Trichomoniasis laboratory findings
|
Trichomoniasis Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Trichomoniasis laboratory findings On the Web |
|
American Roentgen Ray Society Images of Trichomoniasis laboratory findings |
|
Risk calculators and risk factors for Trichomoniasis laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Maliha Shakil, M.D. [2], Aysha Anwar, M.B.B.S[3]
Overview
Laboratory tests used in the diagnosis of trichomoniasis include saline microscopy, culture, and nucleic acid amplification tests (NAATs).[1]
Laboratory Findings
Microscopy
Wet-mount microscopy: has been used as the preferred diagnostic test, however it has low sensitivity (44%–68%) compared with culture. To improve detection, clinicians using wet mounts should attempt to evaluate slides immediately after specimen collection because sensitivity decreases quickly to 20% within 1 hour after collection.[2]
Trichomoniasis is diagnosed by visually observing the trichomonads via a microscope. In women, the examiner collects the specimen during a pelvic examination by inserting a speculum into the vagina and then using a cotton-tipped applicator to collect the sample. The sample is then placed onto a microscopic slide and sent to a laboratory to be analyzed. Trichomoniasis has been difficult to diagnose due to the poor sensitivity of the tests.[3][1] [4][5]
Findings on microscopy suggestive of trichomoniasis include:[6][7]
- Characteristic "tumbling" motility of protozoa
- Leukocytes
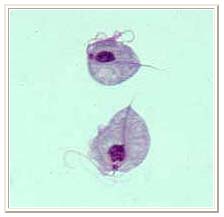
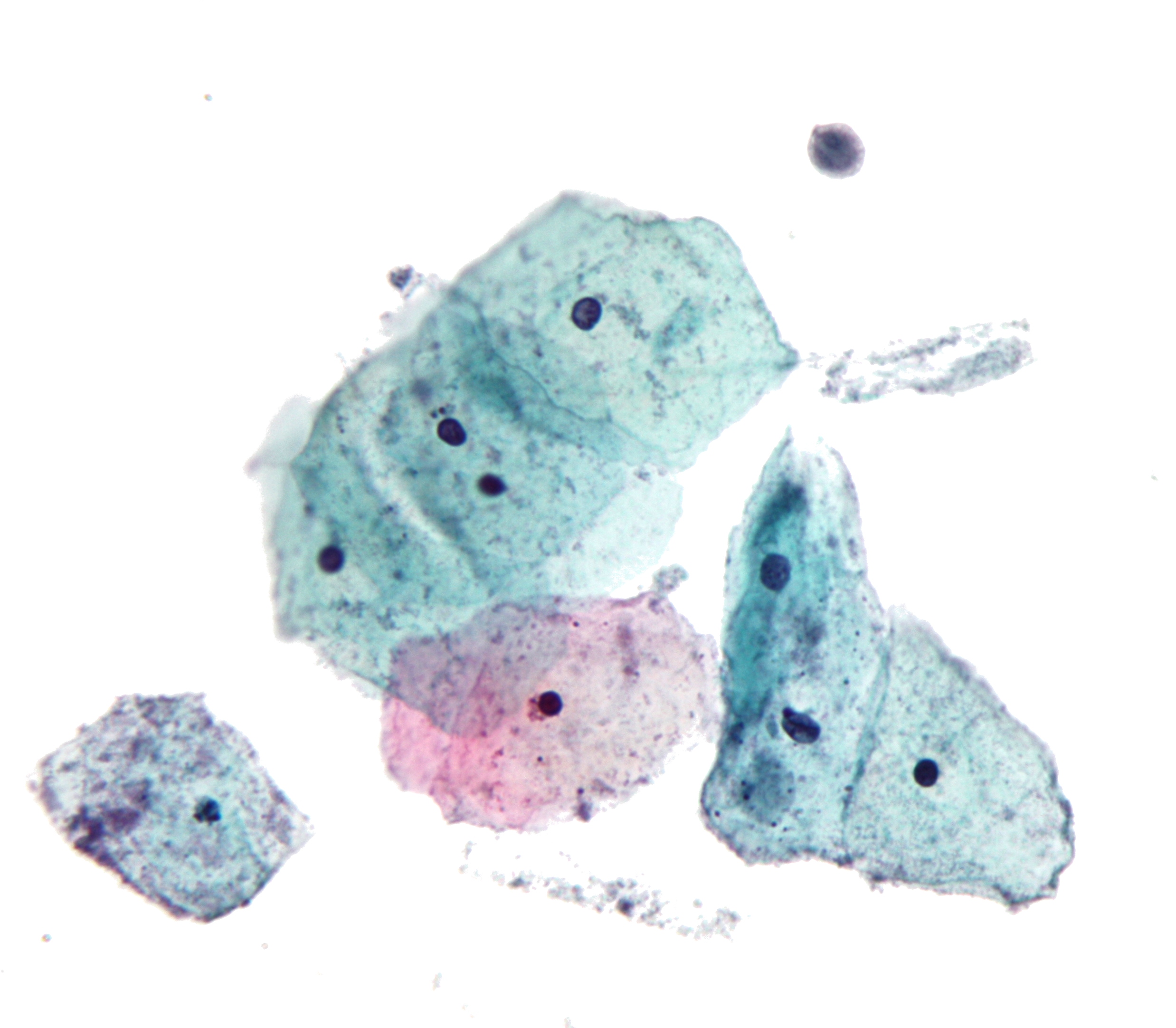
| Trichomonas vaginalis | Pap smear |
|---|---|
 |
|
Two trophozoites of Trichomonas vaginalis obtained from in vitro culture. Smear was stained with Giemsa.[8]
Culture
Historically, culture has been the gold standard for diagnosis of trichomoniasis. However, sensitivity is somewhat low (70-89%).[9]
Nucleic Acid Amplification Tests
Nucleic acid probe techniques, the most sensitive tests, are moderately priced and fast, but they require instrumentation and thus are not considered point-of-care. The APTIMA Trichomonas vaginalis Assay (Hologic Gen-Probe, San Diego, CA) was FDA-cleared in 2011 for use with urine, endocervical, and vaginal swabs, and endocervical specimens collected in the Hologic PreserveCyt solution (ThinPrep) from females only. Sensitivity is 95–100% and specificity is also 95–100%.[10][11][12]
References
- ↑ 1.0 1.1 http://www.cdc.gov/std/tg2015/trichomoniasis.htm Accessed on September 14, 2016
- ↑ "Trichomoniasis - STI Treatment Guidelines".
- ↑ Andrea SB, Chapin KC (2011). "Comparison of Aptima Trichomonas vaginalis Transcription-Mediated Amplification Assay and BD Affirm VPIII for Detection of T. vaginalis in Symptomatic Women: Performance Parameters and Epidemiological Implications". J Clin Microbiol. 49 (3): 866–9. doi:10.1128/JCM.02367-10. PMID 21248097. Lay summary.
- ↑ Nye, Melinda B., Jane R. Schwebke, and Barbara A. Body. "Comparison of APTIMA Trichomonas vaginalis transcription-mediated amplification to wet mount microscopy, culture, and polymerase chain reaction for diagnosis of trichomoniasis in men and women." American journal of obstetrics and gynecology 200.2 (2009): 188-e1.
- ↑ Stoner, Kevin A., et al. "Survival of Trichomonas vaginalis in wet preparation and on wet mount." Sexually transmitted infections (2013): sextrans-2012.
- ↑ Hobbs MM, Seña AC (2013). "Modern diagnosis of Trichomonas vaginalis infection". Sex Transm Infect. 89 (6): 434–8. doi:10.1136/sextrans-2013-051057. PMC 3787709. PMID 23633669.
- ↑ Schwebke JR, Burgess D (2004). "Trichomoniasis". Clin Microbiol Rev. 17 (4): 794–803, table of contents. doi:10.1128/CMR.17.4.794-803.2004. PMC 523559. PMID 15489349.
- ↑ "DPDx - Trichomoniasis". Retrieved 2012-12-27.
- ↑ Trichomoniasis . Wikipedia.https://en.wikipedia.org/wiki/Trichomoniasis Accessed on February 4, 2016
- ↑ Kissinger P (2015). "Trichomonas vaginalis: a review of epidemiologic, clinical and treatment issues". BMC Infect Dis. 15: 307. doi:10.1186/s12879-015-1055-0. PMC 4525749. PMID 26242185.
- ↑ Nye, Melinda B., Jane R. Schwebke, and Barbara A. Body. "Comparison of APTIMA Trichomonas vaginalis transcription-mediated amplification to wet mount microscopy, culture, and polymerase chain reaction for diagnosis of trichomoniasis in men and women." American journal of obstetrics and gynecology 200.2 (2009): 188-e1.
- ↑ Kingston, M. A., D. Bansal, and E. M. Carlin. "'Shelf life'of Trichomonas vaginalis." International journal of STD & AIDS 14.1 (2003): 28.