Retinal detachment: Difference between revisions
Ahmed Younes (talk | contribs) No edit summary |
m Bot: Removing from Primary care |
||
| Line 149: | Line 149: | ||
{{Eye pathology}} | {{Eye pathology}} | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
| Line 167: | Line 161: | ||
[[sv:Näthinneavlossning]] | [[sv:Näthinneavlossning]] | ||
[[ta:விழித்திரை விலகல்]] | [[ta:விழித்திரை விலகல்]] | ||
[[Category:Ophthalmology]] | |||
[[Category:Emergency medicine]] | |||
Latest revision as of 23:58, 29 July 2020
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Retinal detachment is a disorder of the eye in which the retina peels away from its underlying layer of support tissue. Initial detachment may be localized, but without rapid treatment the entire retina may detach, leading to vision loss and blindness. It is a medical emergency. [1]
The retina is a thin layer of light-sensitive tissue on the back wall of the eye. The optical system of the eye focuses light on the retina much like light is focused on the film in a camera. The retina translates that focused image into neural impulses and sends them to the brain via the optic nerve. Occasionally, posterior vitreous detachment, injury or trauma to the eye or head may cause a small tear in the retina. The tear allows vitreous fluid to seep through it under the retina, and peel it away like a bubble in wallpaper.
Classification
- Rhegmatogenous retinal detachment - A rhegmatogenous retinal detachment occurs due to a hole, tear, or break in the retina that allows fluid to pass from the vitreous space into the subretinal space between the sensory retina and the retinal pigment epithelium.
- Exudative, serous, or secondary retinal detachment - An exudative retinal detachment occurs due to inflammation, injury or vascular abnormalities that results in fluid accumulating underneath the retina without the presence of a hole, tear, or break.
- Tractional retinal detachment - A tractional retinal detachment occurs when fibrovascular tissue, caused by an injury, inflammation or neovascularization, pulls the sensory retina from the retinal pigment epithelium.
Epidemiology and Demographics
Prevalence
The risk of retinal detachment in otherwise normal eyes is around 5 in 100,000 per year.[2] Detachment is more frequent in the middle-aged or elderly population with rates of around 20 in 100,000 per year.[3] The lifetime risk in normal eyes is about 1 in 300.[4]
- Retinal detachment is more common in those with severe or extreme myopia (above 5-6 diopters), as their eyes are longer and the retina is stretched thin. The lifetime risk increases to 1 in 20.[5] Myopia is associated with 67% of retinal detachment cases. Patients suffering from a detachment related to myopia tend to be younger than non-myopic detachment patients.
- Retinal detachment can occur more frequently after surgery for cataracts. The estimate of risk of retinal detachment after cataract surgery is 5 to 16 per 1000 cataract operations.[6] The risk may be much higher in those who are highly myopic, with a frequency of 7% reported in one study.[7] Young age at cataract removal further increased risk in this study. Long term risk of retinal detachment after extracapsular and phacoemulsification cataract surgery at 2, 5, and 10 years was estimated in one study to be 0.36%, 0.77%, and 1.29%, respectively.[8]
- Tractional retinal detachments can also occur in patients with proliferative diabetic retinopathy [9] or those with proliferative retinopathy of sickle cell disease.[10] In proliferative retinopathy, abnormal blood vessels (neovascularization) grow within the retina and extend into the vitreous. In advanced disease, the vessels can pull the retina away from the back wall of the eye causing a traction retinal detachment.
Although retinal detachment usually occurs in one eye, there is a 15% chance of developing it in the other eye, and this risk increases to 25-30% in patients who have had cataracts extracted from both eyes.[5]
Causes
- Drug side effect
Diagnosis
Symptoms
A retinal detachment is commonly preceded by a posterior vitreous detachment which gives rise to these symptoms:
- Flashes of light (photopsia) - very brief in the extreme peripheral (outside of center) part of vision
- A sudden dramatic increase in the number of floaters
- A ring of floaters or hairs just to the temporal side of the central vision
- A slight feeling of heaviness in the eye
Although most posterior vitreous detachments do not progress to retinal detachments, those that do produce the following symptoms:
- A dense shadow that starts in the peripheral vision and slowly progresses towards the central vision
- The impression that a veil or curtain was drawn over the field of vision
- Straight lines (scale, edge of the wall, road, etc.) that suddenly appear curved (positive Amsler grid test)
- Central visual loss
| Disease | Prominent clinical feature | Radiological findings |
|---|---|---|
| Ocular cysticercosis |
|
|
| Retinal detachment |
|
|
| Hyperthyroid Ophthalmopathy |
|
|
| Retinoblastoma |
|
|
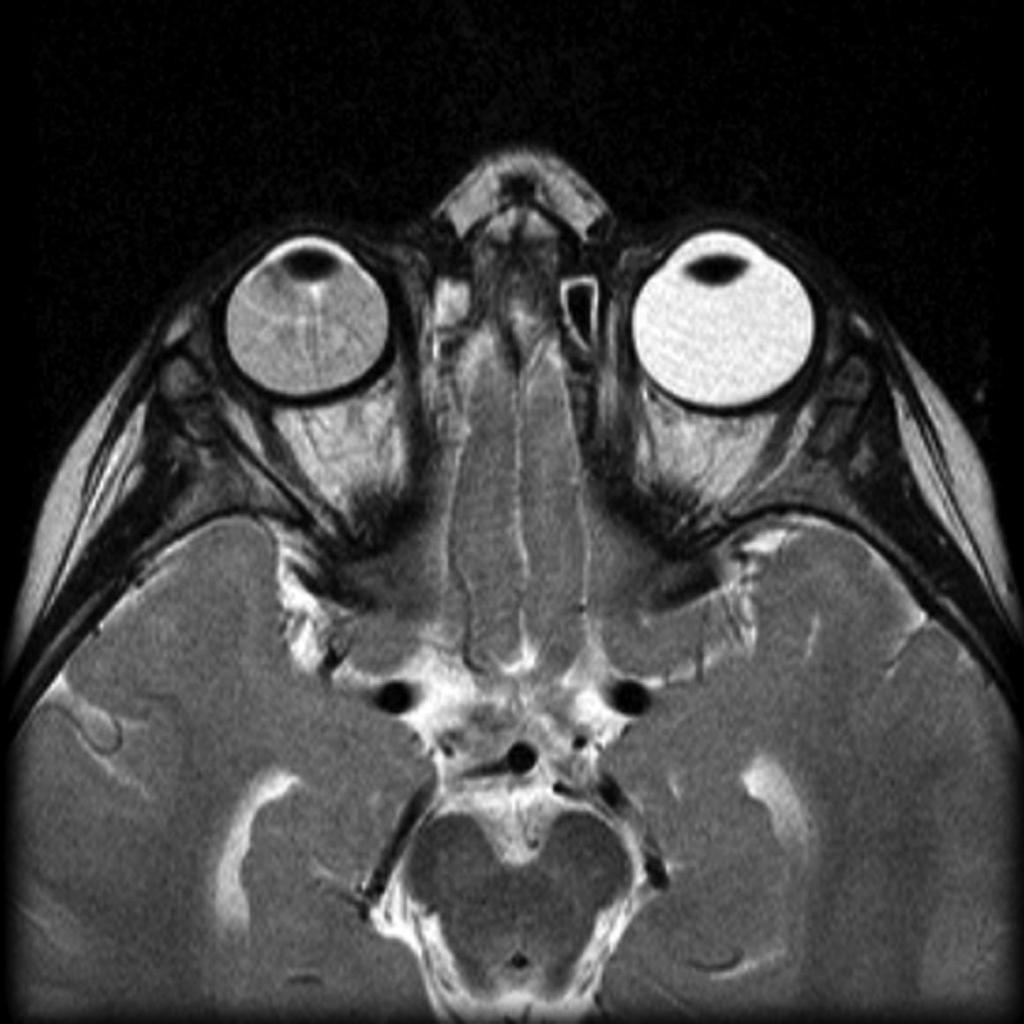 |
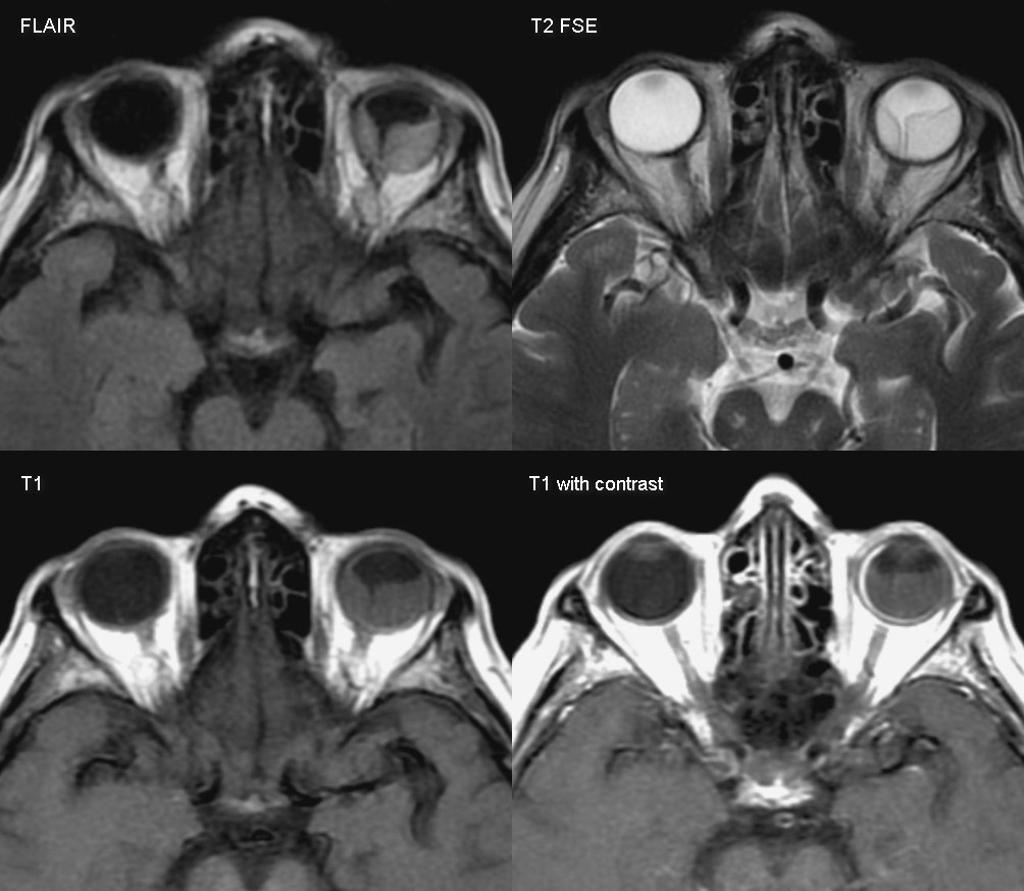 |
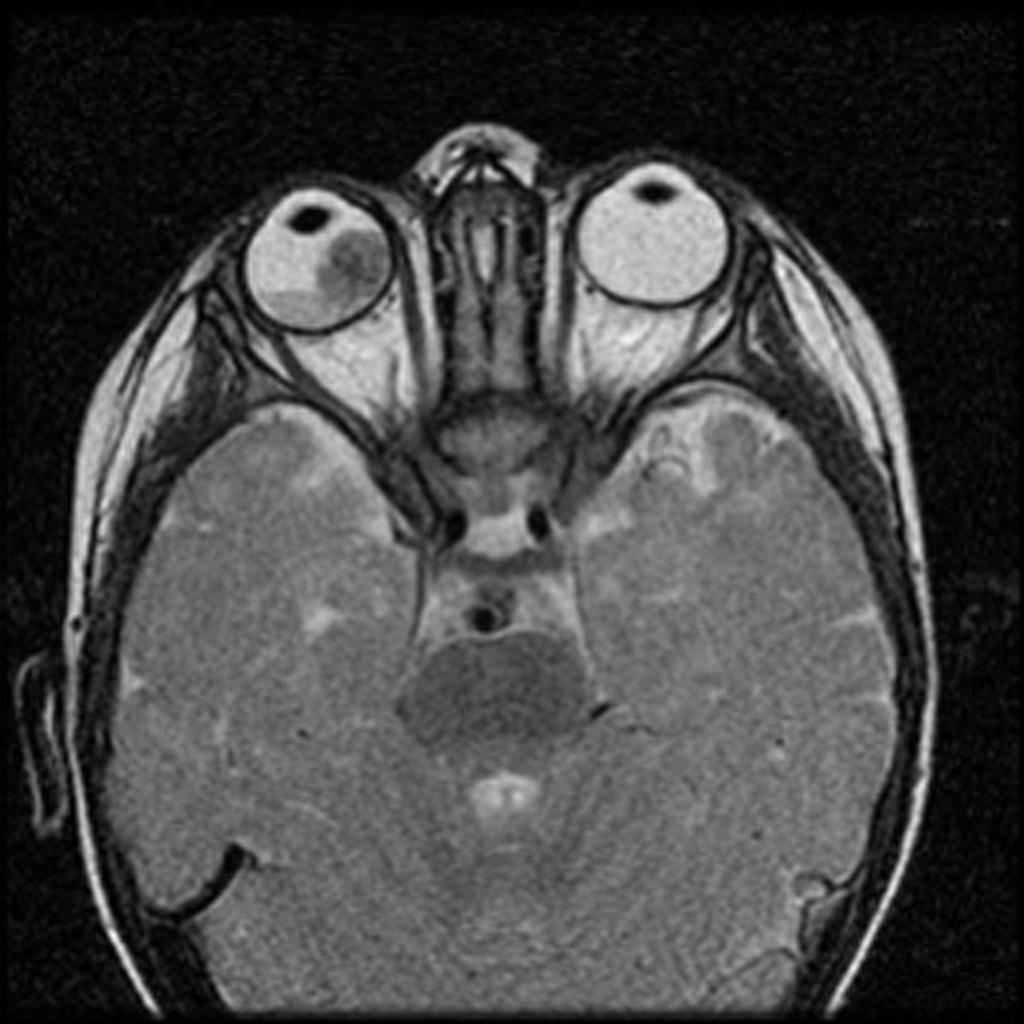 |
 |
|---|
Treatment
There are several methods of treating a detached retina which all depend on finding and closing the holes (tears) which have formed in the retina.
- Cryopexy and Laser Photocoagulation
- Cryotherapy (freezing) and laser photocoagulation are treatments used to create a scar/adhesion around the retinal hole to prevent fluid from entering the hole and accumulating behind the retina and exacerbating the retinal detachment. Cryopexy and photocoagulation are generally interchangeable. However, cryopexy is generally used in instances where there is a lot of fluid behind the hole; laser retinopexy will not take.
- Scleral buckle surgery
- Scleral buckle surgery is an established treatment in which the eye surgeon sews one or more silicone bands (bands, tyres) to the outside of the eyeball. The bands push the wall of the eye inward against the retinal hole, closing the hole and allowing the retina to re-attach. The bands do not usually have to be removed. The most common side effect of a scleral operation is myopic shift. That is, the operated eye will be more short sighted after the operation. Radial scleral buckle indicated to U-shaped tears or Fishmouth tears and posterior breaks. Circumferential scleral buckle indicated to multiple breaks, anterior breaks and wide breaks. Encircling buckles indicated to breaks more than 2 quadrant of retinal area, lattice degeration located on more than 2 quadrant of retinal area, undetecable breaks, proliferative vitreous retinopathy and inexperienced surgeon [15].
- Pneumatic retinopexy
- This operation is generally performed in the doctor's office under local anesthesia. It is another method of repairing a retinal detachment in which a gas bubble (SF6 or C3F8 gas) is injected into the eye after which laser or freezing treatment is applied to the retinal hole. The patient's head is then positioned so that the bubble rests against the retinal hole. Patients may have to keep their heads tilted for several days to keep the gas bubble in contact with the retinal hole. The surface tension of the air/water interface seals the hole in the retina, and allows the retinal pigment epithelium to pump the subretinal space dry and pull the retina back into place. This strict positioning requirement makes the treatment of the retinal holes and detachments that occurs in the lower part of the eyeball impractical. This procedure is usually combined with cryopexy or laser photocoagulation.
- Vitrectomy
- Vitrectomy is an increasingly used treatment for retinal detachment in countries with modern healthcare systems. It involves the removal of the vitreous gel and is usually combined with filling the eye with a gas bubble (SF6 or C3F8 gas). Advantages of this operation is that there is no myopic shift after the operation. A disadvantage is that a vitrectomy always leads to more rapid progression of a cataract in the operated eye. In many places vitrectomy is the most commonly performed operation for the treatment of retinal detachment.
- Ignipuncture
- Ignipuncture is an outdated procedure that involves cauterization of the retina with a very hot pointed instrument.[16] It was pioneered and named by Jules Gonin in the early 1900s.[16]
After treatment, patients gradually regain their vision over a period of a few weeks, although the visual acuity may not be as good as it was prior to the detachment, particularly if the macula was involved in the area of the detachment. However, if left untreated, total blindness could occur in a matter of days.
Prevention
Retinal detachment can be prevented in some. The most effective way of preventing retinal detachment is by educating people to seek ophthalmic medical attention if they suffer symptoms suggestive of a posterior vitreous detachment.[17] Early examination allows detection of retinal tears which can be treated with laser or cryotherapy. This reduces the risk of retinal detachment in those who have tears from around 1:3 to 1:20.
There are some known risk factors for retinal detachment. There are also many activities which at one time or another have been forbidden to those at risk of retinal detachment, with varying degrees of evidence supporting the restrictions.
Cataract surgery is a major cause, and can result in detachment even a long time after the operation. The risk is increased if there are complications during cataract surgery, but remains even in apparently uncomplicated surgery. The increasing rates of cataract surgery, and decreasing age at cataract surgery, inevitably lead to an increased incidence of retinal detachment.
Trauma is a less frequent cause. Activities which can cause direct trauma to the eye (boxing, kickboxing, karate, etc.) may cause a particular type of retinal tear called a retinal dialysis. This type of tear can be detected and treated before it develops into a retinal detachment. For this reason governing bodies in some of these sports require regular ophthalmic examination.
Individuals prone to retinal detachment due to a high level of myopia are encouraged to avoid activities where there is a risk of shock to the head or eyes, although without direct trauma to the eye the evidence base for this may be unconvincing.[5] Some doctors recommend avoiding activities that increase pressure in the eye, including diving, skydiving, again with little supporting evidence. According to one medical website, retinal detachment does not happen as a result of straining your eyes, bending or, heavy lifting.[18] Therefore, heavy weightlifting would appear to be fine. However, two recent scientific articles [19][20] have noted cases of retinal detachment or maculopathy due to weightlifting (specifically with the Valsalva method), and a third documented an increase in blood pressure in the eye during weightlifting [21].
Activities that involve sudden acceleration or deceleration also increase eye pressure and are discouraged by some doctors. These include bungee jumping[5] and may also include rollercoaster rides.
Related Chapters
External links
- Retinal Detachment Resource Guide from the National Eye Institute (NEI).
- Guidelines from the American Academy of Family Physicians
References
- ↑ "Retinal detachment". MedlinePlus Medical Encyclopedia. National Institutes of Health. 2005.
- ↑ Ivanisević M, Bojić L, Eterović D (2000). "Epidemiological study of nontraumatic phakic rhegmatogenous retinal detachment". Ophthalmic Res. 32 (5): 237–9. PMID 10971186.
- ↑ Li X (2003). "Incidence and epidemiological characteristics of rhegmatogenous retinal detachment in Beijing, China". Ophthalmology. 110 (12): 2413–7. PMID 14644727.
- ↑ "Evaluation and Management of Suspected Retinal Detachment - April 1, 2004 - American Family Physician".
- ↑ Jump up to: 5.0 5.1 5.2 5.3 "eMedicine - Retinal Detachment : Article by Gregory Luke Larkin, MD, MSPH, MSEng, FACEP".
- ↑ Ramos M, Kruger EF, Lashkari K (2002). "Biostatistical analysis of pseudophakic and aphakic retinal detachments". Seminars in ophthalmology. 17 (3–4): 206–13. PMID 12759852.
- ↑ Hyams SW, Bialik M, Neumann E (1975). "Myopia-aphakia. I. Prevalence of retinal detachment". The British journal of ophthalmology. 59 (9): 480–2. PMID 1203233.
- ↑ J.A. Rowe, J.C. Erie, K.H. Baratz; et al. (1999). "Retinal detachment in Olmsted County, Minnesota, 1976 through 1995". Ophthalmology. 106: 154–159. PMID 9917797.
- ↑ "Diabetic Retinopathy: Retinal Disorders: Merck Manual Home Edition".
- ↑ "IU Opt Online CE: Retinal Vascular Disease: Sickle Cell Retinopathy".
- ↑ Jump up to: 11.0 11.1 "How to Diagnose and Manage Coats' Disease".
- ↑ Jump up to: 12.0 12.1 "Management of retinal detachment: a guide for non-ophthalmologists".
- ↑ Jump up to: 13.0 13.1 "Thyroid Ophthalmopathy - EyeWiki".
- ↑ Jump up to: 14.0 14.1 "c.ymcdn.com".
- ↑ The principles of retinal detachment by Pardianto G et al., in Mimbar Ilmiah Oftalmologi Indonesia.2005;2: 63-4.
- ↑ Jump up to: 16.0 16.1 Wolfensberger TJ. "Jules Gonin. Pioneer of retinal detachment surgery." Indian J Ophthalmol. 2003 Dec;51(4):303-8. PMID 14750617.
- ↑ Byer NE (1994). "Natural history of posterior vitreous detachment with early management as the premier line of defense against retinal detachment". Ophthalmology. 101 (9): 1503–13, discussion 1513-4. PMID 8090453.
- ↑ "Understanding retinal detachment".
- ↑ Kocak N, Kaynak S, Kaynak T, Oner HF, Cingil G (2003). "Unilateral Purtscher-like retinopathy after weight-lifting". European journal of ophthalmology. 13 (4): 395–7. PMID 12872799.
- ↑ Chapman-Davies A, Lazarevic A (2002). "Valsalva maculopathy". Clinical & experimental optometry : journal of the Australian Optometrical Association. 85 (1): 42–5. PMID 11952395.
- ↑ Dickerman RD, Smith GH, Langham-Roof L, McConathy WJ, East JW, Smith AB (1999). "Intra-ocular pressure changes during maximal isometric contraction: does this reflect intra-cranial pressure or retinal venous pressure?". Neurol. Res. 21 (3): 243–6. PMID 10319330.
de:Netzhautablösung it:Distacco della retina no:Netthinneavløsning fi:Verkkokalvon irtauma sv:Näthinneavlossning ta:விழித்திரை விலகல்