2020 during the pandemic of SARS-CoV-2. Duong L et. reported a case of a young female with COVID-19 who developed meningoencephalitis without respiratory failure in Downtown Los Angeles in early April, 2020. Bernard-Valnet R et al. reported two cases of meningoencephalitis in patients with concomitant SARS-CoV-2 infection. There is no established system for the classification of SARS-CoV-2 related meningitis. There are three mechanisms proposed for pathophysiology of COVID-19-associated meningitis. SARS-CoV-2 directly reaches brain through cribriform plate which is located in close proximity to olfactory bulb. This is supported by the facts that some patients of COVID-19 present with anosmia and hyposmia. Viral interaction with ACE2 expressed on neurons lead to damage to neurons and inflamation (encephalitis) and inflammation of brain membranes (meningitis). SARS-CoV-2 can reach brain via anterograde or retrograde transport with the help of motor proteins kinesin and dynein via sensory nerve endings, especially afferent nerve endings of vagus nerve from lungs.
Historical Perspective
- Neurological symptoms in COVID-19 patients were first reported in February 2020 in a retrospective case series study by Mao L. et al. in hospitalized COVID-19 patients in Wuhan.
- Ling Mao from Tongji Medical College in Wuhan, and his group reviewed the data retrospectively from January 16, 2020, to February 19, 2020.
- One third of the 214 hospitalized laboratory- confirmed COVID-19 patients included in this study reported at least one neurological symptom.
- Covid-19 associated meningitis was first discovered by Moriguchi T. et al. a Japanese critical care physician in late February 2020 during the pandemic of SARS-Coronavirus-2: SARS-CoV-2 [1].
- Duong L et. reported a case of a young female with COVID-19 who developed meningoencephalitis without respiratory failure in Downtown Los Angeles in early April, 2020 [2].
- Bernard-Valnet R et al. reported two cases of meningoencephalitis in patients with concomitant SARS-CoV-2 infection.[3]
Classification
- There is no established system for the classification of COVID-19-associated meningitis.
Pathophysiology
The exact pathogenesis of COVID-19-associated meningitis is not fully understood.
- Severe acute respiratory syndrome (SARS) and Middle East respiratory Syndrome (MERS) caused some neurological manifestations in 2002 and 2012 respectively[4].
- As neucleic acid of SARS-CoV and MERS-CoV was found in cerebrospinal fluid and later on the autopsy of brain[5].
- SARS-CoV-2 is 79% identical to SARS-CoV and 50% to MERS-CoV. [6] Due to structural homology it is safe to say that SARS-CoV-2 causes neurological problems by the same mechanism as caused by SARS-CoV and MERS-CoV.
The proposed pathophysiology of COVID-19-associated meningitis is by following three mechanisms;
1.Direct pathway
- SARS-CoV-2 directly reaches brain through cribriform plate which is located in close proximity to olfactory bulb[7].
2. Blood circulation pathway
- Angiotensin converting enzyme-2 (ACE2) is the functional receptor of the SARS-CoV-2. [8] ACE2 is expressed on glial tissue, neurons and brain vasculature. [9]
- SARS-CoV-2 binds with ACE2 precsent on vascular endothelial cells and glial tissues with the help of spike S protein.[10]
- Subsequent viral budding from endothelial cells and resultant damage to capillary endothelium favors viral entry into milieu of brain[11].
- Viral interaction with ACE2 expressed on neurons lead to damage to neurons and inflamation (encephalitis) and inflammation of brain membranes (meningitis).
3. Neuronal Pathway
- SARS-CoV-2 can reach brain via anterograde or retrograde transoport with the help of motor proteins kinesin and dynein via sensory nerve endings, especially afferent nerve endings of vagus nerve from lungs.[12]
- SARS-CoV-2 causes some gastrointestinal problems in COVID-19 patients and can reach CNS from enteric nerve and sympathetic afferent via neuronal pathway.[13]
- Exosomal cellular transport is also a pathway for SARS-CoV-2 systemic dissemination and spread to CNS.[14]
Causes
- Meningitis in COVID-19 patients is caused by SARS-CoV-2 virus.
Differentiating COVID-19-associated meningitis from other Diseases
- For further information about the differential diagnosis, click here.
- To view the differential diagnosis of COVID-19, click here.
Epidemiology and Demographics
- More data is needed to establish the understanding of the epidemiology of COVID-19 associated meningitis[15].
- However, direct infection of the neurological system appears to be extremely rare.
- To view epidemiology and demographics for COVID-19, click here.
Risk Factors
- Risk factors for this disease are the same as for COVID-19.
- To view the risk factors of COVID-19, click here.
Screening
- There is insufficient evidence to recommend routine screening for COVID-19-associated meningitis.
- To view screening for COVID-19, click here.
Natural History, Complications, and Prognosis
History
- If left untreated, COVID-19-associated meningitis may cause long term neurological complications.
- To view Natural History for COVID-19, click here.
Complications
If left untreated, meningitis in COVID-19 patients may develop following complications.
- Encephalitis
- Encephalopathy
- Psychomotor changes
- Uncontrolled seizures
- Cerebral vasculitis
- Cranial nerves involvement
- Sepsis (However more common in bacterial meningitis, sepsis can be caused by viral meningitis)
- Herniation of swollen brain tissue
- Hydrocephalus
- coma/ death
- To view Complications for COVID-19, click here.
Prognosis
- Exact prognosis of COVID-19 associated meningitis is not known.
- However, treating the underlying cause i.e., COVID-19, including treatment with steroids, have shown improvement in meningitis symptoms in a COVID-19 patient.
- To view Prognosis for COVID-19, click here.
Diagnosis
Diagnostic Study of Choice
- The diagnostic study of choice for meningitis in COVID-19 patients is CSF analysis and ruling out other causes of meningitis (e.g., other viruses, bacteria, fungi).
History and Symptoms
History
- The disease course of 5 cases of COVID-19 associated meningitis include:
| Patient No. | Early symptoms | Late symptoms | CSF analysis | Viral panel (HSV,VZV, enterovirus) | Bacterial panel | SARS-CoV-2 analysis | Imaging CT/MRI | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Protein(mg/L) | Glucose(CSF:serum ratio) | Cells (mm3) | RT-PCR CSF | RT-PCR Nasopharyngeal swab | ||||||
|
Headache,
Fever, fatigue |
Worsening headache, Sore throat. (Day 5)
Impaired consciousness and transient generalized seizure, (Day 9) |
NA | NA | Cell count was 12/μL–10 | Negative | Positive | Negative | Brain MRI:
Hyperintensity in the right lateral ventricle's inferior horn along the wall, | |
| 2. 64 year old female with a known contact with SARS-CoV-2 (her husband tested positive 15 days before)[17] | Mild flue like symptoms
myalgia cough |
Tonic-clonic seizures
disorientation psychotic symptoms |
466 mg/L | 0.59 | 17 cells with 97% lymphocytes | negative | negative | positive | Brain MRI normal at admission | |
| 3. 67 year old female with known SARS-CoV-2 for 17 days with mild respiratory symptoms[18] | wake up severe headache | Drowsiness, disoriented was lying on the floor, brought to hospital with confusion, disorientation, | 461
mg/L |
0.62 | 21 cells with 87 % cells were lymphocytes | negative | negative | positive | Brain MRI normal at admission | |
| 4. 69 year old man who returned from Middle East 15 days ago (French Indies)[19] | 7 day history of
fever cough myalgia cervical pain ageusia anosmia |
Severe headache
neck stiffness confusion |
84
mg/L |
normal | 37 cells, purely lymphocytes, with no RBCs | negative | neagtive | negative on nasopharyngeal swab but became positive on bronchoalveolar lavage on 4th day of admission | Brain MRI normal on admission | |
| 5. 41 year old female, presented with meningoencephalitis without respiratory failure in Downtown Los Angeles in April 2020[20] | fever
headache |
new onset seizure
severe headache neck stiffness photophobia |
100
mg/L |
0.60 | 70 cells with 100% lymphocytes | negative | NA | positive | CT head without contrast was normal | |
Common Symptoms
- Fever
- Headache
- Nausea/ vomiting
- Irritability
- Malaise
- Neck stiffness
- Light sensitivity/ photophobia
Less Common Symptoms
- Myalgias
- Confusion
- Seizures (with concomitant encephalitis)
Physical Examination
Vitals:
- Fever
- Tachycardia
- Increased respiratory rate
Neuromuscular:
- Altered mental status
- Photophobia
- Neck rigidity
- Positive Kernig sign
- Positive Brudzinski's sign
Laboratory Findings
- Blood test including C-reactive protein, Complete Blood Count, and blood culture may determine the cause of meningitis. [21] [22]
- Lumbar Puncture may show lymphocyte-predominant CSF with normal glucose and normal to high protein. [21]
- COVID-19 meningitis is differentiated from other causes of meningitis by the following CSF findings:[23][24][25][26][27]
| Cerebrospinal fluid level | Normal level | Bacterial meningitis[26] | SARS-CoV-2 meningitis | Viral meningitis[26] | Fungal meningitis | Tuberculous meningitis[28] | Malignant meningitis[23] |
|---|---|---|---|---|---|---|---|
| Cells/ul | < 5 | >300 | 10-1000 | 10-1000 | 10-500 | 50-500 | >4 |
| Cells | Lymphos:Monos 7:3 | Gran. > Lymph | predominantly lymphocytes | Lymph. > Gran. | Lympho.>Gran | Lymphocytes | Lymphocytes |
| Total protein (mg/dl) | 45-60 | Typically 100-500 | Normal or slightly high | Normal or slightly high | High | Typically 100-200 | >50 |
| Glucose ratio (CSF/plasma)[24] | > 0.5 | < 0.3 | > 0.6 | > 0.6 | <0.3 | < 0.5 | <0.5 |
| Lactate (mmols/l)[25] | < 2.1 | > 2.1 | N/A | < 2.1 | >3.2 | > 2.1 | >2.1 |
| Others | ICP:6-12 (cm H2O) | CSF gram stain, CSF culture, CSF bacterial antigen | RT-PCR for SARS-CoV-2 RNA in CSF (still not approved by FDA) | PCR of HSV-DNA, VZV | CSF gram stain, CSF india ink | PCR of TBC-DNA | CSF tumour markers such as alpha fetoproteins, CEA |
Electrocardiogram
- To view the electrocardiogram findings on COVID-19, click here.
- There are no ECG findings associated with COVID-19-associated meningitis
X-ray
- There are no x-ray findings associated with COVID-19-associated meningitis.
- To view the x-ray finidings on COVID-19, click here.
Echocardiography or Ultrasound
- There are no echocardiography/ultrasound findings associated with COVID-19-associated meningitis.
- To view the echocardiographic findings on COVID-19, click here.
CT scan
- CT scan of the brain may detect brain inflammation.
- To view the CT scan findings on COVID-19, click here.
MRI
- MRI of brain may show hyperintense areas due to brain inflammation.
- To view other imaging findings on COVID-19, click here.
Other Imaging Findings
- There are no other imaging findings associated with COVID-19 associated meningitis.
Other Diagnostic Studies
- There are no other diagnostic studies associated with COVID-19 associated meningitis.
Treatment
Medical Therapy
The mainstays of medical therapy for viral meningitis are:[29][30][31][32][33][34][35]
Symptomatic treatments:
- Anti-inflammatory drugs like steroids are helpful to decrease brain inflammation in COVID-19 associated meningitis.
- Corticosteroids (methylprednisolone 300 mg/day) in severe COVID-19 patients are shown to reduce mortality.
- If a COVID-19 patient with meningitis develops seizures anti-epileptic drugs like levetiracetam (50-60 mg/kg/day) may be necessary..
- Tocilizumab (8mg/kg/dose) is IL-6 anatgonist, that reduces cytokine storm syndrome responsible for neurological manifestations in a COVID-19 patient.
- Intubation and mechanical ventilation may be needed .
- To see treatment protocol to manage the underlying cause i.e., COVID-19, click here.
Surgery
- In case of brain parenchyma involvement surgery can be done [33].
Primary Prevention
- There are no established measures for the primary prevention of COVID-19 associated meningitis.
- To view primary prevention for COVID-19 click here.
Secondary Prevention
- There are no established measures for the secondary prevention of COVID-19 associated meningitis.
- To view secondary prevention for COVID-19 click here.
References
- ↑ Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J; et al. (2020). "A first case of meningitis/encephalitis associated with SARS-Coronavirus-2". Int J Infect Dis. 94: 55–58. doi:10.1016/j.ijid.2020.03.062. PMC 7195378 Check
|pmc=value (help). PMID 32251791 Check|pmid=value (help). - ↑ Duong L, Xu P, Liu A (2020). "Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in Downtown Los Angeles, early April 2020". Brain Behav Immun. 87: 33. doi:10.1016/j.bbi.2020.04.024. PMC 7162766 Check
|pmc=value (help). PMID 32305574 Check|pmid=value (help). - ↑ Bernard-Valnet R, Pizzarotti B, Anichini A, Demars Y, Russo E, Schmidhauser M; et al. (2020). "Two patients with acute meningoencephalitis concomitant with SARS-CoV-2 infection". Eur J Neurol. doi:10.1111/ene.14298. PMC 7267660 Check
|pmc=value (help). PMID 32383343 Check|pmid=value (help). - ↑ Tsai LK, Hsieh ST, Chang YC (2005). "Neurological manifestations in severe acute respiratory syndrome". Acta Neurol Taiwan. 14 (3): 113–9. PMID 16252612.
- ↑ Schoeman D, Fielding BC (2019). "Coronavirus envelope protein: current knowledge". Virol J. 16 (1): 69. doi:10.1186/s12985-019-1182-0. PMC 6537279 Check
|pmc=value (help). PMID 31133031. - ↑ Lu R, Zhao X, Li J, Niu P, Yang B, Wu H; et al. (2020). "Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding". Lancet. 395 (10224): 565–574. doi:10.1016/S0140-6736(20)30251-8. PMC 7159086 Check
|pmc=value (help). PMID 32007145 Check|pmid=value (help). - ↑ Baig AM, Khaleeq A, Ali U, Syeda H (2020). "Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms". ACS Chem Neurosci. 11 (7): 995–998. doi:10.1021/acschemneuro.0c00122. PMC 7094171 Check
|pmc=value (help). PMID 32167747 Check|pmid=value (help). - ↑ Ge XY, Li JL, Yang XL, Chmura AA, Zhu G, Epstein JH; et al. (2013). "Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor". Nature. 503 (7477): 535–8. doi:10.1038/nature12711. PMC 5389864. PMID 24172901.
- ↑ Turner AJ, Hiscox JA, Hooper NM (2004). "ACE2: from vasopeptidase to SARS virus receptor". Trends Pharmacol Sci. 25 (6): 291–4. doi:10.1016/j.tips.2004.04.001. PMC 7119032 Check
|pmc=value (help). PMID 15165741. - ↑ Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O; et al. (2020). "Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation". Science. 367 (6483): 1260–1263. doi:10.1126/science.abb2507. PMC 7164637 Check
|pmc=value (help). PMID 32075877 Check|pmid=value (help). - ↑ Baig AM, Khaleeq A, Ali U, Syeda H (2020). "Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms". ACS Chem Neurosci. 11 (7): 995–998. doi:10.1021/acschemneuro.0c00122. PMC 7094171 Check
|pmc=value (help). PMID 32167747 Check|pmid=value (help). - ↑ Swanson PA, McGavern DB (2015). "Viral diseases of the central nervous system". Curr Opin Virol. 11: 44–54. doi:10.1016/j.coviro.2014.12.009. PMC 4456224. PMID 25681709.
- ↑ Wong SH, Lui RN, Sung JJ (2020). "Covid-19 and the digestive system". J Gastroenterol Hepatol. 35 (5): 744–748. doi:10.1111/jgh.15047. PMID 32215956 Check
|pmid=value (help). - ↑ Alenquer M, Amorim MJ (2015). "Exosome Biogenesis, Regulation, and Function in Viral Infection". Viruses. 7 (9): 5066–83. doi:10.3390/v7092862. PMC 4584306. PMID 26393640.
- ↑ Tsivgoulis G, Palaiodimou L, Katsanos AH, Caso V, Köhrmann M, Molina C, Cordonnier C, Fischer U, Kelly P, Sharma VK, Chan AC, Zand R, Sarraj A, Schellinger PD, Voumvourakis KI, Grigoriadis N, Alexandrov AV, Tsiodras S (2020). "Neurological manifestations and implications of COVID-19 pandemic". Ther Adv Neurol Disord. 13: 1756286420932036. doi:10.1177/1756286420932036. PMC 7284455 Check
|pmc=value (help). PMID 32565914 Check|pmid=value (help). - ↑ Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J; et al. (2020). "A first case of meningitis/encephalitis associated with SARS-Coronavirus-2". Int J Infect Dis. 94: 55–58. doi:10.1016/j.ijid.2020.03.062. PMC 7195378 Check
|pmc=value (help). PMID 32251791 Check|pmid=value (help). - ↑ Bernard-Valnet R, Pizzarotti B, Anichini A, Demars Y, Russo E, Schmidhauser M; et al. (2020). "Two patients with acute meningoencephalitis concomitant with SARS-CoV-2 infection". Eur J Neurol. doi:10.1111/ene.14298. PMC 7267660 Check
|pmc=value (help). PMID 32383343 Check|pmid=value (help). - ↑ Bernard-Valnet R, Pizzarotti B, Anichini A, Demars Y, Russo E, Schmidhauser M; et al. (2020). "Two patients with acute meningoencephalitis concomitant with SARS-CoV-2 infection". Eur J Neurol. doi:10.1111/ene.14298. PMC 7267660 Check
|pmc=value (help). PMID 32383343 Check|pmid=value (help). - ↑ Chaumont H, Etienne P, Roze E, Couratier C, Roger PM, Lannuzel A (2020). "Acute meningoencephalitis in a patient with COVID-19". Rev Neurol (Paris). 176 (6): 519–521. doi:10.1016/j.neurol.2020.04.014. PMC 7211749 Check
|pmc=value (help). PMID 32414534 Check|pmid=value (help). - ↑ Duong L, Xu P, Liu A (2020). "Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in Downtown Los Angeles, early April 2020". Brain Behav Immun. 87: 33. doi:10.1016/j.bbi.2020.04.024. PMC 7162766 Check
|pmc=value (help). PMID 32305574 Check|pmid=value (help). - ↑ 21.0 21.1 Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM, Whitley RJ (November 2004). "Practice guidelines for the management of bacterial meningitis". Clin. Infect. Dis. 39 (9): 1267–84. doi:10.1086/425368. PMID 15494903.
- ↑ Chaudhuri A, Martinez-Martin P, Martin PM, Kennedy PG, Andrew Seaton R, Portegies P, Bojar M, Steiner I (July 2008). "EFNS guideline on the management of community-acquired bacterial meningitis: report of an EFNS Task Force on acute bacterial meningitis in older children and adults". Eur. J. Neurol. 15 (7): 649–59. doi:10.1111/j.1468-1331.2008.02193.x. PMID 18582342.
- ↑ 23.0 23.1 Le Rhun E, Taillibert S, Chamberlain MC (2013). "Carcinomatous meningitis: Leptomeningeal metastases in solid tumors". Surg Neurol Int. 4 (Suppl 4): S265–88. doi:10.4103/2152-7806.111304. PMC 3656567. PMID 23717798.
- ↑ 24.0 24.1 Chow E, Troy SB (2014). "The differential diagnosis of hypoglycorrhachia in adult patients". Am J Med Sci. 348 (3): 186–90. doi:10.1097/MAJ.0000000000000217. PMC 4065645. PMID 24326618.
- ↑ 25.0 25.1 Leen WG, Willemsen MA, Wevers RA, Verbeek MM (2012). "Cerebrospinal fluid glucose and lactate: age-specific reference values and implications for clinical practice". PLoS One. 7 (8): e42745. doi:10.1371/journal.pone.0042745. PMC 3412827. PMID 22880096.
- ↑ 26.0 26.1 26.2 Negrini B, Kelleher KJ, Wald ER (2000). "Cerebrospinal fluid findings in aseptic versus bacterial meningitis". Pediatrics. 105 (2): 316–9. PMID 10654948.
- ↑ Brouwer MC, Tunkel AR, van de Beek D (2010). "Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis". Clin Microbiol Rev. 23 (3): 467–92. doi:10.1128/CMR.00070-09. PMC 2901656. PMID 20610819.
- ↑ Caudie C, Tholance Y, Quadrio I, Peysson S (2010). "[Contribution of CSF analysis to diagnosis and follow-up of tuberculous meningitis]". Ann Biol Clin (Paris). 68 (1): 107–11. doi:10.1684/abc.2010.0407. PMID 20146981.
- ↑ Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J; et al. (2020). "A first case of meningitis/encephalitis associated with SARS-Coronavirus-2". Int J Infect Dis. 94: 55–58. doi:10.1016/j.ijid.2020.03.062. PMC 7195378 Check
|pmc=value (help). PMID 32251791 Check|pmid=value (help). - ↑ Russell CD, Millar JE, Baillie JK (February 2020). "Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury". Lancet. 395 (10223): 473–475. doi:10.1016/S0140-6736(20)30317-2. PMC 7134694 Check
|pmc=value (help). PMID 32043983 Check|pmid=value (help). - ↑ Russell B, Moss C, George G, Santaolalla A, Cope A, Papa S; et al. (2020). "Associations between immune-suppressive and stimulating drugs and novel COVID-19-a systematic review of current evidence". Ecancermedicalscience. 14: 1022. doi:10.3332/ecancer.2020.1022. PMC 7105343 Check
|pmc=value (help). PMID 32256705 Check|pmid=value (help). - ↑ Ueda R, Saito Y, Ohno K, Maruta K, Matsunami K, Saiki Y, Sokota T, Sugihara S, Nishimura Y, Tamasaki A, Narita A, Imamura A, Maegaki Y (May 2015). "Effect of levetiracetam in acute encephalitis with refractory, repetitive partial seizures during acute and chronic phase". Brain Dev. 37 (5): 471–7. doi:10.1016/j.braindev.2014.08.003. PMID 25174548.
- ↑ 33.0 33.1 Efe IE, Aydin OU, Alabulut A, Celik O, Aydin K (2020). "COVID-19-Associated Encephalitis Mimicking Glial Tumor". World Neurosurg. 140: 46–48. doi:10.1016/j.wneu.2020.05.194. PMC 7256557 Check
|pmc=value (help). PMID 32479911 Check|pmid=value (help). - ↑ [+https://clinicaltrials.gov/ct2/show/NCT04372186 "A Study to Evaluate the Efficacy and Safety of Tocilizumab in Hospitalized Participants With COVID-19 Pneumonia - Full Text View - ClinicalTrials.gov"] Check
|url=value (help). - ↑ Zhang C, Wu Z, Li JW, Zhao H, Wang GQ (2020). "Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality". Int J Antimicrob Agents. 55 (5): 105954. doi:10.1016/j.ijantimicag.2020.105954. PMC 7118634 Check
|pmc=value (help). PMID 32234467 Check|pmid=value (help).