Pneumonia natural history, complications, and prognosis
|
Pneumonia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pneumonia natural history, complications, and prognosis On the Web |
|
American Roentgen Ray Society Images of Pneumonia natural history, complications, and prognosis |
|
FDA on Pneumonia natural history, complications, and prognosis |
|
CDC onPneumonia natural history, complications, and prognosis |
|
Pneumonia natural history, complications, and prognosis in the news |
|
Blogs on Pneumonia natural history, complications, and prognosis |
|
Risk calculators and risk factors for Pneumonia natural history, complications, and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ;Associate Editor(s)-in-Chief: Hamid Qazi, MD, BSc [2], Priyamvada Singh, M.D. [3]
Overview
Pneumonia is an infection of the lungs that can cause mild to severe illness in people of all ages. The incubation period is between 1 and 3 days and symptoms include fever, cough, chest pain, dyspnea and tachypnea. Complications of pneumonia include sepsis, respiratory failure, pleural effusion, empyema, and lung abscess. Most types of pneumonia can be completely cured with the appropriate medical therapy and mortality rates can be 1%, depending on the age and comorbidities.
Natural History
- Pneumococcal pneumonia is the most common clinical presentation of pneumococcal disease among adults, although pneumonia without bacteremia or empyema is not considered to be “invasive” disease. [1]
- The incubation period of pneumococcal pneumonia is short, about 1 to 3 days. [1]
- Symptoms generally include an abrupt onset of fever and chills or rigors. [1]
- Typically there is a single rigor, and repeated shaking chills are uncommon. [1]
- Other common symptoms include pleuritic chest pain, cough productive of mucopurulent, rusty sputum, dyspnea, tachypnea, hypoxia, tachycardia, malaise, and weakness. Nausea, vomiting, and headaches occur less frequently.[1]
- Transmission of streptococcus pneumonia occurs as a result of direct person-to-person contact via respiratory droplets and by autoinoculation in persons carrying the bacteria in their upper respiratory tract. [1]
- The pneumococcal serotypes most often responsible for causing infection are those most frequently found in carriers.[1]
Complications
Despite appropriate antibiotic therapy, severe complications can result from CAP, including:
Sepsis
- Sepsis can occur when microorganisms enter the blood stream and the immune system responds.
- Sepsis most often occurs with bacterial pneumonia
- Streptococcus pneumoniae is the most common cause.
- Individuals with sepsis require hospitalization in an intensive care unit. They often require medications and intravenous fluids to keep their blood pressure from going too low. Sepsis can cause liver, kidney, and heart damage among other things.
Respiratory Failure
- If enough of the lung is involved, it may not be possible for a person to breathe enough to live without support.
- Non-invasive machines such as a bilevel positive airway pressure machine may be used.
- Otherwise, placement of a breathing tube into the mouth may be necessary. A ventilator may also be used to help the person breathe.
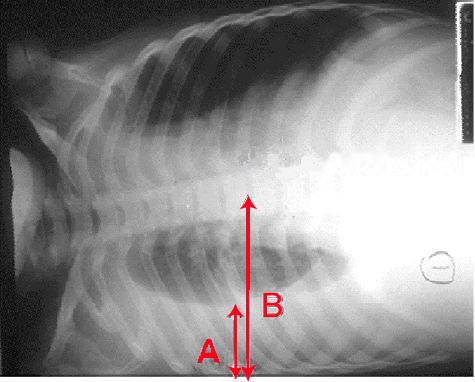
Pleural Effusion and Empyema
- Occasionally, microorganisms from the lung will cause fluid to form in the space surrounding the lung, called the pleural cavity.
- If the microorganisms themselves are present, the fluid collection is often called an empyema.
- If pleural fluid is present in a person with CAP, the fluid should be collected with a needle (thoracentesis) and examined.
- Depending on the result of the examination, complete drainage of the fluid may be necessary, often with a chest tube. If the fluid is not drained, bacteria can continue to cause illness because antibiotics do not penetrate well into the pleural cavity.
Abscess
- Rarely, microorganisms in the lung will form a pocket of fluid and bacteria called an abscess.
- Abscesses can be seen on an x-ray as a cavity within the lung. Abscesses typically occur in aspiration pneumonia and most often contain a mixture of anaerobic bacteria.
- Usually antibiotics are able to fully treat abscesses, but sometimes they must be drained by a surgeon or radiologist.
Sometimes pneumonia can lead to additional complications. Complications are more frequently associated with bacterial pneumonia than with viral pneumonia. The most important complications include:
Respiratory and Circulatory Failure
- Because pneumonia affects the lungs, often people with pneumonia have difficulty breathing, and it may not be possible for them to breathe well enough to stay alive without support.
- Non-invasive breathing assistance may be helpful, such as with a bilevel positive airway pressure machine.
- In other cases, placement of an endotracheal tube (breathing tube) may be necessary, and a ventilator may be used to help the person breathe.
- Pneumonia can also cause respiratory failure by triggering acute respiratory distress syndrome (ARDS), which results from a combination of infection and inflammatory response.
- The lungs quickly fill with fluid and become very stiff. This stiffness, combined with severe difficulties extracting oxygen due to the alveolar fluid, creates a need for mechanical ventilation.
- Sepsis and septic shock are potential complications of pneumonia.
- Sepsis occurs when microorganisms enter the bloodstream and the immune systemresponds by secreting cytokines.
- Sepsis most often occurs with bacterial pneumonia; Streptococcus pneumoniae is the most common cause.
- Individuals with sepsis or septic shock need hospitalization in an intensive care unit.
- They often require intravenous fluids and medications to help keep their blood pressure from dropping too low.
- Sepsis can cause liver, kidney, and heart damage, among other problems, and it often causes death.
Prognosis
- Individuals who are treated for CAP outside of the hospital have a mortality rate less than 1%.
- Fever typically responds in the first two days of therapy and other symptoms resolve in the first week.
- The x-ray, however, may remain abnormal for at least a month, even when CAP has been successfully treated.
- Among individuals who require hospitalization, the mortality rate averages 12% overall, but it is as much as 40% in people who have bloodstream infections or require intensive care.[4]
- When CAP does not respond as expected, there are several possible causes.
- A complication of CAP may have occurred or a previously unknown health problem may be playing a role.
- Additional causes include inappropriate antibiotics for the causative organism (ie DRSP), a previously unsuspected microorganism (such as tuberculosis), or a condition which mimics CAP (such as Wegener's granulomatosis).
- Additional testing may be performed and may include additional radiologic imaging (such as a computed tomography scan) or a procedure such as a bronchoscopy or lung biopsy.
Prognosis and Mortality
- With treatment, most types of bacterial pneumonia can be cured within one to two weeks.
- Viral pneumonia may last longer, and mycoplasmal pneumonia may take four to six weeks to resolve completely.
- The eventual outcome of an episode of pneumonia depends on how ill the person is when he or she is first diagnosed.
- In the United States, about one of every twenty people with pneumococcal pneumonia will die.[2]
- In cases where the pneumonia progresses to blood poisoning (bacteremia), one of every five will die. The death rate (or mortality) also depends on the underlying cause of the pneumonia. Pneumonia caused by Mycoplasma, for instance, is associated with little mortality. However, about half of the people who develop methicillin-resistant Staphylococcus aureus (MRSA) pneumonia while on a ventilator will die.[3]
- In regions of the world without advanced health care systems, pneumonia is even deadlier.
- Limited access to clinics and hospitals, limited access to x-rays, limited antibiotic choices, and inability to treat underlying conditions inevitably leads to higher rates of death from pneumonia.
Clinical Prediction Rules
- Clinical prediction rules have been developed to more objectively prognosticate outcomes in pneumonia.
- These rules can be helpful in deciding whether or not to hospitalize the person.
- Pneumonia severity index[4] -online calculator
- CURB-65 score, which takes into account the severity of symptoms, any underlying diseases, and age.[5]
Community Acquired Pneumonia
Natural History
- Pneumococcal pneumonia is the most common clinical presentation of pneumococcal disease amongst adults, although pneumonia without bacteremia or empyema is not considered to be “invasive” disease. [1]
- The incubation period of pneumococcal pneumonia is short, about 1 to 3 days. [1]
- Symptoms generally include an abrupt onset of fever and chills or rigors. [1]
- Typically there is a single rigor; repeated shaking chills are uncommon. [1]
- Other common symptoms include: pleuritic chest pain, cough productive of mucopurulent, rusty sputum, dyspnea, tachypnea, hypoxia, tachycardia, malaise, and weakness. Nausea, vomiting, and headaches occur less frequently.[1]
- Transmission of Streptococcus pneumoniae occurs as a result of direct person-to-person contact via respiratory droplets and by autoinoculation in persons carrying the bacteria in their upper respiratory tract. [1]
Causes
- The pneumococcal serotypes most often responsible for causing infection are those that are most frequently found in carriers.[1]
- Pneumococcal pneumonia is the most common clinical presentation of pneumococcal disease amongst adults, although pneumonia without bacteremia or empyema is not considered to be “invasive” disease. [1]
- The incubation period of pneumococcal pneumonia is short, about 1 to 3 days. [1]
- Symptoms generally include an abrupt onset of fever and chills or rigors. [1]
- Typically there is a single rigor; repeated shaking chills are uncommon. [1]
- Other common symptoms include: pleuritic chest pain, cough productive of mucopurulent, rusty sputum, dyspnea, tachypnea, hypoxia, tachycardia, malaise, and weakness. Nausea, vomiting, and headaches occur less frequently.[1]
- Transmission of Streptococcus pneumoniae occurs as a result of direct person-to-person contact via respiratory droplets and by autoinoculation in persons carrying the bacteria in their upper respiratory tract. [1]
- The pneumococcal serotypes most often responsible for causing infection are those that are most frequently found in carriers.[1]
Complications
Pleural Effusion and Empyema
- Community-acquired pneumonia may be complicated by parapneumonic pleural effusions. Thoracentesis and pleural fluid analysis should be performed.
- Empyema may occur if there is local formation of pus in the pleural cavity; this requires drainage in addition to antibiotic therapy.
Abscess
- Intraparenchymal abscesses (with or without loculation) may be seen in aspiration pneumonia. They are often primarily anaerobic or polymicrobial.
Sepsis and Septic Shock
- Sepsis most often occurs with bacterial pneumonia, with Streptococcus pneumoniae as the most common etiology.
Respiratory Failure
- Patients at the opposite ends of the age spectrum are at a high risk of respiratory failure.
- Non-invasive maneuvers, such as a bilevel positive airway pressure (BI-PAP) machine, may be used for respiratory support. Otherwise, intubation with mechanical ventilation may be required.
- Pneumonia may be complicated by acute respiratory distress syndrome (ARDS), which results from a combination of infection and inflammatory response.
Prognosis and Mortality
- With treatment, most types of bacterial pneumonia can be cured within one to two weeks.
- Viral pneumonia may last longer, and mycoplasmal pneumonia may take four to six weeks to resolve completely.
- The eventual outcome of an episode of pneumonia depends on how ill the person is when he or she is first diagnosed.
- In the United States, about one out of every twenty people with pneumococcal pneumonia will die.[6]
- In cases where pneumonia progresses to blood poisoning (bacteremia), one of every five will die.
- The death rate (or mortality) also depends on the underlying cause of the pneumonia.
- Pneumonia caused by Mycoplasma, for instance, is associated with little mortality. However, about half of the people who develop methicillin-resistant Staphylococcus aureus (MRSA) pneumonia while on a ventilator will die.[3]
- In regions of the world without advanced health care systems, pneumonia is even deadlier.
- Limited access to clinics and hospitals, x-rays, antibiotic choices, and inability to treat underlying conditions will inevitably lead to higher rates of death from pneumonia.
- Individuals who are treated for CAP outside of the hospital have a mortality rate of less than 1%.
- Fever typically responds in the first two days of therapy and other symptoms resolve in the first week.
- The CXR, however, may remain abnormal for at least a month, even when CAP has been successfully treated.
- Amongst individuals who require hospitalization, the mortality rate averages 12% overall, but it is as much as 40% in people who have bloodstream infections or require intensive care.[5]
- When CAP does not respond as expected, there are several possible causes.
- A complication of CAP may have occurred or a previously unknown health problem may be playing a role.
- Additional causes include: inappropriate antibiotics for the causative organism (such as drug resistant Streptococcus pneumoniae, a previously unsuspected microorganism (such as tuberculosis), or a condition which mimics CAP (such as Wegener's granulomatosis).
- Additional testing may be performed and may include radiologic imaging (such as a computed tomography scan) or a procedure such as a bronchoscopy or lung biopsy.
Hospital Acquired Pneumonia
Natural History
- The natural course of hospital-acquired pneumonia will depend on several factors, such as the causative pathogen, the host immune status and the choice of antibiotic therapy.
- By definition, hospital-acquired pneumonia occurs 48 hours or more since hospital admission; and ventilator-associated pneumonia occurs 48 to 72 hours after the patient was intubated. [7]
- Physicians should suspect of hospital-acquired pneumonia in hospitalized patients that develop fever (> 38° C), productive cough and/or leukocytosis associated with a new chest X-ray infiltration.
- Empirical antibiotic therapy should be started in case of high suspicion, as it has shown improvement of patient survival.
Complications
Despite appropriate antibiotic therapy, severe complications can result from HAP, including:
Sepsis
- Sepsis can occur when microorganisms enter the blood stream and the immune system responds.
- Sepsis most often occurs with bacterial pneumonia
- Streptococcus pneumoniae is the most common cause.
- Individuals with sepsis require hospitalization in an intensive care unit. They often require medications and intravenous fluids to keep their blood pressure from going too low. Sepsis can cause liver, kidney, and heart damage among other things.
Respiratory Failure
- If enough of the lung is involved, it may not be possible for a person to breathe enough to live without support.
- Non-invasive machines such as a bilevel positive airway pressure machine may be used.
- Otherwise, placement of a breathing tube into the mouth may be necessary and a ventilator may be used to help the person breathe.
Pleural Effusion and Empyema
- Occasionally, microorganisms from the lung will cause fluid to form in the space surrounding the lung, called the pleural cavity.
- If the microorganisms themselves are present, the fluid collection is often called an empyema.
- If pleural fluid is present in a person with CAP, the fluid should be collected with a needle (thoracentesis) and examined.
- Depending on the result of the examination, complete drainage of the fluid may be necessary, often with a chest tube. If the fluid is not drained, bacteria can continue to cause illness because antibiotics do not penetrate well into the pleural cavity.
Abscess
- Rarely, microorganisms in the lung will form a pocket of fluid and bacteria called an abscess.
- Abscesses can be seen on an x-ray as a cavity within the lung. Abscesses typically occur in aspiration pneumonia and most often contain a mixture of anaerobic bacteria.
- Usually antibiotics are able to fully treat abscesses, but sometimes they must be drained by a surgeon or radiologist.
Prognosis
With treatment, most types of bacterial pneumonia can be cured within one to two weeks. Viral pneumonia may last longer, and mycoplasmal pneumonia may take four to six weeks to resolve completely. The eventual outcome of an episode of pneumonia depends on how ill the person is when he or she is first diagnosed.
In the United States, about one of every twenty people with pneumococcal pneumonia will die.[8] In cases where the pneumonia progresses to blood poisoning (bacteremia), one of every five will die. The death rate (or mortality) also depends on the underlying cause of the pneumonia. Pneumonia caused by Mycoplasma, for instance, is associated with little mortality. However, about half of the people who develop methicillin-resistantStaphylococcus aureus (MRSA) pneumonia while on a ventilator will die.[3] In regions of the world without advanced health care systems, pneumonia is even deadlier.
- Fever typically responds in the first two days of therapy and other symptoms resolve in the first week.
- The x-ray, however, may remain abnormal for at least a month, even when HAP has been successfully treated.
- When HAP does not respond as expected, there are several possible causes.
- A complication of HAP may have occurred or a previously unknown health problem may be playing a role.
- Additional causes include inappropriate antibiotics for the causative organism (ie DRSP), a previously unsuspected microorganism (such as tuberculosis), or a condition which mimics HAP (such as Wegener's granulomatosis).
- Additional testing may be performed and may include additional radiologic imaging (such as a computed tomography scan) or a procedure such as a bronchoscopy or lung biopsy.
Clinical Prediction Rules
Clinical prediction rules have been developed to more objectively prognosticate outcomes in Hospital-acquired pneumonia. Pneumonia severity index[4] -online calculator
- CURB-65 score, which takes into account the severity of symptoms, any underlying diseases, and age[5] -online calculator
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 "CDC Pneumococcal Disease Clinical Features".
- ↑ http://www.kidshealth.org/parent/infections/bacterial_viral/pneumonia.html
- ↑ 3.0 3.1 3.2 Combes A, Luyt CE, Fagon JY, Wollf M, Trouillet JL, Gibert C, Chastre J; PNEUMA Trial Group. Impact of methicillin resistance on outcome of Staphylococcus aureus ventilator-associated pneumonia. Am J Respir Crit Care Med. 2004 Oct 1;170(7):786-92. PMID 15242840
- ↑ 4.0 4.1 Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, Coley CM, Marrie TJ, Kapoor WN. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997 Jan 23;336(4):243–250. PMID 8995086
- ↑ 5.0 5.1 Lim WS, van der Eerden MM, Laing R; et al. (2003). "Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study". Thorax. 58 (5): 377–82. PMID 12728155.
- ↑ http://www.kidshealth.org/parent/infections/bacterial_viral/pneumonia.html
- ↑ "http://www.idsociety.org/uploadedFiles/IDSA/Guidelines-Patient_Care/PDF_Library/HAP.pdf" (PDF). External link in
|title=(help) - ↑ http://www.kidshealth.org/parent/infections/bacterial_viral/pneumonia.html