Hamman-Rich syndrome pathophysiology: Difference between revisions
No edit summary |
|||
| (20 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Hamman-Rich syndrome}} | |||
{{CMG}}; {{AE}} | {{CMG}}; {{AE}} {{CK}} | ||
==Overview== | ==Overview== | ||
[[Hamman-Rich syndrome|Acute interstitial pneumonitis]] shows the [[Histopathology|histopathologic appearance]] of diffuse [[Alveolus|alveolar]] damage. On [[gross examination]], lungs appear firm, heavy and have a dark red or beefy appearance and show irregular areas of [[Consolidation (medicine)|consolidation]] and [[fibrosis]]. On [[Microscopy|microscopic examination]], [[Hamman-Rich syndrome|acute interstitial pneumonitis]] shows bilateral, temporal uniformity of the diffuse [[Alveolus|alveolar]] damage, hyaline membrane deposition and extensive [[Fibroblast|fibroblastic]] and [[Myofibroblast|myofibroblastic]] proliferation. | |||
[ | |||
[ | |||
==Pathophysiology== | ==Pathophysiology== | ||
===Pathogenesis=== | ===Pathogenesis=== | ||
*The | *The mechanism of initial [[injury]] to the pulmonary [[epithelium]] in [[Hamman-Rich syndrome|acute interstitial pneumonitis]] is not known. | ||
*Based on the findings of [[lung]] [[biopsy]], the uniformity and extent of the injury, it is assumed that a single insult triggers the pathologic process. | |||
* | *On microscopy, appearance of hyaline membrane remenats and organizing alveolar exudate may suggest that acute interstitial pnemonia progresses from the exudative stage of diffuse alveolar damage. | ||
*[ | *Diffuse [[Alveolus|alveolar]] damage occurs in 3 stages.<ref name="pmid23028252">{{cite journal |vauthors=Nur Urer H, Ersoy G, Yılmazbayhan ED |title=Diffuse alveolar damage of the lungs in forensic autopsies: assessment of histopathological stages and causes of death |journal=ScientificWorldJournal |volume=2012 |issue= |pages=657316 |date=2012 |pmid=23028252 |pmc=3458269 |doi=10.1100/2012/657316 |url=}}</ref><ref name="pmid19647854">{{cite journal |vauthors=Kang D, Nakayama T, Togashi M, Yamamoto M, Takahashi M, Kunugi S, Ishizaki M, Fukuda Y |title=Two forms of diffuse alveolar damage in the lungs of patients with acute respiratory distress syndrome |journal=Hum. Pathol. |volume=40 |issue=11 |pages=1618–27 |date=November 2009 |pmid=19647854 |doi=10.1016/j.humpath.2009.04.019 |url=}}</ref> | ||
* | **Acute, [[Exudate|exudative]] | ||
*[ | **Proliferative, organizing | ||
* | **[[Fibrosis|Fibrotic]] | ||
* | *The rapid and abrupt onset of a widespread [[injury]] pattern may be suggested as an initiating factor involving [[Lung|pulmonary]] [[endothelium]]. This is followed by damage to [[Alveolus|alveolar]] [[epithelium]] and [[Programmed cell death|cell death]], that leads to release of mediating factors such as [[tumor necrosis factor alpha]], [[Interleukin|interleukins]] and monocyte chemoattractant factor. | ||
*Followed by the influx of [[Neutrophil|neutrophils]] into the [[Alveolus|alveolar]] spaces and [[Alveolus|alveolar walls]] leads to further cellular damage, by the release of toxic [[Free radicals|oxygen free radicals]] and [[Protease|proteases]]. | |||
*[[Neutrophil|Neutrophils]] and other [[Inflammation|inflammatory cells]] can contribute to the progression of the epithelial cell injury and airspace [[Exudate|exudation]]. | |||
*The extent of [[Epithelium|epithelial]] [[injury]] and [[basement membrane]] damage may modulate the nature and extent of the subsequent [[Fibroblast|fibroblastic]] response in [[Hamman-Rich syndrome|acute interstitial pneumonitis]]. | |||
*Following the acute phase, a stage of organization occurs. | |||
**The [[Hyaline|hyaline membranes]] are resorbed into the [[Alveolus|alveolar septa]] and overgrown by proliferating [[Pneumocytes|type II pneumocytes]]. | |||
*In fibrotic phase, proliferation of [[Fibroblast|fibroblasts]] and differentiation into [[Myofibroblast|myofibroblasts]] leads to the production of [[collagen]], causes widening of the [[Alveolus|alveolar]] septa, and organization of the [[Alveolus|alveolar]] [[exudate]]. | |||
*Collapse of [[Alveolus|alveolar]] wall and apposition, associated with reepithelization of the fibrotic exudate within the [[Alveolus|alveolar]] space may contribute to the severity and extent of the [[Fibrosis|fibrotic process]]. | |||
== | ==Gross Pathology== | ||
== | *Patients with [[Hamman-Rich syndrome|acute interstitial pneumonitis]], [[Gross examination|gross appearance]] of [[Lung|lungs]] is identical to the [[Patient|patients]] with [[Acute respiratory distress syndrome|ARDS]].<ref name="pmid11019719">{{cite journal |vauthors=Tomashefski JF |title=Pulmonary pathology of acute respiratory distress syndrome |journal=Clin. Chest Med. |volume=21 |issue=3 |pages=435–66 |date=September 2000 |pmid=11019719 |doi= |url=}}</ref> | ||
* | *The [[Gross examination|gross appearance]] of [[Lung|lungs]] correlates with the stage of the [[Acute respiratory distress syndrome|diffuse alveolar damage]]. | ||
**In the early phase, the [[Lung|lungs]] are firm, boggy, and have a dark red or beefy appearance. | |||
**In later phases, the [[Lung|lungs]] are extremely heavy due to [[edema]] and show irregular areas of dense [[Consolidation (medicine)|consolidation]] and [[fibrosis]]. | |||
**As the [[fibrosis]] progresses, cobblestoning of the [[Pleura|pleural surface]] may occur. | |||
**Formation of peripheral [[Cyst|cysts]] and honeycombing may suggest the possibility of underlying chronic [[Fibrosis|fibrotic lung disease]]. | |||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
*On microscopic [[Histopathology|histopathological analysis]], [[Hamman-Rich syndrome|Acute interstitial pneumonitis]] will show following features:<ref name="pmid23001802">{{cite journal |vauthors=Mukhopadhyay S, Parambil JG |title=Acute interstitial pneumonia (AIP): relationship to Hamman-Rich syndrome, diffuse alveolar damage (DAD), and acute respiratory distress syndrome (ARDS) |journal=Semin Respir Crit Care Med |volume=33 |issue=5 |pages=476–85 |date=October 2012 |pmid=23001802 |doi=10.1055/s-0032-1325158 |url=}}</ref> | *On microscopic [[Histopathology|histopathological analysis]], [[Hamman-Rich syndrome|Acute interstitial pneumonitis]] will show following features:<ref name="pmid23001802">{{cite journal |vauthors=Mukhopadhyay S, Parambil JG |title=Acute interstitial pneumonia (AIP): relationship to Hamman-Rich syndrome, diffuse alveolar damage (DAD), and acute respiratory distress syndrome (ARDS) |journal=Semin Respir Crit Care Med |volume=33 |issue=5 |pages=476–85 |date=October 2012 |pmid=23001802 |doi=10.1055/s-0032-1325158 |url=}}</ref><ref name="pmid12570127">{{cite journal |vauthors=Bonaccorsi A, Cancellieri A, Chilosi M, Trisolini R, Boaron M, Crimi N, Poletti V |title=Acute interstitial pneumonia: report of a series |journal=Eur. Respir. J. |volume=21 |issue=1 |pages=187–91 |date=January 2003 |pmid=12570127 |doi= |url=}}</ref> | ||
**[[Diffuse alveolar damage]] | **[[Diffuse alveolar damage]] | ||
**[[Hyaline]] membrane formation | **[[Hyaline]] membrane formation | ||
**[[Interstitial lung disease|Interstitial fibrosis]]: | **[[Interstitial lung disease|Interstitial fibrosis]]: | ||
***It is [[diffuse]], [[Uniform distribution|uniform]] temporally with extensive [[Fibroblast|fibroblastic]] and [[Myofibroblast|myofibroblastic]] proliferation and relatively less [[collagen]] deposition. | ***It is [[diffuse]], bilateral, [[Uniform distribution|uniform]] temporally with extensive [[Fibroblast|fibroblastic]] and [[Myofibroblast|myofibroblastic]] proliferation and relatively less [[collagen]] deposition. | ||
***The [[Uniform distribution|uniformity]] of the [[Fibroblast|fibroblastic]]/[[Myofibroblast|myofibroblastic]] proliferation and prominent activity distinguish AIP from the other types of idiopathic interstitial pneumonia. | ***The [[Uniform distribution|uniformity]] of the [[Fibroblast|fibroblastic]]/[[Myofibroblast|myofibroblastic]] proliferation and prominent activity distinguish AIP from the other types of idiopathic interstitial pneumonia. | ||
**[[Pneumocyte|Type II pneumocyte]] [[hyperplasia]] with cytologic [[atypia]] and [[Respiratory epithelium|bronchiolar]] [[Squamous epithelium|squamous]] [[metaplasia]] is present. | **[[Pneumocyte|Type II pneumocyte]] [[hyperplasia]] with cytologic [[atypia]] and [[Respiratory epithelium|bronchiolar]] [[Squamous epithelium|squamous]] [[metaplasia]] is present. | ||
| Line 67: | Line 49: | ||
**[[Biopsy|Biopsies]] taken in the later course of the [[disease]] show: | **[[Biopsy|Biopsies]] taken in the later course of the [[disease]] show: | ||
***Enlarged and remodeled [[Alveolus|airspaces]] that resemble honeycomb change of UIP (usual interstitial fibrosis), but extensive [[Fibroblast|fibroblastic]]/ [[Myofibroblast|myofibroblastic]] proliferation and [[collagen]] deposition is still present within the walls of the [[Alveolus|alveoli]]. | ***Enlarged and remodeled [[Alveolus|airspaces]] that resemble honeycomb change of UIP (usual interstitial fibrosis), but extensive [[Fibroblast|fibroblastic]]/ [[Myofibroblast|myofibroblastic]] proliferation and [[collagen]] deposition is still present within the walls of the [[Alveolus|alveoli]]. | ||
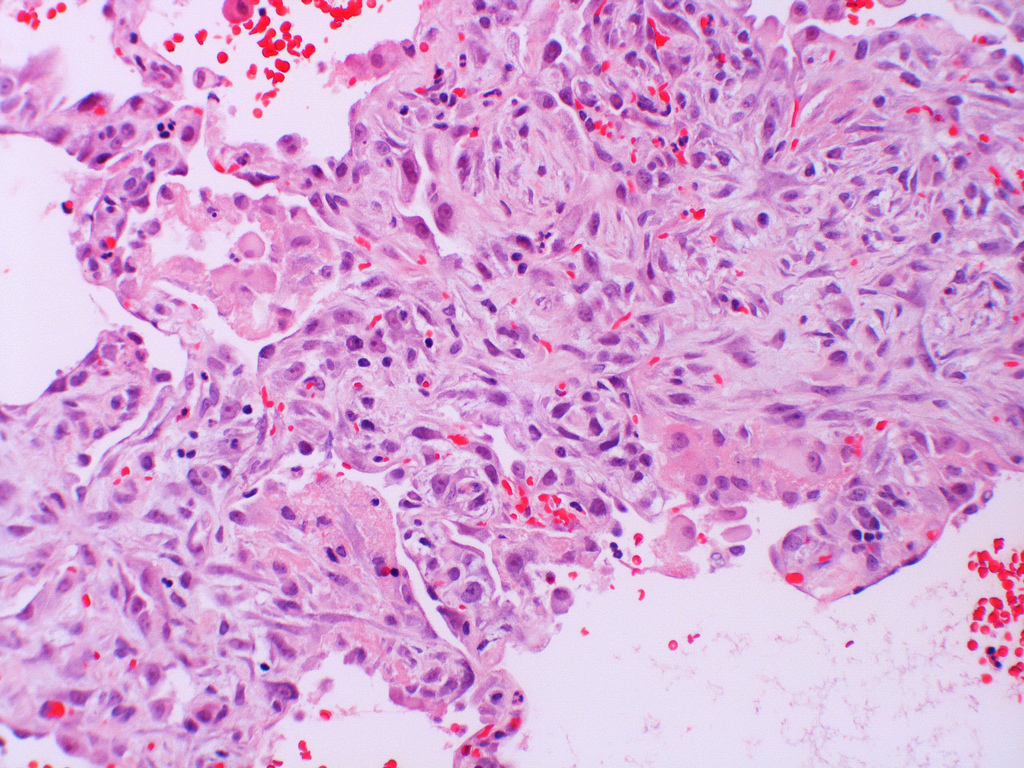
[[File:Acute interstitial pneumonia (AIP) Idiopathic DAD.jpg|center|thumb|[[Idiopathic]] DAD<ref>By Yale Rosen [CC BY-SA 2.0 (<nowiki>https://creativecommons.org/licenses/by-sa/2.0</nowiki>)], via Wikimedia Commons</ref> in [[Hamman-Rich syndrome|Acute interstitial pneumonia]]]] | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
| Line 80: | Line 62: | ||
{{WS}} | {{WS}} | ||
[[Category:Pulmonology]] | [[Category: Pulmonology]] | ||
Latest revision as of 20:57, 23 March 2018
|
Hamman-Rich syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hamman-Rich syndrome pathophysiology On the Web |
|
American Roentgen Ray Society Images of Hamman-Rich syndrome pathophysiology |
|
Risk calculators and risk factors for Hamman-Rich syndrome pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Chandrakala Yannam, MD [2]
Overview
Acute interstitial pneumonitis shows the histopathologic appearance of diffuse alveolar damage. On gross examination, lungs appear firm, heavy and have a dark red or beefy appearance and show irregular areas of consolidation and fibrosis. On microscopic examination, acute interstitial pneumonitis shows bilateral, temporal uniformity of the diffuse alveolar damage, hyaline membrane deposition and extensive fibroblastic and myofibroblastic proliferation.
Pathophysiology
Pathogenesis
- The mechanism of initial injury to the pulmonary epithelium in acute interstitial pneumonitis is not known.
- Based on the findings of lung biopsy, the uniformity and extent of the injury, it is assumed that a single insult triggers the pathologic process.
- On microscopy, appearance of hyaline membrane remenats and organizing alveolar exudate may suggest that acute interstitial pnemonia progresses from the exudative stage of diffuse alveolar damage.
- Diffuse alveolar damage occurs in 3 stages.[1][2]
- The rapid and abrupt onset of a widespread injury pattern may be suggested as an initiating factor involving pulmonary endothelium. This is followed by damage to alveolar epithelium and cell death, that leads to release of mediating factors such as tumor necrosis factor alpha, interleukins and monocyte chemoattractant factor.
- Followed by the influx of neutrophils into the alveolar spaces and alveolar walls leads to further cellular damage, by the release of toxic oxygen free radicals and proteases.
- Neutrophils and other inflammatory cells can contribute to the progression of the epithelial cell injury and airspace exudation.
- The extent of epithelial injury and basement membrane damage may modulate the nature and extent of the subsequent fibroblastic response in acute interstitial pneumonitis.
- Following the acute phase, a stage of organization occurs.
- The hyaline membranes are resorbed into the alveolar septa and overgrown by proliferating type II pneumocytes.
- In fibrotic phase, proliferation of fibroblasts and differentiation into myofibroblasts leads to the production of collagen, causes widening of the alveolar septa, and organization of the alveolar exudate.
- Collapse of alveolar wall and apposition, associated with reepithelization of the fibrotic exudate within the alveolar space may contribute to the severity and extent of the fibrotic process.
Gross Pathology
- Patients with acute interstitial pneumonitis, gross appearance of lungs is identical to the patients with ARDS.[3]
- The gross appearance of lungs correlates with the stage of the diffuse alveolar damage.
- In the early phase, the lungs are firm, boggy, and have a dark red or beefy appearance.
- In later phases, the lungs are extremely heavy due to edema and show irregular areas of dense consolidation and fibrosis.
- As the fibrosis progresses, cobblestoning of the pleural surface may occur.
- Formation of peripheral cysts and honeycombing may suggest the possibility of underlying chronic fibrotic lung disease.
Microscopic Pathology
- On microscopic histopathological analysis, Acute interstitial pneumonitis will show following features:[4][5]
- Diffuse alveolar damage
- Hyaline membrane formation
- Interstitial fibrosis:
- It is diffuse, bilateral, uniform temporally with extensive fibroblastic and myofibroblastic proliferation and relatively less collagen deposition.
- The uniformity of the fibroblastic/myofibroblastic proliferation and prominent activity distinguish AIP from the other types of idiopathic interstitial pneumonia.
- Type II pneumocyte hyperplasia with cytologic atypia and bronchiolar squamous metaplasia is present.
- Thickening and distortion of alveolar septa caused by spindle cell proliferation.
- Intraluminal polypoid plugs formation
- Organizing thrombi in small and medium-sized arteries
- Biopsies taken in the later course of the disease show:
- Enlarged and remodeled airspaces that resemble honeycomb change of UIP (usual interstitial fibrosis), but extensive fibroblastic/ myofibroblastic proliferation and collagen deposition is still present within the walls of the alveoli.
References
- ↑ Nur Urer H, Ersoy G, Yılmazbayhan ED (2012). "Diffuse alveolar damage of the lungs in forensic autopsies: assessment of histopathological stages and causes of death". ScientificWorldJournal. 2012: 657316. doi:10.1100/2012/657316. PMC 3458269. PMID 23028252.
- ↑ Kang D, Nakayama T, Togashi M, Yamamoto M, Takahashi M, Kunugi S, Ishizaki M, Fukuda Y (November 2009). "Two forms of diffuse alveolar damage in the lungs of patients with acute respiratory distress syndrome". Hum. Pathol. 40 (11): 1618–27. doi:10.1016/j.humpath.2009.04.019. PMID 19647854.
- ↑ Tomashefski JF (September 2000). "Pulmonary pathology of acute respiratory distress syndrome". Clin. Chest Med. 21 (3): 435–66. PMID 11019719.
- ↑ Mukhopadhyay S, Parambil JG (October 2012). "Acute interstitial pneumonia (AIP): relationship to Hamman-Rich syndrome, diffuse alveolar damage (DAD), and acute respiratory distress syndrome (ARDS)". Semin Respir Crit Care Med. 33 (5): 476–85. doi:10.1055/s-0032-1325158. PMID 23001802.
- ↑ Bonaccorsi A, Cancellieri A, Chilosi M, Trisolini R, Boaron M, Crimi N, Poletti V (January 2003). "Acute interstitial pneumonia: report of a series". Eur. Respir. J. 21 (1): 187–91. PMID 12570127.
- ↑ By Yale Rosen [CC BY-SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0)], via Wikimedia Commons