Osteosarcoma x ray
Jump to navigation
Jump to search
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohammadmain Rezazadehsaatlou[2]
|
Osteosarcoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Osteosarcoma x ray On the Web |
|
American Roentgen Ray Society Images of Osteosarcoma x ray |
Overview
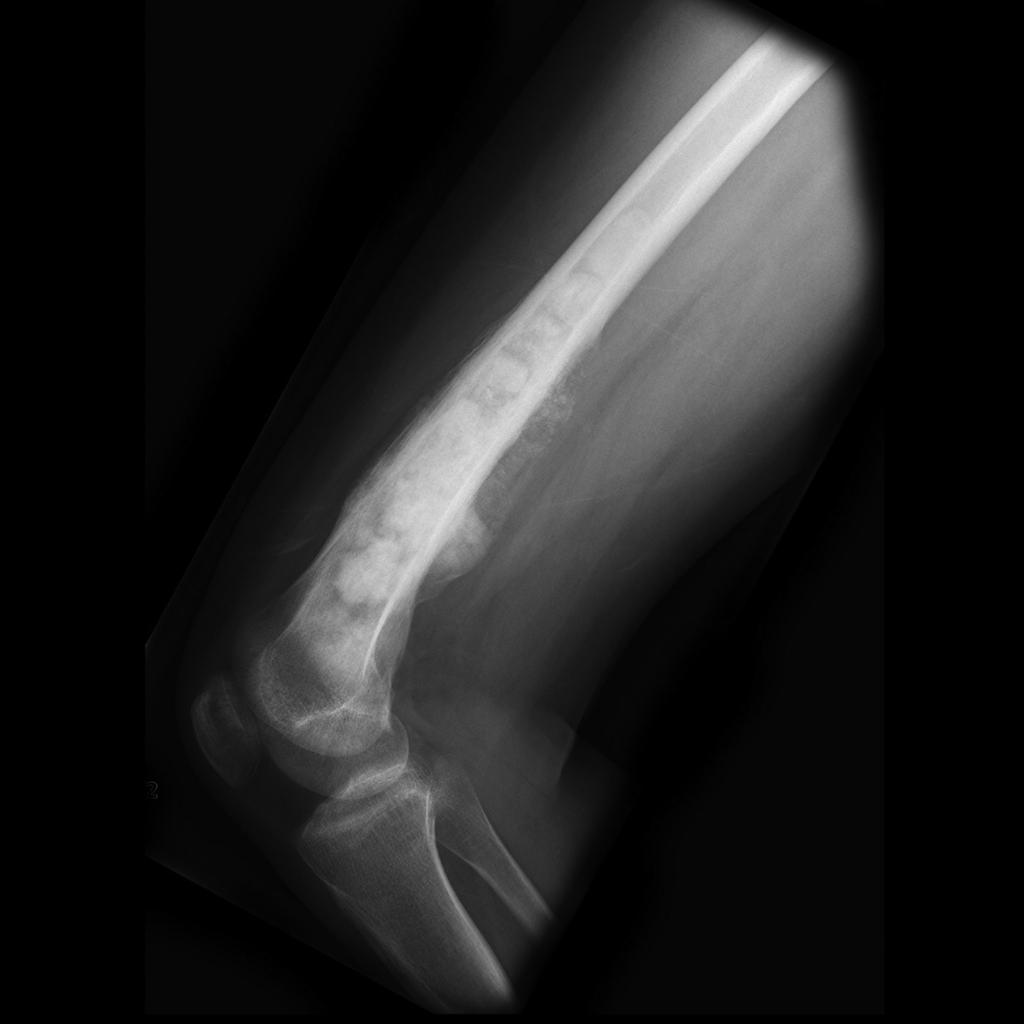
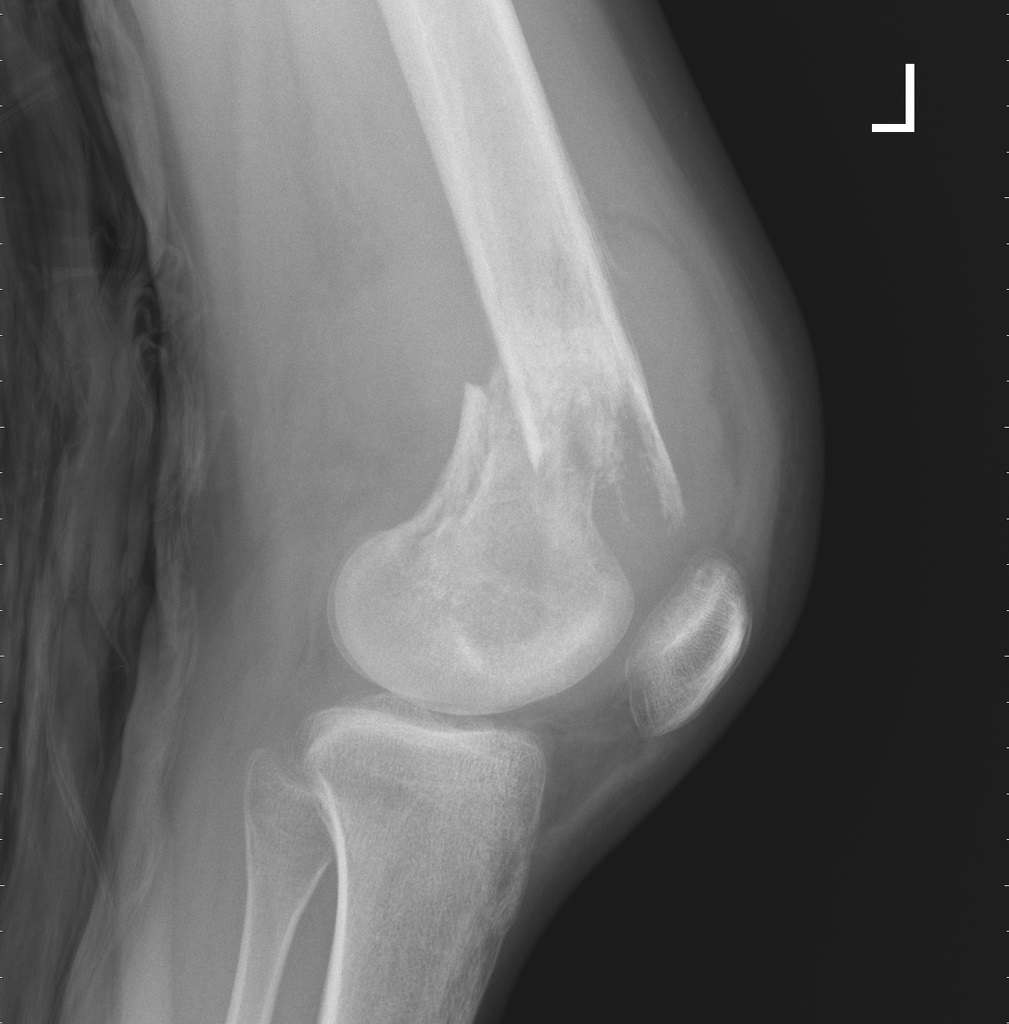
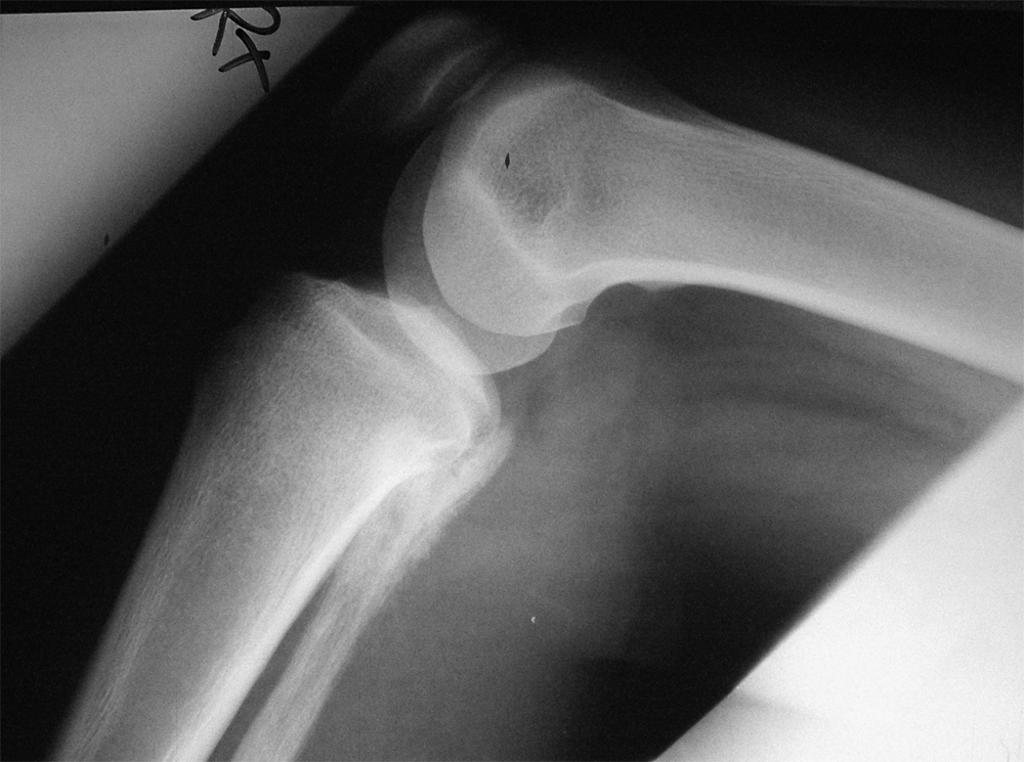
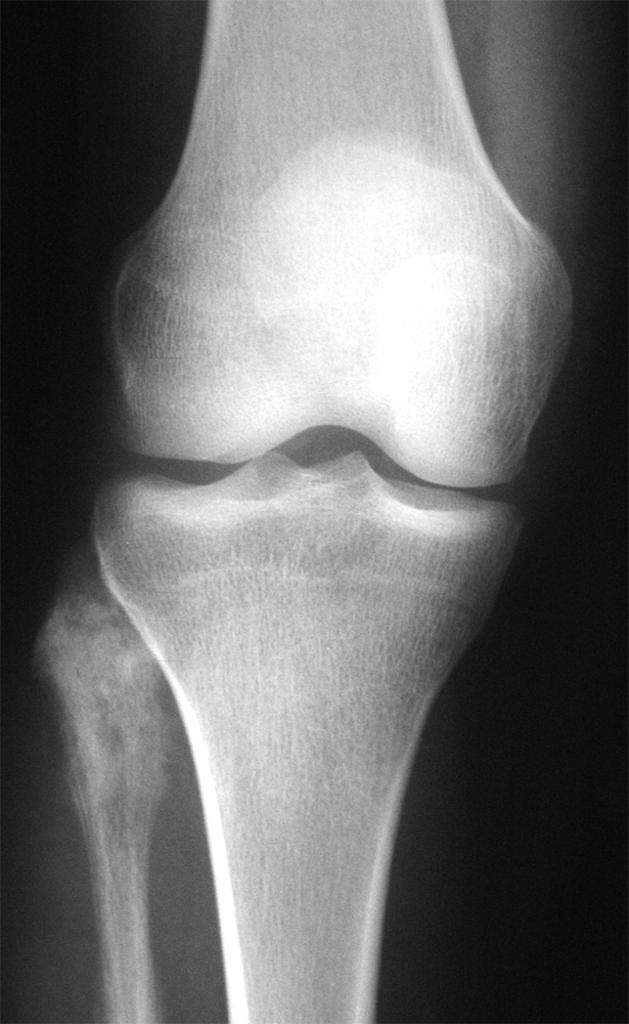
On X-ray, osteosarcoma is characterized by medullary and cortical bone destruction, periosteal reaction, tumor matrix calcification, and soft tissue mass.
X Ray
Conventional radiography continues to play an important role in diagnosis of osteosarcoma. Typical appearances of conventional high grade osteosarcoma include:[1][2][3][4][5][6][7]
- Medullary and cortical bone destruction.
- Wide zone of transition, permeative or moth-eaten appearance.
- Aggressive periosteal reaction characterized by:
- Sunburst appearance
- Codman triangle
- Lamellated (onion skin) reaction: less frequently seen
- Soft-tissue mass.
- Tumor matrix ossification/calcification.
- Variable: reflects a combination of the amount of tumor bone production, calcified matrix, and osteoid.
- Ill-defined fluffy or cloud-like cf. to the rings and arcs of chondroid lesions.
- The following table illustrates the findings on x-ray for the subtypes of osteosarcoma:[1]
| Subtype | X-Ray findings |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
References
- ↑ Jump up to: 1.0 1.1 Osteosarcoma. Dr Amir Rezaee ◉ and Dr Frank Gaillard ◉ et al. Radiopaedia.org 2015. http://radiopaedia.org/articles/osteosarcoma
- ↑ Gürtler KF, Riebel T, Beron G, Heller M, Euler A (April 1984). "[Comparison of x-ray plain films, x-ray tomograms and computed tomograms in lung nodules in children and adolescents]". Rofo (in German). 140 (4): 416–20. doi:10.1055/s-2008-1052998. PMID 6425164.
- ↑ Riebel T, Knop J, Winkler K, Delling G (October 1986). "[Comparative x-ray and nuclear medical studies of osteosarcomas to evaluate the effectiveness of preoperative chemotherapy]". Rofo (in German). 145 (4): 365–72. doi:10.1055/s-2008-1048952. PMID 3022331.
- ↑ Dinkel E, Uhl H, Roeren T (April 1985). "[Lung metastases--limitations and possibilities of radiologic diagnosis]". Radiologe (in German). 25 (4): 158–65. PMID 3889998.
- ↑ Kesselring FO, Penn W (1982). "Radiological aspects of 'classic' primary osteosarcoma: value of some radiological investigations: A review". Diagn Imaging. 51 (2): 78–92. PMID 7042255.
- ↑ Kubo T, Furuta T, Johan MP, Adachi N, Ochi M (September 2016). "Percent slope analysis of dynamic magnetic resonance imaging for assessment of chemotherapy response of osteosarcoma or Ewing sarcoma: systematic review and meta-analysis". Skeletal Radiol. 45 (9): 1235–42. doi:10.1007/s00256-016-2410-y. PMID 27229874.
- ↑ Rothermundt C, Seddon BM, Dileo P, Strauss SJ, Coleman J, Briggs TW, Haile SR, Whelan JS (May 2016). "Follow-up practices for high-grade extremity Osteosarcoma". BMC Cancer. 16: 301. doi:10.1186/s12885-016-2333-y. PMC 4859955. PMID 27154292.