Splenic vein thrombosis pathophysiology: Difference between revisions
| (4 intermediate revisions by 3 users not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}} ; {{AE}} {{Vbe}} | {{CMG}} ; {{AE}} {{Vbe}} | ||
==Overview== | ==Overview== | ||
Splenic vein thrombosis in acute or chronic [[pancreatitis]] results from peri-venous [[inflammation]] caused by the anatomic location of the [[splenic vein]] along the entire posterior aspect of the pancreatic tail, where it lies in direct contact with the peri-pancreatic [[Inflammatory|inflammator]]<nowiki/>y | |||
the [[splenic vein]] along the entire posterior aspect of the pancreatic tail, where it lies in direct contact with the | tissue. The exact mechanism of [[thrombosis]] is likely multi factorial, including both intrinsic endothelial damage from [[inflammatory]] | ||
tissue. The exact mechanism of [[thrombosis]] is likely multi factorial, including both intrinsic endothelial damage from inflammatory | or [[neoplastic]] processes and extrinsic damage secondary to venous compression from fibrosis, adjacent [[Pseudocyst|pseudocysts]] or [[edema]]. | ||
or neoplastic processes and extrinsic damage secondary to venous compression from fibrosis, adjacent | |||
== Structure== | == Structure== | ||
The [[splenic vein]] is a blood vessel that drains blood from the [[spleen]], the stomach fundus and part of the pancreas. It is part of the [[Hepatic portal system|hepatic portal]] system. It follows a course superior to the pancreas, alongside the splenic artery. It collects branches from the stomach and pancreas, and most notably from the [[large intestine]] (also drained by the superior mesenteric vein) via the [[inferior mesenteric vein]], which drains in the [[splenic vein]] shortly before the origin of the [[hepatic portal vein]]. The [[portal vein]] is formed when the [[splenic vein]] joins the superior mesenteric vein. | Following are important facts regarding vasculature of splenic venous system: | ||
* The [[splenic vein]] is a blood vessel that drains blood from the [[spleen]], the stomach fundus and part of the pancreas. | |||
* It is part of the [[Hepatic portal system|hepatic portal]] system. | |||
* It follows a course superior to the pancreas, alongside the splenic artery. | |||
* It collects branches from the stomach and pancreas, and most notably from the [[large intestine]] (also drained by the [[superior mesenteric vein]]) via the [[inferior mesenteric vein]], which drains in the [[splenic vein]] shortly before the origin of the [[hepatic portal vein]]. | |||
* The [[portal vein]] is formed when the [[splenic vein]] joins the [[superior mesenteric vein]]. | |||
== Pathophysiology== | == Pathophysiology== | ||
===Pathogenesis=== | ===Pathogenesis=== | ||
It is thought that splenic vein thrombosis is caused by [[Virchow's triad]] which includes:<ref name="pmid25941431">{{cite journal |vauthors=Chawla YK, Bodh V |title=Portal vein thrombosis |journal=J Clin Exp Hepatol |volume=5 |issue=1 |pages=22–40 |year=2015 |pmid=25941431 |pmc=4415192 |doi=10.1016/j.jceh.2014.12.008 |url=}}</ref> | |||
*Reduced portal blood flow | |||
*[[Hypercoagulable state]] | |||
*Vascular [[endothelial]] injury | |||
<figure-inline>[[File:VTE Pathophysisology Virchow's triad.JPG|639x639px]]</figure-inline> | <figure-inline><figure-inline><figure-inline><figure-inline><figure-inline>[[File:VTE Pathophysisology Virchow's triad.JPG|639x639px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> | ||
Shown below is a table depicting the elements of Virchow's triad and their modern counterparts. | Shown below is a table depicting the elements of Virchow's triad and their modern counterparts. | ||
| Line 31: | Line 35: | ||
| style="background:#DCDCDC;" align="center" + |"Stasis" or "[[venous stasis]]"<ref name="pmid15692260">{{cite journal |author=Lowe GD |title=Virchow's triad revisited: abnormal flow |journal=Pathophysiol. Haemost. Thromb. |volume=33 |issue=5-6 |pages=455–7 |year=2003 |pmid=15692260 |doi=10.1159/000083845 |url=http://content.karger.com/produktedb/produkte.asp?doi=10.1159/000083845&typ=pdf}}</ref> | | style="background:#DCDCDC;" align="center" + |"Stasis" or "[[venous stasis]]"<ref name="pmid15692260">{{cite journal |author=Lowe GD |title=Virchow's triad revisited: abnormal flow |journal=Pathophysiol. Haemost. Thromb. |volume=33 |issue=5-6 |pages=455–7 |year=2003 |pmid=15692260 |doi=10.1159/000083845 |url=http://content.karger.com/produktedb/produkte.asp?doi=10.1159/000083845&typ=pdf}}</ref> | ||
| style="background:#F5F5F5;" + | | | style="background:#F5F5F5;" + | | ||
* The first category | * The first category includes alterations in normal [[blood]] flow in several situations. | ||
* These include [[turbulence]], [[stasis (medicine)|stasis]], [[mitral stenosis]], and [[varicose veins]]. | * These include [[turbulence]], [[stasis (medicine)|stasis]], [[mitral stenosis]], and [[varicose veins]]. | ||
* The equivalence of [[Virchow's triad|Virchow's]] version and the modern version has been disputed.<ref name="urlFurther reflections on Virchows triad. - Free Online Library">{{cite web |url=http://www.thefreelibrary.com/Further+reflections+on+Virchow%27s+triad.(Letter+to+the+Editor)-a0128075135 |title=Further reflections on Virchow's triad. - Free Online Library |format= |work= |accessdate=2009-02-10}}</ref> | * The equivalence of [[Virchow's triad|Virchow's]] version and the modern version has been disputed.<ref name="urlFurther reflections on Virchows triad. - Free Online Library">{{cite web |url=http://www.thefreelibrary.com/Further+reflections+on+Virchow%27s+triad.(Letter+to+the+Editor)-a0128075135 |title=Further reflections on Virchow's triad. - Free Online Library |format= |work= |accessdate=2009-02-10}}</ref> | ||
| Line 38: | Line 42: | ||
| style="background:#DCDCDC;" align="center" + |"Endothelial injury" or "vessel wall injury" | | style="background:#DCDCDC;" align="center" + |"Endothelial injury" or "vessel wall injury" | ||
| style="background:#F5F5F5;" + | | | style="background:#F5F5F5;" + | | ||
* The second category | * The second category includes injuries and/or [[trauma]] to [[endothelium]], damage to the veins arising from [[shear stress]] or [[hypertension]]. | ||
|- | |- | ||
! style="background:#DCDCDC;" align="center" + |Phenomena of [[blood]]-[[coagulation]] | ! style="background:#DCDCDC;" align="center" + |Phenomena of [[blood]]-[[coagulation]] | ||
| style="background:#DCDCDC;" align="center" + |"[[Hypercoagulability]]" | | style="background:#DCDCDC;" align="center" + |"[[Hypercoagulability]]" | ||
| style="background:#F5F5F5;" + | | | style="background:#F5F5F5;" + | | ||
* The last category | * The last category includes alterations in the constitution of blood,<ref name="pmid15692259">{{cite journal |author=Chung I, Lip GY |title=Virchow's triad revisited: blood constituents |journal=Pathophysiol. Haemost. Thromb. |volume=33 |issue=5-6 |pages=449–54 |year=2003 |pmid=15692259 |doi=10.1159/000083844 |url=http://content.karger.com/produktedb/produkte.asp?doi=10.1159/000083844&typ=pdf}}</ref> has numerous possible [[risk factors]] such as [[hyperviscosity]], deficiency of [[antithrombin]] III, [[nephrotic syndrome]], changes after severe [[Physical trauma|trauma]] or burn, disseminated [[cancer]], late [[pregnancy]], and [[delivery]], race, age, whether the patient is a smoker or [[obesity|obese]]. | ||
* All of these [[risk factors]] lead to [[hypercoagulability]]. | * All of these [[risk factors]] lead to [[hypercoagulability]]. | ||
|} | |} | ||
Mechanism of development of splenic vein thrombosis: | |||
* | *Splenic vein thrombosis in acute or chronic [[pancreatitis]] results from acute inflammation. | ||
*The pathophysiology of thrombosis is likely [[Multi factorial inheritance|multi factorial]] | *The pathophysiology of thrombosis is likely [[Multi factorial inheritance|multi factorial]]. | ||
* Endothelial damage from [[inflammatory]] or neoplastic process is also one of the mechanism reported | * Endothelial damage from [[inflammatory]] or neoplastic process is also one of the mechanism reported. | ||
* Another mechanism known to cause thrombosis is [[Extrinsic allergic alveolitis|extrinsic]] damage secondary to [[venous]] [[Compression bandage|compression]] from [[fibrosis]], adjacent | * Another mechanism known to cause thrombosis is [[Extrinsic allergic alveolitis|extrinsic]] damage secondary to [[venous]] [[Compression bandage|compression]] from [[fibrosis]], adjacent pseudocysts, or [[edema]]. | ||
*Obstruction of the splenic vein caused by enlarged | *Obstruction of the splenic vein caused by enlarged retroperitoneal [[lymph nodes]] or by [[pancreatic]] or peri-splenic nodes which are located near the splenic artery,above the splenic vein. | ||
*These nodes lie adjacent to the [[pancreas]] and [[splenic vein]] and compress the splenic vein when involved in an [[inflammatory]] or [[neoplastic]] process. | *These nodes lie adjacent to the [[pancreas]] and [[splenic vein]] and compress the splenic vein when involved in an [[inflammatory]] or [[neoplastic]] process. | ||
*When [[thrombosis]] of the [[splenic vein]] occurs, collateral vessels develop to shunt blood around the occluded splenic vein. The two most common collateral pathways use the [[short gastric]] vessels. | *When [[thrombosis]] of the [[splenic vein]] occurs, collateral vessels develop to shunt blood around the occluded splenic vein. The two most common collateral pathways use the [[short gastric]] vessels. | ||
* In the distal [[esophagus]], portosystemic collaterals connect the [[short gastric veins]] into the [[Azygous continuation of the inferior vena cava|azygous]] system. | * In the distal [[esophagus]], portosystemic collaterals connect the [[short gastric veins]] into the [[Azygous continuation of the inferior vena cava|azygous]] system. Spleno-portal collaterals decompress the short gastric veins through both the coronary vein into the portal vein and via the [[Gastroepiploic artery|gastroepiploic]] arcade into the [[superior mesenteric vein]]. In either case, the [[Hypertensive Emergencies|hypertensive]] short gastric veins cause increased pressure within the submucosal veins of the gastric fundus, resulting in varices. | ||
the gastric fundus, resulting in varices. | |||
*At times, an enlarged gastroepiploic vein found at laparotomy may be the only indicator of occult splenic vein thrombosis. Isolated esophageal varices, although uncommon in SVT, can occur in cases in which the coronary vein joins the splenic vein proximal to the obstruction. This anatomic variant has been reported to occur in 17 % of the cases. | *At times, an enlarged gastroepiploic vein found at laparotomy may be the only indicator of occult splenic vein thrombosis. Isolated esophageal varices, although uncommon in SVT, can occur in cases in which the coronary vein joins the splenic vein proximal to the obstruction. This anatomic variant has been reported to occur in 17 % of the cases. | ||
| Line 64: | Line 68: | ||
==Genetics== | ==Genetics== | ||
The exact [[genetics]] of [[splenic vein thrombosis]] is not fully understood | The exact [[genetics]] of [[splenic vein thrombosis]] is not fully understood. | ||
==Associated conditions== | ==Associated conditions== | ||
Latest revision as of 15:54, 1 March 2018
|
Splenic vein thrombosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Splenic vein thrombosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Splenic vein thrombosis pathophysiology |
|
Risk calculators and risk factors for Splenic vein thrombosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Vindhya BellamKonda, M.B.B.S [2]
Overview
Splenic vein thrombosis in acute or chronic pancreatitis results from peri-venous inflammation caused by the anatomic location of the splenic vein along the entire posterior aspect of the pancreatic tail, where it lies in direct contact with the peri-pancreatic inflammatory tissue. The exact mechanism of thrombosis is likely multi factorial, including both intrinsic endothelial damage from inflammatory or neoplastic processes and extrinsic damage secondary to venous compression from fibrosis, adjacent pseudocysts or edema.
Structure
Following are important facts regarding vasculature of splenic venous system:
- The splenic vein is a blood vessel that drains blood from the spleen, the stomach fundus and part of the pancreas.
- It is part of the hepatic portal system.
- It follows a course superior to the pancreas, alongside the splenic artery.
- It collects branches from the stomach and pancreas, and most notably from the large intestine (also drained by the superior mesenteric vein) via the inferior mesenteric vein, which drains in the splenic vein shortly before the origin of the hepatic portal vein.
- The portal vein is formed when the splenic vein joins the superior mesenteric vein.
Pathophysiology
Pathogenesis
It is thought that splenic vein thrombosis is caused by Virchow's triad which includes:[1]
- Reduced portal blood flow
- Hypercoagulable state
- Vascular endothelial injury
<figure-inline><figure-inline><figure-inline><figure-inline><figure-inline>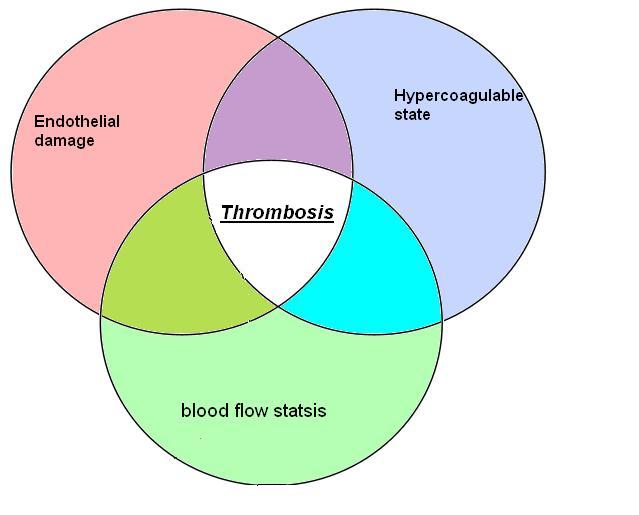
Shown below is a table depicting the elements of Virchow's triad and their modern counterparts.
| Virchow's[2] | Modern | Notes |
|---|---|---|
| Phenomena of interrupted blood-flow | "Stasis" or "venous stasis"[3] |
|
| Phenomena associated with irritation of the vessel and its vicinity | "Endothelial injury" or "vessel wall injury" |
|
| Phenomena of blood-coagulation | "Hypercoagulability" |
|
Mechanism of development of splenic vein thrombosis:
- Splenic vein thrombosis in acute or chronic pancreatitis results from acute inflammation.
- The pathophysiology of thrombosis is likely multi factorial.
- Endothelial damage from inflammatory or neoplastic process is also one of the mechanism reported.
- Another mechanism known to cause thrombosis is extrinsic damage secondary to venous compression from fibrosis, adjacent pseudocysts, or edema.
- Obstruction of the splenic vein caused by enlarged retroperitoneal lymph nodes or by pancreatic or peri-splenic nodes which are located near the splenic artery,above the splenic vein.
- These nodes lie adjacent to the pancreas and splenic vein and compress the splenic vein when involved in an inflammatory or neoplastic process.
- When thrombosis of the splenic vein occurs, collateral vessels develop to shunt blood around the occluded splenic vein. The two most common collateral pathways use the short gastric vessels.
- In the distal esophagus, portosystemic collaterals connect the short gastric veins into the azygous system. Spleno-portal collaterals decompress the short gastric veins through both the coronary vein into the portal vein and via the gastroepiploic arcade into the superior mesenteric vein. In either case, the hypertensive short gastric veins cause increased pressure within the submucosal veins of the gastric fundus, resulting in varices.
- At times, an enlarged gastroepiploic vein found at laparotomy may be the only indicator of occult splenic vein thrombosis. Isolated esophageal varices, although uncommon in SVT, can occur in cases in which the coronary vein joins the splenic vein proximal to the obstruction. This anatomic variant has been reported to occur in 17 % of the cases.
- Less common collateral pathways may also develop to decompress the splenic vein. The left gastroepiploic vein can collateralize to the left colic and inferior mesenteric veins. Although rare, this development has been reported to result in colonic variceal hemorrhage. Other collateral venous channels may develop via the diaphragmatic and intercostal veins to the inferior vena cava .The splenic vein may also collateralize to the renal vein via the adrenal vein.
Genetics
The exact genetics of splenic vein thrombosis is not fully understood.
Associated conditions
The conditions associated with splenic vein thrombosis include:
- Pancreatitis
- Genetic disorders such as Factor V Leiden mutations
- Thrombophilias
- Abdominal trauma
Gross pathology
- There is no finding on gross pathology of Splenic vein thrombosis.
Microscopic pathology
- There is no finding on microscopic histopathological analysis.
References
- ↑ Chawla YK, Bodh V (2015). "Portal vein thrombosis". J Clin Exp Hepatol. 5 (1): 22–40. doi:10.1016/j.jceh.2014.12.008. PMC 4415192. PMID 25941431.
- ↑ Agutter, Paul S. (2008). The Aetiology of Deep Venous Thrombosis: A Critical, Historical and Epistemological Survey. Berlin: Springer. p. 84. ISBN 1-4020-6649-X.
- ↑ Lowe GD (2003). "Virchow's triad revisited: abnormal flow". Pathophysiol. Haemost. Thromb. 33 (5–6): 455–7. doi:10.1159/000083845. PMID 15692260.
- ↑ "Further reflections on Virchow's triad. - Free Online Library". Retrieved 2009-02-10.
- ↑ Chung I, Lip GY (2003). "Virchow's triad revisited: blood constituents". Pathophysiol. Haemost. Thromb. 33 (5–6): 449–54. doi:10.1159/000083844. PMID 15692259.