Tuberculosis chest x ray: Difference between revisions
Mashal Awais (talk | contribs) No edit summary |
Mohamed riad (talk | contribs) |
||
| (18 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Tuberculosis}} | {{Tuberculosis}} | ||
{{CMG}}; {{AE}} {{AL}} | {{CMG}}; {{AE}} {{Mashal Awais}}; {{AL}} | ||
==Overview== | ==Overview== | ||
[[X-rays|X-ray]] is a main diagnostic method for [[pulmonary tuberculosis]]. [[Chest X-ray]] may show [[Parenchymal lung disease|parenchymal]] [[infiltrates]], hilar [[adenopathy]], cavitation, [[nodules]] and [[pleural effusion]]. [[Tuberculosis|Pulmonary tuberculosis]] is often present in the upper [[Lobe (anatomy)|lobes]]. | |||
==Chest X-Ray== | ==Chest X-Ray== | ||
An | An anteroposterior [[chest X-ray]] is one of the main imaging tests to be done in a patient with [[tuberculosis]] or suspected [[Tuberculosis, pulmonary|tuberculosis]].<ref>{{Cite journal | ||
| author = [[Riccardo Piccazzo]], [[Francesco Paparo]] & [[Giacomo Garlaschi]] | | author = [[Riccardo Piccazzo]], [[Francesco Paparo]] & [[Giacomo Garlaschi]] | ||
| title = Diagnostic accuracy of chest radiography for the diagnosis of tuberculosis (TB) and its role in the detection of latent TB infection: a systematic review | | title = Diagnostic accuracy of chest radiography for the diagnosis of tuberculosis (TB) and its role in the detection of latent TB infection: a systematic review | ||
| Line 20: | Line 20: | ||
===Primary Tuberculosis=== | ===Primary Tuberculosis=== | ||
*The 3 | |||
*Primary tuberculosis may | *The 3 major findings on chest X-ray are [[Parenchyma|parenchymal]] infiltrates, hilar [[adenopathy]], and [[pleural effusion]]. | ||
* | *Primary [[tuberculosis]] may affect any part in the [[lung]]. | ||
*Less than | *Children often present with hilar [[lymphadenopathy]] on [[chest X-ray]], which can be present in up to 95% of children with active [[tuberculosis]]. | ||
*Tuberculomas | *Less than 50% of adults with primary [[tuberculosis]] present with hilar [[lymphadenopathy]]. <ref name="CardinaleParlatano2014">{{cite journal|last1=Cardinale|first1=L.|last2=Parlatano|first2=D.|last3=Boccuzzi|first3=F.|last4=Onoscuri|first4=M.|last5=Volpicelli|first5=G.|last6=Veltri|first6=A.|title=The imaging spectrum of pulmonary tuberculosis|journal=Acta Radiologica|year=2014|issn=0284-1851|doi=10.1177/0284185114533247}}</ref> | ||
* Unilateral [[pleural effusion]] | *[[Tuberculomas]] ([[opacities]] similar to a [[lung mass]]) can be seen in 5% of patients and can reach 4 cm in size.<ref name="KimSong2001">{{cite journal|last1=Kim|first1=Hyae Young|last2=Song|first2=Koun-Sik|last3=Goo|first3=Jin Mo|last4=Lee|first4=Jin Seong|last5=Lee|first5=Kyoung Soo|last6=Lim|first6=Tae-Hwan|title=Thoracic Sequelae and Complications of Tuberculosis1|journal=RadioGraphics|volume=21|issue=4|year=2001|pages=839–858|issn=0271-5333|doi=10.1148/radiographics.21.4.g01jl06839}}</ref><ref name="pmid3484866">{{cite journal| author=Woodring JH, Vandiviere HM, Fried AM, Dillon ML, Williams TD, Melvin IG| title=Update: the radiographic features of pulmonary tuberculosis. | journal=AJR Am J Roentgenol | year= 1986 | volume= 146 | issue= 3 | pages= 497-506 | pmid=3484866 | doi=10.2214/ajr.146.3.497 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3484866 }} </ref> | ||
*Unilateral [[pleural effusion]] can be seen as a [[Complication (medicine)|complication]] of primary [[tuberculosis]]. | |||
===Secondary Tuberculosis=== | ===Secondary Tuberculosis=== | ||
* | |||
*The X-ray findings in secondary or | *Secondary [[tuberculosis]] usually targets the [[upper lobes]], particularly the [[apical]] and [[posterior]] segments. However, [[lesions]] can be present anywhere in the [[lungs]]. | ||
:*Patchy consolidation | *The [[X-ray]] findings in secondary or r[[eactivated tuberculosis]] include:<ref name="CardinaleParlatano2014">{{cite journal|last1=Cardinale|first1=L.|last2=Parlatano|first2=D.|last3=Boccuzzi|first3=F.|last4=Onoscuri|first4=M.|last5=Volpicelli|first5=G.|last6=Veltri|first6=A.|title=The imaging spectrum of pulmonary tuberculosis|journal=Acta Radiologica|year=2014|issn=0284-1851|doi=10.1177/0284185114533247}}</ref> | ||
:*[[Cavitation]], | |||
::* | :*Patchy [[Consolidation (medicine)|consolidation]] is poorly defined. | ||
:*[[Cavitation]], that is the most commonly observed finding in secondary [[tuberculosis]] | |||
::*It has thick walls and [[irregular]] [[margins]]. | |||
::*It may be observed in almost 50% of patients. | ::*It may be observed in almost 50% of patients. | ||
::* | ::*Usually located in the upper [[lung]]. | ||
::*Cavities in the lower lung can be found in [[diabetes]] and [[HIV]] infection.<ref name="PatelRami2011">{{cite journal|last1=Patel|first1=AnandK|last2=Rami|first2=KiranC|last3=Ghanchi|first3=FerozD|title=Radiological presentation of patients of pulmonary tuberculosis with diabetes mellitus|journal=Lung India|volume=28|issue=1|year=2011|pages=70|issn=0970-2113|doi=10.4103/0970-2113.76308}}</ref><ref name="PadyanaBhat2012">{{cite journal|last1=Padyana|first1=Mahesha|last2=Bhat|first2=RaghavendraV|last3=Dinesha|first3=M|last4=Nawaz|first4=Alam|title=HIV-Tuberculosis: A Study of Chest X-Ray Patterns in Relation to CD4 Count|journal=North American Journal of Medical Sciences|volume=4|issue=5|year=2012|pages=221|issn=1947-2714|doi=10.4103/1947-2714.95904}}</ref> | ::*[[Cavities]] in the lower lung can be found in [[diabetes]] and [[HIV]] infection.<ref name="PatelRami2011">{{cite journal|last1=Patel|first1=AnandK|last2=Rami|first2=KiranC|last3=Ghanchi|first3=FerozD|title=Radiological presentation of patients of pulmonary tuberculosis with diabetes mellitus|journal=Lung India|volume=28|issue=1|year=2011|pages=70|issn=0970-2113|doi=10.4103/0970-2113.76308}}</ref><ref name="PadyanaBhat2012">{{cite journal|last1=Padyana|first1=Mahesha|last2=Bhat|first2=RaghavendraV|last3=Dinesha|first3=M|last4=Nawaz|first4=Alam|title=HIV-Tuberculosis: A Study of Chest X-Ray Patterns in Relation to CD4 Count|journal=North American Journal of Medical Sciences|volume=4|issue=5|year=2012|pages=221|issn=1947-2714|doi=10.4103/1947-2714.95904}}</ref> | ||
::* | ::*Despite being rare, [[superinfected|superinfection]] of the [[cavities]] may occur and an [[air-fluid]] level is seen inside the [[cavity]]. | ||
:*[[Pneumothorax]] is rare but may be seen in 5% of patients. | :*[[Pneumothorax]] is rare but may be seen in 5% of patients. | ||
:*[[Lymphadenopathy]] is also uncommon in secondary tuberculosis. | :*[[Lymphadenopathy]] is also uncommon in secondary tuberculosis. | ||
:*Small [[pleural effusion]] may occur in 18% of patients. | :*Small [[pleural effusion]] may occur in 18% of patients. | ||
*In the majority of cases the consolidation involves more than one lobe.<ref name="BurrillWilliams2007">{{cite journal|last1=Burrill|first1=Joshua|last2=Williams|first2=Christopher J.|last3=Bain|first3=Gillian|last4=Conder|first4=Gabriel|last5=Hine|first5=Andrew L.|last6=Misra|first6=Rakesh R.|title=Tuberculosis: A Radiologic Review1|journal=RadioGraphics|volume=27|issue=5|year=2007|pages=1255–1273|issn=0271-5333|doi=10.1148/rg.275065176}}</ref> | *In the majority of cases the consolidation involves more than one lobe.<ref name="BurrillWilliams2007">{{cite journal|last1=Burrill|first1=Joshua|last2=Williams|first2=Christopher J.|last3=Bain|first3=Gillian|last4=Conder|first4=Gabriel|last5=Hine|first5=Andrew L.|last6=Misra|first6=Rakesh R.|title=Tuberculosis: A Radiologic Review1|journal=RadioGraphics|volume=27|issue=5|year=2007|pages=1255–1273|issn=0271-5333|doi=10.1148/rg.275065176}}</ref> | ||
=====Chest X-Ray Images in Pulmonary Tuberculosis===== | =====Chest X-Ray Images in Pulmonary Tuberculosis===== | ||
<gallery> | <gallery> | ||
File:Pulmonary Tuberculosis X-ray.jpg|Pulmonary Tuberculosis | |||
File:Pulmonary Tuberculosis X-ray2.jpg|Pulmonary Tuberculosis | |||
File:Pulmonary Tuberculosis X-ray3.jpg|Pulmonary Tuberculosis | |||
File:Pulmonary Tuberculosis X-ray4.jpg|Bilateral Pulmonary Tuberculosis | |||
File:TB CXR.jpg|Pulmonary Tuberculosis | |||
</gallery> | </gallery> | ||
===Common Findings of Miliary Tuberculosis on Chest X-Ray=== | ===Common Findings of Miliary Tuberculosis on Chest X-Ray=== | ||
* Fine, | |||
* Commonly found throughout both lungs. | *Fine, pinpoint approximately 1-2mm in size, discrete, uniform distribution, soft mottlings. | ||
*Commonly found throughout both lungs. | |||
{{further|'''[[Miliary tuberculosis chest x ray|Miliary tuberculosis]]'''}} | {{further|'''[[Miliary tuberculosis chest x ray|Miliary tuberculosis]]'''}} | ||
=====Chest X-Ray Images in Miliary Tuberculosis===== | =====Chest X-Ray Images in Miliary Tuberculosis===== | ||
<gallery> | <gallery> | ||
File:Miliary Tuberculosis.jpg|Miliary Tuberculosis | |||
File:Disseminated-TB-001.jpg|Miliary Tuberculosis | |||
File:Disseminated-TB-002.jpg|Miliary Tuberculosis | |||
</gallery> | </gallery> | ||
==CDC Guidelines for Evaluating Chest X-Ray<small><small><ref name="CDC"> {{cite web| url=http://www.cdc.gov/immigrantrefugeehealth/exams/medical-examination.html| title= CDC Medical Examination of Immigrants and Refugees}}</ref></small></small>== | ==CDC Guidelines for Evaluating Chest X-Ray<small><small><ref name="CDC"> {{cite web| url=http://www.cdc.gov/immigrantrefugeehealth/exams/medical-examination.html| title= CDC Medical Examination of Immigrants and Refugees}}</ref></small></small>== | ||
A medical examination is | A medical examination is obligatory for all refugees traveling to the U.S. and all applicants outside the U.S. applying for an immigrant visa. The aim of the medical examination is to detect applicants with inadmissible health-related conditions such as active tuberculosis. Outside the U.S., medical examinations are done by about 400 physicians (panel physicians) who are selected by United States Department of State consular officials. In the U.S., medical examinations are done by about 3,000 physicians (civil surgeons) selected by district directors of the U.S. Citizenship and Immigration Services. [[Centers for Disease Control and Prevention]] (CDC) has been responsible for establishing the guidelines. | ||
The [[chest X-ray]] and classification | The [[chest X-ray]] and classification system is structured to collect findings into categories according to their probability of being related to TB or non-TB conditions requiring medical follow-up. | ||
===Abnormal Findings=== | ===Abnormal Findings=== | ||
| Line 72: | Line 77: | ||
====Chest X-Ray Findings that Can Suggest Active TB==== | ====Chest X-Ray Findings that Can Suggest Active TB==== | ||
This category | This category consists of all findings typically associated with active [[pulmonary]] [[TB]]. An applicant with any of the following findings must perform an examination of [[sputum]] specimens. | ||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 700px" align=center | {| style="border: 0px; font-size: 90%; margin: 3px; width: 700px" align="center" | ||
|valign=top| | | valign="top" | | ||
|+ | |+ | ||
! style="background: #4479BA; width: 225px;" | {{fontcolor|#FFF|Chest X-ray Findings}} | ! style="background: #4479BA; width: 225px;" |{{fontcolor|#FFF|Chest X-ray Findings}} | ||
! style="background: #4479BA; width: 475px;" | {{fontcolor|#FFF|Description}} | ! style="background: #4479BA; width: 475px;" |{{fontcolor|#FFF|Description}} | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Infiltrate or consolidation | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Infiltrate or consolidation | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" |Opacificaties within the [[lung]] [[parenchyma]]. Consolidation or infiltrate may be dense or patchy and has irregular, ill-defined, or hazy borders. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Any cavitary lesion | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Any cavitary lesion | ||
| style="padding: 5px 5px; background: #F5F5F5;" | Lucency (darkened area) within the lung parenchyma, with or without irregular margins that | | style="padding: 5px 5px; background: #F5F5F5;" |Lucency (darkened area) within the lung parenchyma, with or without irregular margins that may be surrounded by an area of airspace consolidation or infiltrates, or by [[nodular]] or fibrotic (reticular) densities, or both. The walls around the lucent area may be thick or thin. Calcification may also exist surrounding a [[cavity]]. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Nodule with poorly defined margins | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Nodule with poorly defined margins | ||
| style="padding: 5px 5px; background: #F5F5F5;" | Round density within the lung parenchyma, also | | style="padding: 5px 5px; background: #F5F5F5;" |Round density within the [[lung]] [[parenchyma]], also known as a [[tuberculoma]]. Nodules included in this category are those with margins that are poorly defined. The surrounding haziness may be either subtle or readily obvious and indicates coexisting airspace consolidation. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Pleural effusion | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Pleural effusion | ||
| style="padding: 5px 5px; background: #F5F5F5;" | Presence of a | | style="padding: 5px 5px; background: #F5F5F5;" |Presence of a high amount of fluid within the [[pleural]] space. This finding must be differentiated from blunting of the [[costophrenic angle]], which may or may not represent a small amount of fluid within the pleural space (except in children when even minor blunting of the [[costophrenic angle]] is considered a finding suggestive of active [[TB]]). | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Hilar or mediastinal lymphadenopathy ([[bihilar lymphadenopathy]]) | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Hilar or mediastinal [[lymphadenopathy]] ([[bihilar lymphadenopathy]]) | ||
| style="padding: 5px 5px; background: #F5F5F5;" | Enlargement of lymph nodes in one or both hila or within the [[mediastinum]], with or without associated atelectasis | | style="padding: 5px 5px; background: #F5F5F5;" |Enlargement of lymph nodes in one or both hila or within the [[mediastinum]], with or without associated consolidation or [[atelectasis]]. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Linear, interstitial disease (in children only) | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Linear, interstitial disease (in children only) | ||
| style="padding: 5px 5px; background: #F5F5F5;" | Prominence of linear, interstitial (septal) markings. | | style="padding: 5px 5px; background: #F5F5F5;" |Prominence of linear, interstitial (septal) markings. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Other | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Other | ||
| style="padding: 5px 5px; background: #F5F5F5;" | Any other finding | | style="padding: 5px 5px; background: #F5F5F5;" |Any other finding indicating active [[TB]], such as [[miliary TB]]. Miliary findings are nodules of millet size (1 to 2 millimeters) distributed throughout the parenchyma. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | colspan="2" style="padding: 5px 5px; background: #F5F5F5;" |<small> Adpated from CDC<ref name="CDC"> {{cite web| url=http://www.cdc.gov/immigrantrefugeehealth/exams/medical-examination.html| title= CDC Medical Examination of Immigrants and Refugees}}</ref> </small> | ||
|} | |} | ||
====Chest X-Ray Findings that Can Suggest Inactive TB==== | ====Chest X-Ray Findings that Can Suggest Inactive TB==== | ||
These findings can be suggestive of prior [[Tuberculosis|TB]], that is [[inactive]]. It is not possible to diagnose [[active TB]] based on only a single [[Radiography|radiograph]]. If a [[diagnosis]] active [[Tuberculosis|TB]] is in doubt, [[sputum]] [[smears]] examination must be performed. Additionally, if there are any [[signs]] or [[symptoms]] of TB, examination of [[sputum]] smears must be performed then. Consequently, any applicant may have findings grouped in this category, but still have active TB as suggested by: | |||
*The | |||
*[[Sputum]] smears positive for AFB ([[Tuberculosis classification#CDC TB Classification for Immigrants and Refugees|Class A]]). | *The [[signs]] or [[symptoms]] of [[TB]] ([[Tuberculosis classification#CDC TB Classification for Immigrants and Refugees|Class B1]]). | ||
*[[Sputum]] smears positive for [[AFB stain|AFB]] ([[Tuberculosis classification#CDC TB Classification for Immigrants and Refugees|Class A]]). | |||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 700px" align=center | {| style="border: 0px; font-size: 90%; margin: 3px; width: 700px" align="center" | ||
|valign=top| | | valign="top" | | ||
|+ | |+ | ||
! style="background: #4479BA; width: 225px;" | {{fontcolor|#FFF|Chest X-ray Findings}} | ! style="background: #4479BA; width: 225px;" |{{fontcolor|#FFF|Chest X-ray Findings}} | ||
! style="background: #4479BA; width: 475px;" | {{fontcolor|#FFF|Description}} | ! style="background: #4479BA; width: 475px;" |{{fontcolor|#FFF|Description}} | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Discrete fibrotic scar or linear opacity | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Discrete fibrotic scar or linear opacity | ||
| style="padding: 5px 5px; background: #F5F5F5;" |Discrete | | style="padding: 5px 5px; background: #F5F5F5;" |Discrete [[reticular]] densities within the [[lung]] with distinct edges and without suggestion of airspace opacification or haziness between or around the densities. [[Calcification]] may be seen within the lesion and then the it is called a fibrocalcific [[scar]]. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Discrete nodule(s) without calcification | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Discrete nodule(s) without calcification | ||
| style="padding: 5px 5px; background: #F5F5F5;" |One or | | style="padding: 5px 5px; background: #F5F5F5;" |One or multiple [[nodular]] densities with distinct borders and without any surrounding airspace opacification. Nodules are generally round or have rounded edges. These characteristics allow them to be differentiated from infiltrates or airspace opacities. These [[nodules]] must be noncalcified to be included in this category. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Discrete fibrotic scar with volume loss or retraction | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Discrete fibrotic [[scar]] with volume loss or [[retraction]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" |Discrete linear densities with reduction in the space occupied by the upper lobe. | | style="padding: 5px 5px; background: #F5F5F5;" |Discrete linear densities with reduction in the space occupied by the upper lobe. Usually upward deviation of the [[hilum]] on the corresponding side with asymmetry of the volumes of the two [[thoracic]] [[cavities]] are present as associated [[signs]]. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Discrete nodule(s) with volume loss or retraction | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Discrete nodule(s) with volume loss or retraction | ||
| style="padding: 5px 5px; background: #F5F5F5;" |One or | | style="padding: 5px 5px; background: #F5F5F5;" |One or multiple [[nodular]] densities with distinct borders and no surrounding airspace opacification with reduction in the space occupied by the upper [[lobe]]. [[Nodules]] are mainly rounded. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Other | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Other | ||
| style="padding: 5px 5px; background: #F5F5F5;" |Any other finding | | style="padding: 5px 5px; background: #F5F5F5;" |Any other finding indicating previous [[TB]], such as upper lobe [[bronchiectasis]]. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | colspan="2" style="padding: 5px 5px; background: #F5F5F5;" |<small> Adpated from CDC<ref name="CDC"> {{cite web| url=http://www.cdc.gov/immigrantrefugeehealth/exams/medical-examination.html| title= CDC Medical Examination of Immigrants and Refugees}}</ref> </small> | ||
|} | |} | ||
===Other Chest X-Ray Findings=== | ===Other Chest X-Ray Findings=== | ||
====Follow-up==== | ====Follow-up==== | ||
This category includes findings that | This category includes findings that require a follow-up evaluation for non-TB conditions either at the time of the [[chest X-ray]] or after resettlement of the applicant in the U.S. | ||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 700px" align=center | {| style="border: 0px; font-size: 90%; margin: 3px; width: 700px" align="center" | ||
|valign=top| | | valign="top" | | ||
|+ | |+ | ||
! style="background: #4479BA; width: 225px;" | {{fontcolor|#FFF|Chest X-ray Findings}} | ! style="background: #4479BA; width: 225px;" |{{fontcolor|#FFF|Chest X-ray Findings}} | ||
! style="background: #4479BA; width: 475px;" | {{fontcolor|#FFF|Description}} | ! style="background: #4479BA; width: 475px;" |{{fontcolor|#FFF|Description}} | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Musculoskeletal abnormalities | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Musculoskeletal abnormalities | ||
| style="padding: 5px 5px; background: #F5F5F5;" |New bony fractures or | | style="padding: 5px 5px; background: #F5F5F5;" |New bony fractures or bony abnormalities present on radiographs that require follow-up. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Cardiac abnormalities | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Cardiac abnormalities | ||
| style="padding: 5px 5px; background: #F5F5F5;" |Cardiac | | style="padding: 5px 5px; background: #F5F5F5;" |Cardiac or vascular abnormalities, or any other cardiovascular abnormality of significant nature present on radiographs to require follow-up. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Pulmonary abnormalities | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Pulmonary abnormalities | ||
| style="padding: 5px 5px; background: #F5F5F5;" |Pulmonary finding of | | style="padding: 5px 5px; background: #F5F5F5;" |Pulmonary finding that is not suggestive of [[TB]], such as a mass, that requires follow-up. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Other | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Other | ||
| style="padding: 5px 5px; background: #F5F5F5;" |Any other finding that the panel physician believes needs follow-up, but is not one of the above. | | style="padding: 5px 5px; background: #F5F5F5;" |Any other finding that the panel physician believes needs follow-up, but is not one of the above. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | colspan="2" style="padding: 5px 5px; background: #F5F5F5;" |<small> Adpated from CDC<ref name="CDC"> {{cite web| url=http://www.cdc.gov/immigrantrefugeehealth/exams/medical-examination.html| title= CDC Medical Examination of Immigrants and Refugees}}</ref> </small> | ||
|} | |} | ||
====Follow-up Not Required==== | ====Follow-up Not Required==== | ||
This | This includes findings that are minor and do not suggest TB disease. This does not need follow-up evaluation after the applicant resettlement. | ||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 700px" align=center | {| style="border: 0px; font-size: 90%; margin: 3px; width: 700px" align="center" | ||
|valign=top| | | valign="top" | | ||
|+ | |+ | ||
! style="background: #4479BA; width: 225px;" | {{fontcolor|#FFF|Chest X-ray Findings}} | ! style="background: #4479BA; width: 225px;" |{{fontcolor|#FFF|Chest X-ray Findings}} | ||
! style="background: #4479BA; width: 475px;" | {{fontcolor|#FFF|Description}} | ! style="background: #4479BA; width: 475px;" |{{fontcolor|#FFF|Description}} | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Pleural thickening | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Pleural thickening | ||
| style="padding: 5px 5px; background: #F5F5F5;" |Irregularity | | style="padding: 5px 5px; background: #F5F5F5;" |Irregularity of the pleural margin, including apical capping (thickening of the [[pleura]] in the [[apical]] region). Pleural thickening may be calcified. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Diaphragmatic tenting | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Diaphragmatic tenting | ||
| Line 176: | Line 182: | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Blunting of [[costophrenic angle]] (in adults) | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Blunting of [[costophrenic angle]] (in adults) | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" |Blunting or loss of sharpness of one or both [[costophrenic angle]]s. Blunting can be related to a small amount of [[fluid]] in the pleural space or to [[pleural]] thickening and, by itself, is a non-specific finding (except in children, when even minor blunting is considered an indication of active TB). In contrast a large pleural effusion, or the presence of a significant amount of fluid in the pleural space, may be a sign of active TB at any age. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Solitary calcified nodules or [[granuloma]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Solitary calcified nodules or [[granuloma]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" |Discrete calcified nodule or [[granuloma]], or calcified [[lymph node]]. The calcified nodule | | style="padding: 5px 5px; background: #F5F5F5;" |Discrete calcified nodule or [[granuloma]], or calcified [[lymph node]]. The calcified nodule may be present within the lung, hilium, or mediastinum. The borders must be sharp and well defined. Formerly, it was considered a [[Tuberculosis classification#CDC TB Classification for Immigrants and Refugees|Class B3]] TB; however, [[Tuberculosis classification#CDC TB Classification for Immigrants and Refugees|Class B3]] has been excluded from the classification scheme because it has not been reported to be associated with active TB. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | colspan="2" style="padding: 5px 5px; background: #F5F5F5;" |<small> Adpated from CDC<ref name="CDC"> {{cite web| url=http://www.cdc.gov/immigrantrefugeehealth/exams/medical-examination.html| title= CDC Medical Examination of Immigrants and Refugees}}</ref> </small> | ||
|} | |} | ||
==X-Ray Findings in Complications of Tuberculosis== | ==X-Ray Findings in Complications of Tuberculosis== | ||
{| style="border: 0px; font-size: 90%; margin: 3px; width:700px" align=center | {| style="border: 0px; font-size: 90%; margin: 3px; width:700px" align="center" | ||
|valign=top| | | valign="top" | | ||
|+ | |+ | ||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF|Complication}} | ! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF|Complication}} | ||
! style="background: #4479BA; width: 250px;" | {{fontcolor|#FFF|X-Ray Findings}} | ! style="background: #4479BA; width: 250px;" |{{fontcolor|#FFF|X-Ray Findings}} | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Cicatrization<ref name="pmid11452057">{{cite journal| author=Kim HY, Song KS, Goo JM, Lee JS, Lee KS, Lim TH| title=Thoracic sequelae and complications of tuberculosis. | journal=Radiographics | year= 2001 | volume= 21 | issue= 4 | pages= 839-58; discussion 859-60 | pmid=11452057 | doi=10.1148/radiographics.21.4.g01jl06839 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11452057 }} </ref> | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Cicatrization<ref name="pmid11452057">{{cite journal| author=Kim HY, Song KS, Goo JM, Lee JS, Lee KS, Lim TH| title=Thoracic sequelae and complications of tuberculosis. | journal=Radiographics | year= 2001 | volume= 21 | issue= 4 | pages= 839-58; discussion 859-60 | pmid=11452057 | doi=10.1148/radiographics.21.4.g01jl06839 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11452057 }} </ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Upper lobe [[atelectasis]] | *Upper lobe [[atelectasis]] | ||
| Line 202: | Line 208: | ||
*Traction [[bronchiectasis]] | *Traction [[bronchiectasis]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Thin-walled cavity | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Thin-walled cavity | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* Present in active and inactive | *Present in both active and inactive [[tuberculosis]] | ||
* May regress with treatment | *May regress with treatment | ||
* Air-filled [[cysts]] may persist<ref>{{cite book | last = Fraser | first = Richard | title = Synopsis of diseases of the chest | publisher = W.B. Saunders | location = Philadelphia | year = 1994 | isbn = 0721636691 }}</ref> | *Air-filled [[cysts]] may persist<ref>{{cite book | last = Fraser | first = Richard | title = Synopsis of diseases of the chest | publisher = W.B. Saunders | location = Philadelphia | year = 1994 | isbn = 0721636691 }}</ref> | ||
* Maybe misidentified as an [[Emphysema|emphysematous]] bulla or | *Maybe misidentified as an [[Emphysema|emphysematous]] bulla or pneumatocele. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | [[Aspergilloma]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Aspergilloma]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Mobile mass ringed by an air shadow. | *Mobile mass ringed by an air shadow. | ||
*Calcifications | *Calcifications | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Broncholithiasis<ref name="pmid2371439">{{cite journal| author=Galdermans D, Verhaert J, Van Meerbeeck J, de Backer W, Vermeire P| title=Broncholithiasis: present clinical spectrum. | journal=Respir Med | year= 1990 | volume= 84 | issue= 2 | pages= 155-6 | pmid=2371439 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2371439 }} </ref> | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Broncholithiasis<ref name="pmid2371439">{{cite journal| author=Galdermans D, Verhaert J, Van Meerbeeck J, de Backer W, Vermeire P| title=Broncholithiasis: present clinical spectrum. | journal=Respir Med | year= 1990 | volume= 84 | issue= 2 | pages= 155-6 | pmid=2371439 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2371439 }} </ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Calcified material within the tracheobronchial | *Calcified material within the [[lumen]] of the [[tracheobronchial]] tree, originated on a calcified [[lymph node]] | ||
*[[Airway]] obstruction | *[[Airway]] obstruction | ||
*[[Atelectasis]] | *[[Atelectasis]] | ||
| Line 232: | Line 238: | ||
*[[Atelectasis]] | *[[Atelectasis]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Tuberculous spondylitis ([[Pott's disease]]) | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Tuberculous]] [[spondylitis]] ([[Pott's disease]]) | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Vertebral endplate irregularities | *Vertebral endplate irregularities | ||
*Reduction of the intervertebral disk space | *Reduction of the intervertebral disk space | ||
*Adjacent bone sclerosis | *Adjacent bone sclerosis | ||
*In | *In advanced stages of the disease, [[kyphosis]] can occur as a result of anterior compression of the [[vertebral bodies]], and paravertebral [[abscess]]es. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Malignancy]]<ref name="pmid1987602">{{cite journal| author=Minami M, Kawauchi N, Yoshikawa K, Itai Y, Kokubo T, Iguchi M et al.| title=Malignancy associated with chronic empyema: radiologic assessment. | journal=Radiology | year= 1991 | volume= 178 | issue= 2 | pages= 417-23 | pmid=1987602 | doi=10.1148/radiology.178.2.1987602 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1987602 }} </ref> | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Malignancy]]<ref name="pmid1987602">{{cite journal| author=Minami M, Kawauchi N, Yoshikawa K, Itai Y, Kokubo T, Iguchi M et al.| title=Malignancy associated with chronic empyema: radiologic assessment. | journal=Radiology | year= 1991 | volume= 178 | issue= 2 | pages= 417-23 | pmid=1987602 | doi=10.1148/radiology.178.2.1987602 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1987602 }} </ref> | ||
| Line 244: | Line 250: | ||
*Increased [[thoracic cavity]] opacity | *Increased [[thoracic cavity]] opacity | ||
*Medial deviation of the affected [[pleura]] | *Medial deviation of the affected [[pleura]] | ||
*Swelling of the soft-tissue | *[[Swelling]] of the [[soft-tissue]] | ||
|} | |} | ||
| Line 253: | Line 259: | ||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Pulmonology]] | [[Category: Pulmonology]] | ||
[[Category:Bacterial diseases]] | [[Category:Bacterial diseases]] | ||
Latest revision as of 22:44, 26 March 2021
|
Tuberculosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tuberculosis chest x ray On the Web |
|
American Roentgen Ray Society Images of Tuberculosis chest x ray |
|
Risk calculators and risk factors for Tuberculosis chest x ray |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mashal Awais, M.D.[2]; Alejandro Lemor, M.D. [3]
Overview
X-ray is a main diagnostic method for pulmonary tuberculosis. Chest X-ray may show parenchymal infiltrates, hilar adenopathy, cavitation, nodules and pleural effusion. Pulmonary tuberculosis is often present in the upper lobes.
Chest X-Ray
An anteroposterior chest X-ray is one of the main imaging tests to be done in a patient with tuberculosis or suspected tuberculosis.[1]
Primary Tuberculosis
- The 3 major findings on chest X-ray are parenchymal infiltrates, hilar adenopathy, and pleural effusion.
- Primary tuberculosis may affect any part in the lung.
- Children often present with hilar lymphadenopathy on chest X-ray, which can be present in up to 95% of children with active tuberculosis.
- Less than 50% of adults with primary tuberculosis present with hilar lymphadenopathy. [2]
- Tuberculomas (opacities similar to a lung mass) can be seen in 5% of patients and can reach 4 cm in size.[3][4]
- Unilateral pleural effusion can be seen as a complication of primary tuberculosis.
Secondary Tuberculosis
- Secondary tuberculosis usually targets the upper lobes, particularly the apical and posterior segments. However, lesions can be present anywhere in the lungs.
- The X-ray findings in secondary or reactivated tuberculosis include:[2]
- Patchy consolidation is poorly defined.
- Cavitation, that is the most commonly observed finding in secondary tuberculosis
- It has thick walls and irregular margins.
- It may be observed in almost 50% of patients.
- Usually located in the upper lung.
- Cavities in the lower lung can be found in diabetes and HIV infection.[5][6]
- Despite being rare, superinfection of the cavities may occur and an air-fluid level is seen inside the cavity.
- Pneumothorax is rare but may be seen in 5% of patients.
- Lymphadenopathy is also uncommon in secondary tuberculosis.
- Small pleural effusion may occur in 18% of patients.
- In the majority of cases the consolidation involves more than one lobe.[7]
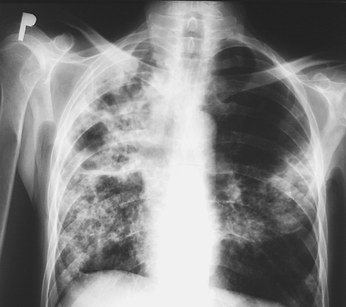
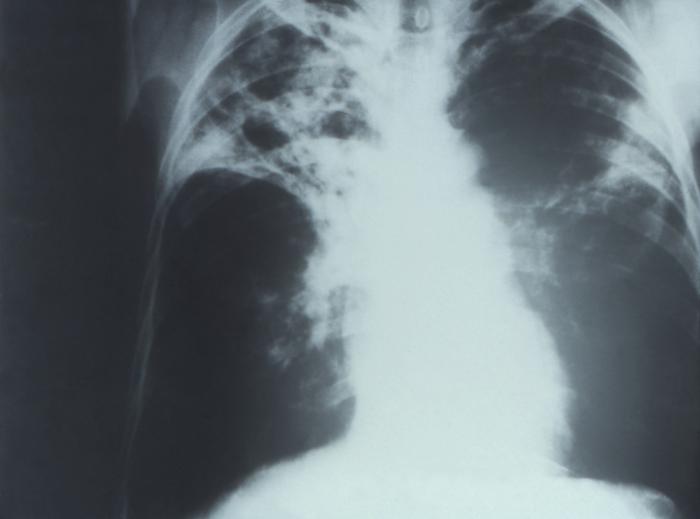
Chest X-Ray Images in Pulmonary Tuberculosis
-
Pulmonary Tuberculosis
-
Pulmonary Tuberculosis
-
Pulmonary Tuberculosis
-
Bilateral Pulmonary Tuberculosis
-
Pulmonary Tuberculosis
Common Findings of Miliary Tuberculosis on Chest X-Ray
- Fine, pinpoint approximately 1-2mm in size, discrete, uniform distribution, soft mottlings.
- Commonly found throughout both lungs.
Chest X-Ray Images in Miliary Tuberculosis
-
Miliary Tuberculosis
-
Miliary Tuberculosis
-
Miliary Tuberculosis
CDC Guidelines for Evaluating Chest X-Ray[8]
A medical examination is obligatory for all refugees traveling to the U.S. and all applicants outside the U.S. applying for an immigrant visa. The aim of the medical examination is to detect applicants with inadmissible health-related conditions such as active tuberculosis. Outside the U.S., medical examinations are done by about 400 physicians (panel physicians) who are selected by United States Department of State consular officials. In the U.S., medical examinations are done by about 3,000 physicians (civil surgeons) selected by district directors of the U.S. Citizenship and Immigration Services. Centers for Disease Control and Prevention (CDC) has been responsible for establishing the guidelines.
The chest X-ray and classification system is structured to collect findings into categories according to their probability of being related to TB or non-TB conditions requiring medical follow-up.
Abnormal Findings
Chest X-Ray Findings that Can Suggest Active TB
This category consists of all findings typically associated with active pulmonary TB. An applicant with any of the following findings must perform an examination of sputum specimens.
| Chest X-ray Findings | Description |
|---|---|
| Infiltrate or consolidation | Opacificaties within the lung parenchyma. Consolidation or infiltrate may be dense or patchy and has irregular, ill-defined, or hazy borders. |
| Any cavitary lesion | Lucency (darkened area) within the lung parenchyma, with or without irregular margins that may be surrounded by an area of airspace consolidation or infiltrates, or by nodular or fibrotic (reticular) densities, or both. The walls around the lucent area may be thick or thin. Calcification may also exist surrounding a cavity. |
| Nodule with poorly defined margins | Round density within the lung parenchyma, also known as a tuberculoma. Nodules included in this category are those with margins that are poorly defined. The surrounding haziness may be either subtle or readily obvious and indicates coexisting airspace consolidation. |
| Pleural effusion | Presence of a high amount of fluid within the pleural space. This finding must be differentiated from blunting of the costophrenic angle, which may or may not represent a small amount of fluid within the pleural space (except in children when even minor blunting of the costophrenic angle is considered a finding suggestive of active TB). |
| Hilar or mediastinal lymphadenopathy (bihilar lymphadenopathy) | Enlargement of lymph nodes in one or both hila or within the mediastinum, with or without associated consolidation or atelectasis. |
| Linear, interstitial disease (in children only) | Prominence of linear, interstitial (septal) markings. |
| Other | Any other finding indicating active TB, such as miliary TB. Miliary findings are nodules of millet size (1 to 2 millimeters) distributed throughout the parenchyma. |
| Adpated from CDC[8] | |
Chest X-Ray Findings that Can Suggest Inactive TB
These findings can be suggestive of prior TB, that is inactive. It is not possible to diagnose active TB based on only a single radiograph. If a diagnosis active TB is in doubt, sputum smears examination must be performed. Additionally, if there are any signs or symptoms of TB, examination of sputum smears must be performed then. Consequently, any applicant may have findings grouped in this category, but still have active TB as suggested by:
| Chest X-ray Findings | Description |
|---|---|
| Discrete fibrotic scar or linear opacity | Discrete reticular densities within the lung with distinct edges and without suggestion of airspace opacification or haziness between or around the densities. Calcification may be seen within the lesion and then the it is called a fibrocalcific scar. |
| Discrete nodule(s) without calcification | One or multiple nodular densities with distinct borders and without any surrounding airspace opacification. Nodules are generally round or have rounded edges. These characteristics allow them to be differentiated from infiltrates or airspace opacities. These nodules must be noncalcified to be included in this category. |
| Discrete fibrotic scar with volume loss or retraction | Discrete linear densities with reduction in the space occupied by the upper lobe. Usually upward deviation of the hilum on the corresponding side with asymmetry of the volumes of the two thoracic cavities are present as associated signs. |
| Discrete nodule(s) with volume loss or retraction | One or multiple nodular densities with distinct borders and no surrounding airspace opacification with reduction in the space occupied by the upper lobe. Nodules are mainly rounded. |
| Other | Any other finding indicating previous TB, such as upper lobe bronchiectasis. |
| Adpated from CDC[8] | |
Other Chest X-Ray Findings
Follow-up
This category includes findings that require a follow-up evaluation for non-TB conditions either at the time of the chest X-ray or after resettlement of the applicant in the U.S.
| Chest X-ray Findings | Description |
|---|---|
| Musculoskeletal abnormalities | New bony fractures or bony abnormalities present on radiographs that require follow-up. |
| Cardiac abnormalities | Cardiac or vascular abnormalities, or any other cardiovascular abnormality of significant nature present on radiographs to require follow-up. |
| Pulmonary abnormalities | Pulmonary finding that is not suggestive of TB, such as a mass, that requires follow-up. |
| Other | Any other finding that the panel physician believes needs follow-up, but is not one of the above. |
| Adpated from CDC[8] | |
Follow-up Not Required
This includes findings that are minor and do not suggest TB disease. This does not need follow-up evaluation after the applicant resettlement.
| Chest X-ray Findings | Description |
|---|---|
| Pleural thickening | Irregularity of the pleural margin, including apical capping (thickening of the pleura in the apical region). Pleural thickening may be calcified. |
| Diaphragmatic tenting | A localized accentuation of the normal convexity of the hemidiaphragm as if 'pulled upwards by a string'. |
| Blunting of costophrenic angle (in adults) | Blunting or loss of sharpness of one or both costophrenic angles. Blunting can be related to a small amount of fluid in the pleural space or to pleural thickening and, by itself, is a non-specific finding (except in children, when even minor blunting is considered an indication of active TB). In contrast a large pleural effusion, or the presence of a significant amount of fluid in the pleural space, may be a sign of active TB at any age. |
| Solitary calcified nodules or granuloma | Discrete calcified nodule or granuloma, or calcified lymph node. The calcified nodule may be present within the lung, hilium, or mediastinum. The borders must be sharp and well defined. Formerly, it was considered a Class B3 TB; however, Class B3 has been excluded from the classification scheme because it has not been reported to be associated with active TB. |
| Adpated from CDC[8] | |
X-Ray Findings in Complications of Tuberculosis
| Complication | X-Ray Findings |
|---|---|
| Cicatrization[9] |
|
| Thin-walled cavity |
|
| Aspergilloma |
|
| Broncholithiasis[11] |
|
| Fibrosing mediastinitis |
|
| Tuberculous spondylitis (Pott's disease) |
|
| Malignancy[12] |
|
References
- ↑ Riccardo Piccazzo, Francesco Paparo & Giacomo Garlaschi (2014). "Diagnostic accuracy of chest radiography for the diagnosis of tuberculosis (TB) and its role in the detection of latent TB infection: a systematic review". The Journal of rheumatology. Supplement. 91: 32–40. doi:10.3899/jrheum.140100. PMID 24788998. Unknown parameter
|month=ignored (help) - ↑ 2.0 2.1 Cardinale, L.; Parlatano, D.; Boccuzzi, F.; Onoscuri, M.; Volpicelli, G.; Veltri, A. (2014). "The imaging spectrum of pulmonary tuberculosis". Acta Radiologica. doi:10.1177/0284185114533247. ISSN 0284-1851.
- ↑ Kim, Hyae Young; Song, Koun-Sik; Goo, Jin Mo; Lee, Jin Seong; Lee, Kyoung Soo; Lim, Tae-Hwan (2001). "Thoracic Sequelae and Complications of Tuberculosis1". RadioGraphics. 21 (4): 839–858. doi:10.1148/radiographics.21.4.g01jl06839. ISSN 0271-5333.
- ↑ Woodring JH, Vandiviere HM, Fried AM, Dillon ML, Williams TD, Melvin IG (1986). "Update: the radiographic features of pulmonary tuberculosis". AJR Am J Roentgenol. 146 (3): 497–506. doi:10.2214/ajr.146.3.497. PMID 3484866.
- ↑ Patel, AnandK; Rami, KiranC; Ghanchi, FerozD (2011). "Radiological presentation of patients of pulmonary tuberculosis with diabetes mellitus". Lung India. 28 (1): 70. doi:10.4103/0970-2113.76308. ISSN 0970-2113.
- ↑ Padyana, Mahesha; Bhat, RaghavendraV; Dinesha, M; Nawaz, Alam (2012). "HIV-Tuberculosis: A Study of Chest X-Ray Patterns in Relation to CD4 Count". North American Journal of Medical Sciences. 4 (5): 221. doi:10.4103/1947-2714.95904. ISSN 1947-2714.
- ↑ Burrill, Joshua; Williams, Christopher J.; Bain, Gillian; Conder, Gabriel; Hine, Andrew L.; Misra, Rakesh R. (2007). "Tuberculosis: A Radiologic Review1". RadioGraphics. 27 (5): 1255–1273. doi:10.1148/rg.275065176. ISSN 0271-5333.
- ↑ 8.0 8.1 8.2 8.3 8.4 "CDC Medical Examination of Immigrants and Refugees".
- ↑ Kim HY, Song KS, Goo JM, Lee JS, Lee KS, Lim TH (2001). "Thoracic sequelae and complications of tuberculosis". Radiographics. 21 (4): 839–58, discussion 859-60. doi:10.1148/radiographics.21.4.g01jl06839. PMID 11452057.
- ↑ Fraser, Richard (1994). Synopsis of diseases of the chest. Philadelphia: W.B. Saunders. ISBN 0721636691.
- ↑ Galdermans D, Verhaert J, Van Meerbeeck J, de Backer W, Vermeire P (1990). "Broncholithiasis: present clinical spectrum". Respir Med. 84 (2): 155–6. PMID 2371439.
- ↑ Minami M, Kawauchi N, Yoshikawa K, Itai Y, Kokubo T, Iguchi M; et al. (1991). "Malignancy associated with chronic empyema: radiologic assessment". Radiology. 178 (2): 417–23. doi:10.1148/radiology.178.2.1987602. PMID 1987602.