Mycophenolate sodium
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: EMBRYOFETAL TOXICITY, MALIGNANCIES, AND SERIOUS INFECTIONS
See full prescribing information for complete Boxed Warning.
* Use during pregnancy is associated with increased risks of pregnancy loss and congenital malformations.
|
Overview
Mycophenolate sodium is an immunosuppressant that is FDA approved for the prophylaxis of organ rejection in patients receiving a kidney transplant.. There is a Black Box Warning for this drug as shown here. Common adverse reactions include anemia, leukopenia, constipation, nausea, diarrhea, vomiting, dyspepsia, urinary tract infection, CMV infection, insomnia, and postoperative pain.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
- Mycophenolic acid is indicated for the prophylaxis of organ rejection in adult patients receiving a kidney transplant.
- Mycophenolic acid is to be used in combination with cyclosporine and corticosteroids.
Limitations of Use
- Mycophenolic acid delayed-release tablets and mycophenolate mofetil (MMF) tablets and capsules should not be used interchangeably without physician supervision because the rate of absorption following the administration of these two products is not equivalent.
Dosage
Dosage in Adult Kidney Transplant Patients
- The recommended dose of mycophenolic acid delayed-release tablets is 720 mg administered twice daily (1440 mg total daily dose).
DOSAGE FORMS AND STRENGTHS
Mycophenolic acid delayed-release tablets are available as 180 mg and 360 mg tablets.

Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Mycophenolic acid in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Mycophenolic acid in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Indications
- Mycophenolic acid is indicated for the prophylaxis of organ rejection in pediatric patients 5 years of age and older who are at least 6 months post kidney transplant.
- Mycophenolic acid is to be used in combination with cyclosporine and corticosteroids.
Limitations of Use
- Mycophenolic acid delayed-release tablets and mycophenolate mofetil (MMF) tablets and capsules should not be used interchangeably without physician supervision because the rate of absorption following the administration of these two products is not equivalent.
Dosage
- The recommended dose of mycophenolic acid in conversion (at least 6 months post-transplant) pediatric patients age 5 years and older is 400 mg/m2 body surface area (BSA) administered twice daily (up to a maximum dose of 720 mg administered twice daily).
DOSAGE FORMS AND STRENGTHS
Mycophenolic acid delayed-release tablets are available as 180 mg and 360 mg tablets.

Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Mycophenolic acid in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Mycophenolic acid in pediatric patients.
Contraindications
Hypersensitivity Reactions
Mycophenolic acid delayed-release tablets are contraindicated in patients with a hypersensitivity to mycophenolate sodium, mycophenolic acid, mycophenolate mofetil, or to any of its excipients. Reactions like rash, pruritus, hypotension and chest pain have been observed in clinical trials and post marketing reports
Warnings
|
WARNING: EMBRYOFETAL TOXICITY, MALIGNANCIES, AND SERIOUS INFECTIONS
See full prescribing information for complete Boxed Warning.
* Use during pregnancy is associated with increased risks of pregnancy loss and congenital malformations.
|
Embryofetal Toxicity
Use of mycophenolic acid delayed-release tablets during pregnancy is associated with an increased risk of first trimester pregnancy loss and an increased risk of congenital malformations, especially external ear and other facial abnormalities including cleft lip and palate, and anomalies of the distal limbs, heart, esophagus, and kidney.
Pregnancy Exposure Prevention and Planning
Females of reproductive potential must be aware of the increased risk of first trimester pregnancy loss and congenital malformations and must be counseled regarding pregnancy prevention and planning. For recommended pregnancy testing and contraception methods.
Management of Immunosuppression
Only physicians experienced in immunosuppressive therapy and management of organ transplant patients should prescribe mycophenolic acid delayed-release tablets. Patients receiving the drug should be managed in facilities equipped and staffed with adequate laboratory and supportive medical resources. The physicians responsible for maintenance therapy should have complete information requisite for the follow-up of the patient.
Lymphoma and Other Malignancies
Patients receiving immunosuppressants, including mycophenolic acid delayed-release tablets, are at increased risk of developing lymphomas and other malignancies, particularly of the skin. The risk appears to be related to the intensity and duration of immunosuppression rather than to the use of any specific agent.
As usual for patients with increased risk for skin cancer, exposure to sunlight and UV light should be limited by wearing protective clothing and using a sunscreen with a high protection factor.
Post-transplant lymphoproliferative disorder (PTLD) has been reported in immunosuppressed organ transplant recipients. The majority of PTLD events appear related to Epstein Barr Virus (EBV) infection. The risk of PTLD appears greatest in those individuals who are EBV seronegative, a population which includes many young children.
Serious Infections
Patients receiving immunosuppressants, including mycophenolic acid delayed-release tablets, are at increased risk of developing bacterial, viral, fungal, and protozoal infections, and new or reactivated viral infections including opportunistic infections. These infections may lead to serious, including fatal outcomes. Because of the danger of oversuppression of the immune system which can increase susceptibility to infection, combination immunosuppressant therapy should be used with caution.
New or Reactivated Viral Infections
Polyomavirus associated nephropathy (PVAN), JC virus associated progressive multifocal leukoencephalopathy (PML), cytomegalovirus (CMV) infections, reactivation of hepatitis B (HBV) or hepatitis C (HCV) have been reported in patients treated with immunosuppressants, including the mycophenolic acid (MPA) derivatives mycophenolic acid delayed-release tablets and MMF. Reduction in immunosuppression should be considered for patients who develop evidence of new or reactivated viral infections. Physicians should also consider the risk that reduced immunosuppression represents to the functioning allograft.
PVAN, especially due to BK virus infection, is associated with serious outcomes, including deteriorating renal function and renal graft loss. Patient monitoring may help detect patients at risk for PVAN.
PML, which is sometimes fatal, commonly presents with hemiparesis, apathy, confusion, cognitive deficiencies, and ataxia. Risk factors for PML include treatment with immunosuppressant therapies and impairment of immune function. In immunosuppressed patients, physicians should consider PML in the differential diagnosis in patients reporting neurological symptoms and consultation with a neurologist should be considered as clinically indicated.
The risk of CMV viremia and CMV disease is highest among transplant recipients seronegative for CMV at time of transplant who receive a graft from a CMV seropositive donor. Therapeutic approaches to limiting CMV disease exist and should be routinely provided. Patient monitoring may help detect patients at risk for CMV disease.
Viral reactivation has been reported in patients infected with HBV or HCV. Monitoring infected patients for clinical and laboratory signs of active HBV or HCV infection is recommended.
Blood Dyscrasias Including Pure Red Cell Aplasia
Cases of pure red cell aplasia (PRCA) have been reported in patients treated with MPA derivatives in combination with other immunosuppressive agents. The mechanism for MPA derivatives induced PRCA is unknown; the relative contribution of other immunosuppressants and their combinations in an immunosuppressive regimen is also unknown. In some cases PRCA was found to be reversible with dose reduction or cessation of therapy with MPA derivatives. In transplant patients, however, reduced immunosuppression may place the graft at risk. Changes to mycophenolic acid therapy should only be undertaken under appropriate supervision in transplant recipients in order to minimize the risk of graft rejection.
Patients receiving mycophenolic acid should be monitored for blood dyscrasias (e.g., neutropenia or anemia). The development of neutropenia may be related to mycophenolic acid itself, concomitant medications, viral infections, or some combination of these reactions. Complete blood count should be performed weekly during the first month, twice monthly for the second and the third month of treatment, then monthly through the first year. If blood dyscrasias occur [neutropenia develops (ANC <1.3×103/mcL) or anemia], dosing with mycophenolic acid should be interrupted or the dose reduced, appropriate tests performed, and the patient managed accordingly.
Serious GI Tract Complications
Gastrointestinal bleeding (requiring hospitalization), intestinal perforations, gastric ulcers, and duodenal ulcers have been reported in patients treated with mycophenolic acid delayed-release tablets. Mycophenolic acid delayed-release tablets should be administered with caution in patients with active serious digestive system disease.
Immunizations
The use of live attenuated vaccines should be avoided during treatment with mycophenolic acid delayed-release tablets; examples include (but not limited to) the following: intranasal influenza, measles, mumps, rubella, oral polio, BCG, yellow fever, varicella, and TY21a typhoid vaccines.
Rare Hereditary Deficiencies
Mycophenolic acid is an inosine monophosphate dehydrogenase inhibitor (IMPDH Inhibitor). Mycophenolic acid should be avoided in patients with rare hereditary deficiency of hypoxanthine-guanine phosphoribosyl-transferase (HGPRT) such as Lesch- Nyhan and Kelley-Seegmiller syndromes because it may cause an exacerbation of disease symptoms characterized by the overproduction and accumulation of uric acid leading to symptoms associated with gout such as acute arthritis, tophi, nephrolithiasis or urolithiasis and renal disease including renal failure.
Adverse Reactions
Clinical Trials Experience
The following adverse reactions are discussed in greater detail in other sections of the label.
- Embryofetal Toxicity
- Lymphomas and Other Malignancies
- Serious Infections
- New or Reactivated Viral Infections
- Blood Dyscrasias Including Pure Red Cell Aplasia
- Serious GI Tract Complications
- Rare Hereditary Deficiencies
Clinical Studies Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The data described below derive from two randomized, comparative, active-controlled, double-blind, double-dummy trials in prevention of acute rejection in de novo and converted stable kidney transplant patients.
- In the de novo trial, patients were administered either mycophenolic acid delayed-release tablets 1.44 grams per day (N=213) or MMF 2 grams per day (N=210) within 48 hours post-transplant for 12 months in combination with cyclosporine, USP MODIFIED and corticosteroids. Forty-one percent of patients also received antibody therapy as induction treatment. In the conversion trial, renal transplant patients who were at least 6 months post-transplant and receiving 2 grams per day MMF in combination with cyclosporine USP MODIFIED, with or without corticosteroids for at least two weeks prior to entry in the trial were randomized to mycophenolic acid delayed-release tablets 1.44 grams per day (N=159) or MMF 2 grams per day (N=163) for 12 months.
- The average age of patients in both studies was 47 years and 48 years (de novo study and conversion study, respectively), ranging from 22 to 75 years. Approximately 66% of patients were male; 82% were white, 12 % were black, and 6% other races. About 40% of patients were from the United States and 60% from other countries.
- In the de novo trial, the overall incidence of discontinuation due to adverse reactions was 18% (39/213) and 17% (35/210) in the mycophenolic acid delayed-release tablets and MMF arms, respectively. The most common adverse reactions leading to discontinuation in the mycophenolic acid arm were graft loss (2%), diarrhea (2%), vomiting (1%), renal impairment (1%), CMV infection (1%), and leukopenia (1%). The overall incidence of patients reporting dose reduction at least once during the 0 to12 month study period was 59% and 60% in the mycophenolic acid delayed-release tablets and MMF arms, respectively. The most frequent reasons for dose reduction in the mycophenolic acid delayed-release tablets arm were adverse reactions (44%), dose reductions according to protocol guidelines (17%), dosing errors (11%) and missing data (2%).
- The most common adverse reactions (≥20%) associated with the administration of mycophenolic acid delayed-release tablets were anemia, leukopenia, constipation, nausea, diarrhea, vomiting, dyspepsia, urinary tract infection, CMV infection, insomnia and postoperative pain.
- The adverse reactions reported in ≥10% of patients in the de novo trial are presented in Table 2 below.
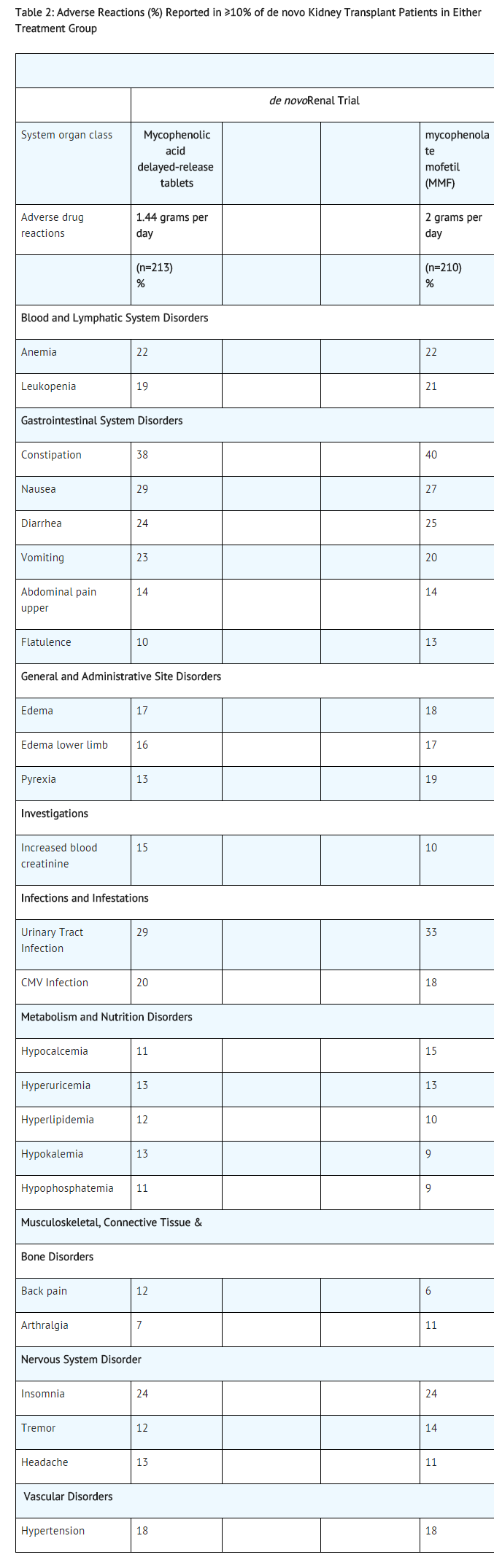
- The trial was not designed to support comparative claims for mycophenolic acid for the adverse reactions reported in this table.
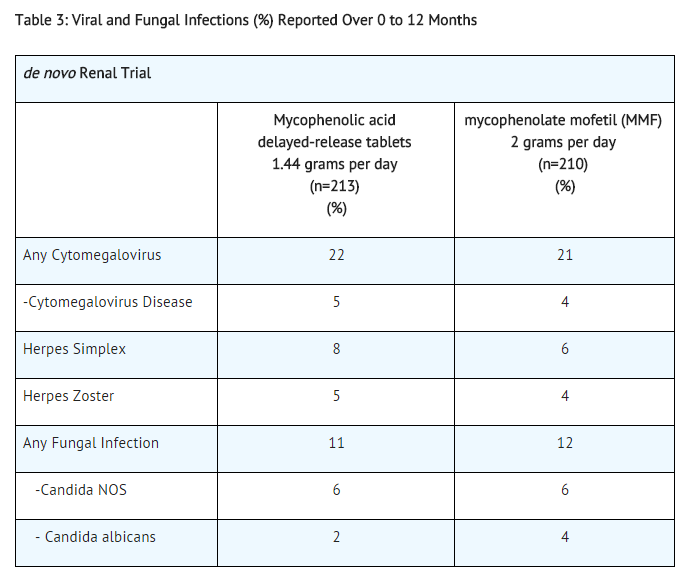
Table 3 summarizes the incidence of opportunistic infections in de novo transplant patients.
- Lymphoma developed in 2 de novo patients (1%), (1 diagnosed 9 days after treatment initiation) and in 2 conversion patients (1%) receiving mycophenolic acid delayed-release tablets with other immunosuppressive agents in the 12-month controlled clinical trials.
- Non melanoma skin carcinoma occurred in 1% de novo and 12% conversion patients. Other types of malignancy occurred in 1% de novo and 1% conversion patients.
- The adverse reactions reported in <10% of de novo or conversion patients treated with mycophenolic acid delayed-release tablets in combination with cyclosporine and corticosteroids are listed in Table 4.

- The following additional adverse reactions have been associated with the exposure to mycophenolic acid (MPA) when administered as a sodium salt or as mofetil ester:
- Gastrointestinal: Intestinal perforation, gastrointestinal hemorrhage, gastric ulcers, duodenal ulcers, colitis (including CMV colitis), pancreatitis, esophagitis, and ileus.
- Infections: Serious life-threatening infections such as meningitis and infectious endocarditis, tuberculosis, and atypical mycobacterial infection.
- Respiratory: Interstitial lung disorders, including fatal pulmonary fibrosis.
Postmarketing Experience
The following adverse reactions have been identified during post-approval use of mycophenolic acid or other MPA derivatives. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Congenital malformations and an increased incidence of first trimester pregnancy loss have been reported following exposure to MMF during pregnancy.
- Infections
- Cases of progressive multifocal leukoencephalopathy (PML), sometimes fatal.
- Polyomavirus associated nephropathy (PVAN), especially due to BK virus infection, associated with serious outcomes, including deteriorating renal function and renal graft loss.
- Viral reactivation in patients infected with HBV or HCV.
- Cases of pure red cell aplasia (PRCA) have been reported in patients treated with MPA derivatives in combination with other immunosuppressive agents .
- The following additional adverse reactions have been identified during postapproval use of mycophenolic acid: agranulocytosis, asthenia, osteomyelitis, lymphadenopathy, lymphopenia, wheezing, dry mouth, gastritis, peritonitis, anorexia, alopecia, pulmonary edema, Kaposi’s sarcoma.
Drug Interactions
Antacids with Magnesium and Aluminum Hydroxides
Concomitant use of mycophenolic acid delayed-release tablets and antacids decreased plasma concentrations of mycophenolic acid (MPA). It is recommended that mycophenolic acid delayed-release tablets and antacids not be administered simultaneously.
Azathioprine
Given that azathioprine and MMF inhibit purine metabolism, it is recommended that mycophenolic acid delayed-release tablets not be administered concomitantly with azathioprine or MMF.
Cholestyramine, Bile Acid Sequestrates, Oral Activated Charcoal and Other Drugs that Interfere with Enterohepatic Recirculation
Drugs that interrupt enterohepatic recirculation may decrease MPA plasma concentrations when coadministered with MMF. Therefore, do not administer mycophenolic acid delayed-release tablets with cholestyramine or other agents that may interfere with enterohepatic recirculation or drugs that may bind bile acids, e.g., bile acid sequestrates or oral activated charcoal, because of the potential to reduce the efficacy of mycophenolic acid delayed-release tablets.
Sevelamer
Concomitant administration of sevelamer and MMF may decrease MPA plasma concentrations. Sevelamer and other calcium free phosphate binders should not be administered simultaneously with mycophenolic acid delayed-release tablets.
Cyclosporine
Cyclosporine inhibits the enterohepatic recirculation of MPA, and therefore, MPA plasma concentrations may be decreased when mycophenolic acid delayed-release tablets are coadministered with cyclosporine. Clinicians should be aware that there is also a potential change of MPA plasma concentrations after switching from cyclosporine to other immunosuppressive drugs or from other immunosuppressive drugs to cyclosporine in patients concomitantly receiving mycophenolic acid delayed-release tablets.
Norfloxacin and Metronidazole
MPA plasma concentrations may be decreased when MMF is administrated with norfloxacin and metronidazole. Therefore, mycophenolic acid delayed-release tablets are not recommended to be given with the combination of norfloxacin and metronidazole. Although there will be no effect on MPA plasma concentrations when mycophenolic acid delayed-release tablets are concomitantly administered with norfloxacin or metronidazole when given separately [see Clinical Pharmacology (12.3)].
Rifampin
The concomitant administration of MMF and rifampin may decrease MPA plasma concentrations. Therefore, mycophenolic acid delayed-release tablets are not recommended to be given with rifampin concomitantly unless the benefit outweighs the risk.
Hormonal Contraceptives
In a drug interaction study, mean levonorgestrel AUC was decreased by 15% when coadministered with MMF. Although mycophenolic acid delayed-release tablets may not have any influence on the ovulation-suppressing action of oral contraceptives, it is recommended to coadminister mycophenolic acid delayed- release tablets with hormonal contraceptives (e.g., birth control pill, transdermal patch, vaginal ring, injection, and implant) with caution, and additional barrier contraceptive methods must be used.
Acyclovir (Valacyclovir), Ganciclovir (Valganciclovir), and Other Drugs that Undergo Renal Tubular Secretion
The coadministration of MMF and acyclovir or ganciclovir may increase plasma concentrations of mycophenolic acid glucuronide (MPAG) and acyclovir/valacyclovir/ganciclovir/valganciclovir as their coexistence competes for tubular secretion. Both acyclovir/valacyclovir/ganciclovir/valganciclovir and MPAG concentrations will be also increased in the presence of renal impairment. Acyclovir/valacyclovir/ganciclovir/valganciclovir may be taken with mycophenolic acid; however, during the period of treatment, physicians should monitor blood cell counts.
Ciprofloxacin, Amoxicillin plus Clavulanic Acid and Other Drugs that Alter the Gastrointestinal Flora
Drugs that alter the gastrointestinal flora such as ciprofloxacin or amoxicillin plus clavulanic acid may interact with MMF by disrupting enterohepatic recirculation. Interference of MPAG hydrolysis may lead to less MPA available for absorption when mycophenolic acid delayed-release tablet is concomitantly administered with ciprofloxacin or amoxicillin plus clavulanic acid. The clinical relevance of this interaction is unclear; however, no dose adjustment of mycophenolic acid delayed-release tablet is needed when coadministered with these drugs.
Pantoprazole
Administration of a pantoprazole at a dose of 40 mg twice daily for 4 days to healthy volunteers did not alter the pharmacokinetics of a single dose of mycophenolic acid delayed-release tablets.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Pregnancy Category D
For those females using mycophenolic acid at any time during pregnancy and those becoming pregnant within 6 weeks of discontinuing therapy, the healthcare practitioner should report the pregnancy to the Mycophenolate Pregnancy Registry (1-800-617-8191). The healthcare practitioner should strongly encourage the patient to enroll in the pregnancy registry. The information provided to the registry will help the Health Care Community to better understand the effects of mycophenolate in pregnancy.
Risk Summary
- Following oral or intravenous (IV) administration, MMF is metabolized to mycophenolic acid (MPA), the active ingredient in mycophenolic acid delayed-release tablets and the active form of the drug. Use of MMF during pregnancy is associated with an increased risk of first trimester pregnancy loss and an increased risk of congenital malformations, especially external ear and other facial abnormalities including cleft lip and palate, and anomalies of the distal limbs, heart, esophagus, and kidney. In animal studies, congenital malformations and pregnancy loss occurred when pregnant rats and rabbits received mycophenolic acid at dose multiples similar to and less than clinical doses.
- Risks and benefits of mycophenolic acid delayed-release tablets should be discussed with the patient. When appropriate, consider alternative immunosuppressants with less potential for embryofetal toxicity. In certain situations, the patient and her healthcare practitioner may decide that the maternal benefits outweigh the risks to the fetus. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
Data
Human Data
- In the National Transplantation Pregnancy Registry (NTPR), there were data on 33 MMF-exposed pregnancies in 24 transplant patients; there were 15 spontaneous abortions (45%) and 18 live-born infants. Four of these 18 infants had structural malformations (22%). In postmarketing data (collected from 1995 to 2007) on 77 women exposed to systemic MMF during pregnancy, 25 had spontaneous abortions and 14 had a malformed infant or fetus. Six of 14 malformed offspring had ear abnormalities. Because these postmarketing data are reported voluntarily, it is not always possible to reliably estimate the frequency of particular adverse outcomes. These malformations are similar to findings in animal reproductive toxicology studies. For comparison, the background rate for congenital anomalies in the United States is about 3%, and NTPR data show a rate of 4% to 5% among babies born to organ transplant patients using other immunosuppressive drugs. There are no relevant qualitative or quantitative differences in the teratogenic potential of mycophenolate sodium and MMF.
Animal Data
- In a teratology study performed with mycophenolate sodium in rats, at a dose as low as 1 mg per kg, malformations in the offspring were observed, including anophthalmia, exencephaly, and umbilical hernia. The systemic exposure at this dose represents 0.05 times the clinical exposure at the dose of 1440 mg per day mycophenolic acid delayed-release tablets. In teratology studies in rabbits, fetal resorptions and malformations occurred at doses equal to or greater than 80 mg per kg per day, in the absence of maternal toxicity (which corresponds to about 1.1 times the recommended clinical dose, based on body surface area).
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Mycophenolate sodium in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Mycophenolate sodium during labor and delivery.
Nursing Mothers
- It is not known whether MPA is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from mycophenolic acid delayed-release tablets, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- The safety and effectiveness of mycophenolic acid delayed-release tablets have been established in pediatric kidney transplant patients 5 to 16 years of age who were initiated on mycophenolic acid delayed-release tablets at least 6 months post-transplant. Use of mycophenolic acid delayed-release tablets in this age group is supported by evidence from adequate and well-controlled studies of mycophenolic acid delayed-release tablets in a similar population of adult kidney transplant patients with additional pharmacokinetic data in pediatric kidney transplant patients.
- Pediatric doses for patients with BSA <1.19 m2 cannot be accurately administered using currently available formulations of mycophenolic acid delayed-release tablets. The safety and effectiveness of mycophenolic acid delayed-release tablets in de novo pediatric kidney transplant patients and in pediatric kidney transplant patients below the age of 5 years have not been established.
Geriatic Use
- Clinical studies of mycophenolic acid delayed-release tablets did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Of the 372 patients treated with mycophenolic acid delayed-release tablets in the clinical trials, 6% (N=21) were 65 years of age and older and 0.3% (N=1) were 75 years of age and older. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Gender
Females of Reproductive Potential
Pregnancy Exposure Prevention and Planning
- Females of reproductive potential must be made aware of the increased risk of first trimester pregnancy loss and congenital malformations and must be counseled regarding pregnancy prevention and planning.
- Females of reproductive potential include girls who have entered puberty and all women who have a uterus and have not passed through menopause. Menopause is the permanent end of menstruation and fertility. Menopause should be clinically confirmed by a patient’s healthcare practitioner. Some commonly used diagnostic criteria include 1) 12 months of spontaneous amenorrhea (not amenorrhea induced by a medical condition or medical therapy), or 2) postsurgical from a bilateral oophorectomy.
Pregnancy Testing
- To prevent unplanned exposure during pregnancy, females of reproductive potential should have a serum or urine pregnancy test with a sensitivity of at least 25 mIU/mL immediately before starting mycophenolic acid delayed-release tablets. Another pregnancy test with the same sensitivity should be done 8 to 10 days later. Repeat pregnancy tests should be performed during routine follow-up visits. Results of all pregnancy tests should be discussed with the patient.
- In the event of a positive pregnancy test, females should be counseled with regard to whether the maternal benefits of mycophenolate treatment may outweigh the risks to the fetus in certain situations.
Contraception
- Females of reproductive potential taking mycophenolic acid delayed-release tablets must receive contraceptive counseling and use acceptable contraception (see Table 5 for Acceptable Contraception Methods). Patients must use acceptable birth control during entire mycophenolic acid delayed-release tablets therapy, and for 6 weeks after stopping mycophenolic acid delayed-release tablets, unless the patient chooses abstinence (she chooses to avoid heterosexual intercourse completely).
- Patients should be aware that mycophenolic acid delayed-release tablets reduce blood levels of the hormones in the oral contraceptive pill and could theoretically reduce its effectiveness.

Pregnancy Planning
- For patients who are considering pregnancy, consider alternative immunosuppressants with less potential for embryofetal toxicity. Risks and benefits of mycophenolic acid delayed-release tablets should be discussed with the patient.
Race
There is no FDA guidance on the use of Mycophenolate sodium with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Mycophenolate sodium in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Mycophenolate sodium in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Mycophenolate sodium in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Mycophenolate sodium in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
- Mycophenolic acid delayed-release tablets should be taken on an empty stomach, 1 hour before or 2 hours after food intake.
- Mycophenolic acid delayed-release tablets should not be crushed, chewed, or cut prior to ingesting. The tablets should be swallowed whole in order to maintain the integrity of the enteric coating.
- Pediatric patients with a BSA of 1.19 to 1.58 m2 may be dosed either with three mycophenolic acid 180 mg tablets, or one 180 mg tablet plus one 360 mg tablet twice daily (1080 mg daily dose). Patients with a BSA of >1.58 m2 may be dosed either with four mycophenolic acid 180 mg tablets, or two mycophenolic acid 360 mg tablets twice daily (1440 mg daily dose). Pediatric doses for patients with BSA <1.19 m2 cannot be accurately administered using currently available formulations of mycophenolic acid tablets.
Monitoring
There is limited information regarding Mycophenolate sodium Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Mycophenolate sodium and IV administrations.
Overdosage
Signs and Symptoms
- There have been anecdotal reports of deliberate or accidental overdoses with mycophenolic acid delayed-release tablets, whereas not all patients experienced related adverse reactions.
- In those overdose cases in which adverse reactions were reported, the reactions fall within the known safety profile of the class. Accordingly an overdose of mycophenolic acid delayed-release tablets could possibly result in over suppression of the immune system and may increase the susceptibility to infection including opportunistic infections, fatal infections and sepsis. If blood dyscrasias occur (e.g., neutropenia with absolute neutrophil count <1.5 x 103/mcL or anemia), it may be appropriate to interrupt or discontinue mycophenolic acid delayed-release tablets.
- Possible signs and symptoms of acute overdose could include the following: hematological abnormalities such as leukopenia and neutropenia, and gastrointestinal symptoms such as abdominal pain, diarrhea, nausea and vomiting, and dyspepsia.
Treatment and Management
General supportive measures and symptomatic treatment should be followed in all cases of overdosage. Although dialysis may be used to remove the inactive metabolite mycophenolic acid glucuronide (MPAG), it would not be expected to remove clinically significant amounts of the active moiety, mycophenolic acid, due to the 98% plasma protein binding of mycophenolic acid. By interfering with enterohepatic circulation of mycophenolic acid, activated charcoal or bile sequestrates, such as cholestyramine, may reduce the systemic mycophenolic acid exposure.
Pharmacology

Mechanism of Action
- Mycophenolic acid (MPA), an immunosuppressant, is an uncompetitive and reversible inhibitor of inosine monophosphate dehydrogenase (IMPDH), and therefore inhibits the de novo pathway of guanosine nucleotide synthesis without incorporation to DNA. T- and B-lymphocytes are critically dependent for their proliferation on de novo synthesis of purines, whereas other cell types can utilize salvage pathways. MPA has cytostatic effects on lymphocytes.
- Mycophenolate sodium has been shown to prevent the occurrence of acute rejection in rat models of kidney and heart allotransplantation. Mycophenolate sodium also decreases antibody production in mice.
Structure
There is limited information regarding Mycophenolate sodium Structure in the drug label.
Pharmacodynamics
There is limited information regarding Mycophenolate sodium Pharmacodynamics in the drug label.
Pharmacokinetics
- Mycophenolic acid delayed-release tablets exhibit linear and dose-proportional pharmacokinetics over the dose-range (360 to 2160 mg) evaluated. The absolute bioavailability of mycophenolic acid delayed-release tablets in stable renal transplant patients on cyclosporine was 72%. MPA is highly protein bound (>98% bound to albumin). The predominant metabolite of MPA is the phenolic glucuronide (MPAG) which is pharmacologically inactive. A minor metabolite AcMPAG which is an acyl glucuronide of MPAG is also formed and has pharmacological activity comparable to MPA. MPAG undergoes renal elimination. A fraction of MPAG also undergoes biliary excretion, followed by deconjugation by gut flora and subsequent reabsorption as MPA. The mean elimination half-lives of MPA and MPAG ranged between 8 and 16 hours, and 13 and 17 hours, respectively.
Absorption
- In vitro studies demonstrated that the enteric-coated mycophenolic acid tablet does not release MPA under acidic conditions (pH <5) as in the stomach but is highly soluble in neutral pH conditions as in the intestine. Following mycophenolic acid oral administration without food in several pharmacokinetic studies conducted in renal transplant patients, consistent with its enteric-coated formulation, the median delay (Tlag) in the rise of MPA concentration ranged between 0.25 and 1.25 hours and the median time to maximum concentration (Tmax) of MPA ranged between 1.5 and 2.75 hours. In comparison, following the administration of MMF, the median Tmax ranged between 0.5 and 1.0 hours. In stable renal transplant patients on cyclosporine, USP MODIFIED based immunosuppression, gastrointestinal absorption and absolute bioavailability of MPA following the administration of mycophenolic acid delayed-release tablet was 93% and 72%, respectively. Mycophenolic acid delayed-release tablets pharmacokinetics is dose proportional over the dose range of 360 to 2160 mg.
Distribution
- The mean (± SD) volume of distribution at steady state and elimination phase for MPA is 54 (± 25) L and 112 (± 48) L, respectively. MPA is highly protein bound to albumin, >98%. The protein binding of mycophenolic acid glucuronide (MPAG) is 82%. The free MPA concentration may increase under conditions of decreased protein binding (uremia, hepatic failure, and hypoalbuminemia).
Metabolism
- MPA is metabolized principally by glucuronyl transferase to glucuronidated metabolites. The phenolic glucuronide of MPA, mycophenolic acid glucuronide (MPAG), is the predominant metabolite of MPA and does not manifest pharmacological activity. The acyl glucuronide is a minor metabolite and has comparable pharmacological activity to MPA. In stable renal transplant patients on cyclosporine, USP MODIFIED based immunosuppression, approximately 28% of the oral mycophenolic acid delayed-release tablets dose was converted to MPAG by presystemic metabolism. The AUC ratio of MPA:MPAG:acyl glucuronide is approximately 1:24:0.28 at steady state. The mean clearance of MPA was 140 (± 30) mL/min.
Elimination
- The majority of MPA dose administered is eliminated in the urine primarily as MPAG (>60%) and approximately 3% as unchanged MPA following mycophenolic acid administration to stable renal transplant patients. The mean renal clearance of MPAG was 15.5 (± 5.9) mL/min. MPAG is also secreted in the bile and available for deconjugation by gut flora. MPA resulting from the deconjugation may then be reabsorbed and produce a second peak of MPA approximately 6 to 8 hours after mycophenolic acid dosing. The mean elimination half-life of MPA and MPAG ranged between 8 and 16 hours, and 13 and 17 hours, respectively.
Food Effect
- Compared to the fasting state, administration of mycophenolic acid delayed-release tablets 720 mg with a high-fat meal (55 g fat, 1000 calories) had no effect on the systemic exposure (AUC) of MPA. However, there was a 33% decrease in the maximal concentration (Cmax), a 3.5-hour delay in the Tlag (range, -6 to 18 hours), and 5.0-hour delay in the Tmax (range, -9 to 20 hours) of MPA. To avoid the variability in MPA absorption between doses, mycophenolic acid delayed-release tablets should be taken on an empty stomach.
Pharmacokinetics in Renal Transplant Patients
- The mean pharmacokinetic parameters for MPA following the administration of mycophenolic acid in renal transplant patients on cyclosporine, USP MODIFIED based immunosuppression are shown in Table 6. Single-dose mycophenolic acid pharmacokinetics predicts multiple-dose pharmacokinetics. However, in the early post-transplant period, mean MPA AUC and Cmax were approximately one-half of those measured 6 months post-transplant.
- After near equimolar dosing of mycophenolic acid 720 mg twice daily and MMF 1000 mg twice daily (739 mg as MPA) in both the single- and multiple-dose cross-over trials, mean systemic MPA exposure (AUC) was similar.

Specific Populations
- Renal Insufficiency: No specific pharmacokinetic studies in individuals with renal impairment were conducted with mycophenolic acid delayed-release tablets. However, based on studies of renal impairment with MMF, MPA exposure is not expected to be appreciably increased over the range of normal to severely impaired renal function following mycophenolic acid delayed-release tablets administration.
- In contrast, MPAG exposure would be increased markedly with decreased renal function; MPAG exposure being approximately 8-fold higher in the setting of anuria. Although dialysis may be used to remove the inactive metabolite MPAG, it would not be expected to remove clinically significant amounts of the active moiety MPA. This is in large part due to the high plasma protein binding of MPA.
- Hepatic Insufficiency: No specific pharmacokinetic studies in individuals with hepatic impairment were conducted with mycophenolic acid delayed-release tablets. In a single dose (MMF 1000 mg) trial of 18 volunteers with alcoholic cirrhosis and 6 healthy volunteers, hepatic MPA glucuronidation processes appeared to be relatively unaffected by hepatic parenchymal disease when the pharmacokinetic parameters of healthy volunteers and alcoholic cirrhosis patients within this trial were compared. However, it should be noted that for unexplained reasons, the healthy volunteers in this trial had about a 50% lower AUC compared to healthy volunteers in other studies, thus making comparison between volunteers with alcoholic cirrhosis and healthy volunteers difficult. Effects of hepatic disease on this process probably depend on the particular disease. Hepatic disease, such as primary biliary cirrhosis, with other etiologies may show a different effect.
- Pediatrics: Limited data are available on the use of mycophenolic acid delayed-release tablets at a dose of 450 mg/m2 body surface area in children. The mean MPA pharmacokinetic parameters for stable pediatric renal transplant patients, 5 to 16 years, on cyclosporine, USP MODIFIED are shown in Table 6. At the same dose administered based on body surface area, the respective mean Cmax and AUC of MPA determined in children were higher by 33% and 18% than those determined for adults. The clinical impact of the increase in MPA exposure is not known.
- Gender: There are no significant gender differences in mycophenolic acid delayed-release tablets pharmacokinetics.
- Elderly: Pharmacokinetics in the elderly have not been formally studied.
- Ethnicity: Following a single dose administration of 720 mg of mycophenolic acid delayed-release tablets to 18 Japanese and 18 Caucasian healthy subjects, the exposure (AUCinf) for MPA and MPAG were 15% and 22% lower in Japanese subjects compared to Caucasians. The peak concentrations (Cmax) for MPAG were similar between the two populations, however, Japanese subjects had 9.6% higher Cmax for MPA. These results do not suggest any clinically relevant differences.
Drug Interactions:
Antacids with Magnesium and Aluminum Hydroxides:
- Absorption of a single dose of mycophenolic acid delayed-release tablets was decreased when administered to 12 stable kidney transplant patients also taking magnesium-aluminum-containing antacids (30 mL): the mean Cmax and AUC(0 to t) values for MPA were 25% and 37% lower, respectively, than when mycophenolic acid delayed-release tablets were administered alone under fasting conditions.
Pantoprazole:
- In a trial conducted in 12 healthy volunteers, the pharmacokinetics of MPA were observed to be similar when a single dose of 720 mg of mycophenolic acid delayed-release tablets was administered alone and following concomitant administration of mycophenolic acid delayed-release tablets and pantoprazole, which was administered at a dose of 40 mg twice daily for 4 days.
- The following drug interaction studies were conducted following the administration of MMF:
Cholestyramine
- Following single-dose oral administration of 1.5 grams MMF to 12 healthy volunteers pretreated with 4 grams three times daily of cholestyramine for 4 days, MPA AUC decreased approximately 40%. This decrease is consistent with interruption of enterohepatic recirculation which may be due to binding of recirculating MPAG with cholestyramine in the intestine.
Sevelamer
- Concomitant administration of sevelamer and MMF in stable adult and pediatric kidney transplant patients decreased the mean MPA Cmax and AUC(0 to 12h) by 36% and 26% respectively.
Cyclosporine
- Cyclosporine (Sandimmune®) pharmacokinetics (at doses of 275 to 415 mg/day) were unaffected by single and multiple doses of 1.5 grams twice daily of MMF in 10 stable kidney transplant patients. The mean (±SD) AUC(0 to 12h) and Cmax of cyclosporine after 14 days of multiple doses of MMF were 3290 (±822) ng•h/mL and 753 (±161) ng/mL, respectively, compared to 3245 (±1088) ng•h/mL and 700 (±246) ng/mL, respectively, 1 week before administration of MMF.
- A total of 73 de novo kidney allograft recipients on MMF therapy received either low dose cyclosporine withdrawal by 6 months post-transplant (50 to 100 ng/mL for up to 3 months post-transplant followed by complete withdrawal at month 6 post-transplant) or standard dose cyclosporine (150 to 300 ng/mL from baseline through to month 4 post-transplant and 100 to 200 ng/mL thereafter). At month 12 post-transplant, the mean MPA (AUC(0 to 12h)) in the cyclosporine withdrawal group was approximately 40% higher, than that of the standard dose cyclosporine group.
- Cyclosporine inhibits multidrug-resistance-associated protein 2 (MRP-2) transporter in the biliary tract, thereby preventing the excretion of MPAG into the bile that would lead to enterohepatic recirculation of MPA [see Drug Interactions (7.5)].
Norfloxacin and Metronidazole
- Following single-dose administration of MMF (1 g) to 11 healthy volunteers on day 4 of a 5 day course of a combination of norfloxacin and metronidazole, the mean MPA AUC(0 to 48h) was reduced by 33% compared to the administration of MMF alone (p<0.05). There was no significant effect on mean MPA AUC(0 to 48h) when MMF was concomitantly administered with norfloxacin or metronidazole separately. The mean (±SD) MPA AUC(0 to 48h) after coadministration of MMF with norfloxacin or metronidazole separately was 48.3 (±24) mcg•h/mL and 42.7 (±23) mcg•h/mL, respectively, compared with 56.2 (±24) mcg•h/mL after administration of MMF alone.
Rifampin
- In a single heart-lung transplant patient on MMF therapy (1 gram twice daily), a 67% decrease in MPA exposure (AUC(0 to12h)) was observed with concomitant administration of MMF and 600 mg rifampin daily.
- In 8 kidney transplant patients on stable MMF therapy (1 gram twice daily), administration of 300 mg rifampin twice daily resulted in a 17.5% decrease in MPA AUC(0 to 12h) due to inhibition of enterohepatic recirculation of MPAG by rifampin. Rifampin coadministration also resulted in a 22.4% increase in MPAG AUC(0 to 12h).
Oral Contraceptives
- In a drug-drug interaction trial, mean AUCs were similar for ethinyl estradiol and norethindrone, when coadministered with MMF as compared to administration of the oral contraceptives alone.
Acyclovir
- Coadministration of MMF (1 gram) and acyclovir (800 mg) to 12 healthy volunteers resulted in no significant change in MPA AUC and Cmax. However, MPAG and acyclovir plasma mean AUC(0 to 24h) were increased 10% and 18%, respectively. Because MPAG plasma concentrations are increased in the presence of kidney impairment, as are acyclovir concentrations, the potential exists for mycophenolate and acyclovir or its prodrug (e.g., valacyclovir) to compete for tubular secretion, further increasing the concentrations of both drugs.
Ganciclovir
- Following single-dose administration to 12 stable kidney transplant patients, no pharmacokinetic interaction was observed between MMF (1.5 grams) and intravenous ganciclovir (5 mg per kg). Mean (±SD) ganciclovir AUC and Cmax (n=10) were 54.3 (±19.0) mcg•h/mL and 11.5 (±1.8) mcg/mL, respectively, after coadministration of the two drugs, compared to 51.0 (±17.0) mcg•h/mL and 10.6 (±2.0) mcg/mL, respectively, after administration of intravenous ganciclovir alone. The mean (±SD) AUC and Cmax of MPA (n=12) after coadministration were 80.9 (±21.6) mcg•h/mL and 27.8 (±13.9) mcg/mL, respectively, compared to values of 80.3 (±16.4) mcg•h/mL and 30.9 (±11.2) mcg/mL, respectively, after administration of MMF alone.
- Because MPAG plasma concentrations are increased in the presence of renal impairment, as are ganciclovir concentrations, the two drugs will compete for tubular secretion and thus further increases in concentrations of both drugs may occur. In patients with renal impairment in which MMF and ganciclovir or its prodrug (e.g., valganciclovir) are coadministered, patients should be monitored carefully.
Ciprofloxacin and Amoxicillin plus Clavulanic Acid
- A total of 64 MMF treated kidney transplant recipients received either oral ciprofloxacin 500 mg twice daily or amoxicillin plus clavulanic acid 375 mg three times daily for 7 or at least 14 days. Approximately 50% reductions in median trough MPA concentrations (predose) from baseline (MMF alone) were observed in 3 days following commencement of oral ciprofloxacin or amoxicillin plus clavulanic acid. These reductions in trough MPA concentrations tended to diminish within 14 days of antibiotic therapy and ceased within 3 days after discontinuation of antibiotics. The postulated mechanism for this interaction is an antibiotic-induced reduction in glucuronidase-possessing enteric organisms leading to a decrease in enterohepatic recirculation of MPA. The change in trough level may not accurately represent changes in overall MPA exposure; therefore, clinical relevance of these observations is unclear.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- In a 104-week oral carcinogenicity study in rats, mycophenolate sodium was not tumorigenic at daily doses up to 9 mg per kg, the highest dose tested. This dose resulted in approximately 0.6 to 1.2 times the systemic exposure (based on plasma AUC) observed in renal transplant patients at the recommended dose of 1440 mg per day. Similar results were observed in a parallel study in rats performed with MMF. In a 104-week oral carcinogenicity study in mice, MMF was not tumorigenic at a daily dose level as high as 180 mg per kg (which corresponds to 0.6 times the recommended mycophenolate sodium therapeutic dose, based on body surface area).
- The genotoxic potential of mycophenolate sodium was determined in five assays. Mycophenolate sodium was genotoxic in the mouse lymphoma/thymidine kinase assay, the micronucleus test in V79 Chinese hamster cells, and the in vivo mouse micronucleus assay. Mycophenolate sodium was not genotoxic in the bacterial mutation assay (Salmonella typhimurium TA 1535, 97a, 98, 100, and 102) or the chromosomal aberration assay in human lymphocytes.
- Mycophenolate mofetil generated similar genotoxic activity. The genotoxic activity of mycophenolic acid (MPA) is probably due to the depletion of the nucleotide pool required for DNA synthesis as a result of the pharmacodynamic mode of action of MPA (inhibition of nucleotide synthesis).
- Mycophenolate sodium had no effect on male rat fertility at daily oral doses as high as 18 mg per kg and exhibited no testicular or spermatogenic effects at daily oral doses of 20 mg per kg for 13 weeks (approximately 2 times the systemic exposure of MPA at the recommended therapeutic dose). No effects on female fertility were seen up to a daily dose of 20 mg per kg (approximately 3 times the systemic exposure of MPA at the recommended therapeutic dose).
Clinical Studies
Prophylaxis of Organ Rejection in Patients Receiving Allogeneic Renal Transplants
- The safety and efficacy of mycophenolic acid delayed-release tablets in combination with cyclosporine, USP MODIFIED and corticosteroids for the prevention of organ rejection was assessed in two multicenter, randomized, double-blind active-controlled trials in de novo and conversion renal transplant patients compared to MMF.
- The de novo trial was conducted in 423 renal transplant patients (ages 18 to 75 years) in Austria, Canada, Germany, Hungary, Italy, Norway, Spain, UK, and USA. Eighty-four percent of randomized patients received kidneys from deceased donors. Patients were excluded if they had second or multi-organ (e.g., kidney and pancreas) transplants, or previous transplant with any other organs; kidneys from non-heart beating donors; panel reactive antibodies (PRA) of >50% at last assessment prior to transplantation, and presence of severe diarrhea, active peptic ulcer disease, or uncontrolled diabetes mellitus. Patients were administered either mycophenolic acid delayed-release tablets 1.44 grams per day or MMF 2 grams per day within 48 hours post-transplant for 12 months in combination with cyclosporine, USP MODIFIED and corticosteroids. Forty-one percent of patients received antibody therapy as induction treatment. Treatment failure was defined as the first occurrence of biopsy proven acute rejection, graft loss, death or lost to follow-up at 6 months.
- The incidence of treatment failure was similar in mycophenolic acid delayed-release tablets - and MMF-treated patients at 6 and 12 months (Table 7). The cumulative incidence of graft loss, death and lost to follow-up at 12 months is also shown in Table 7.
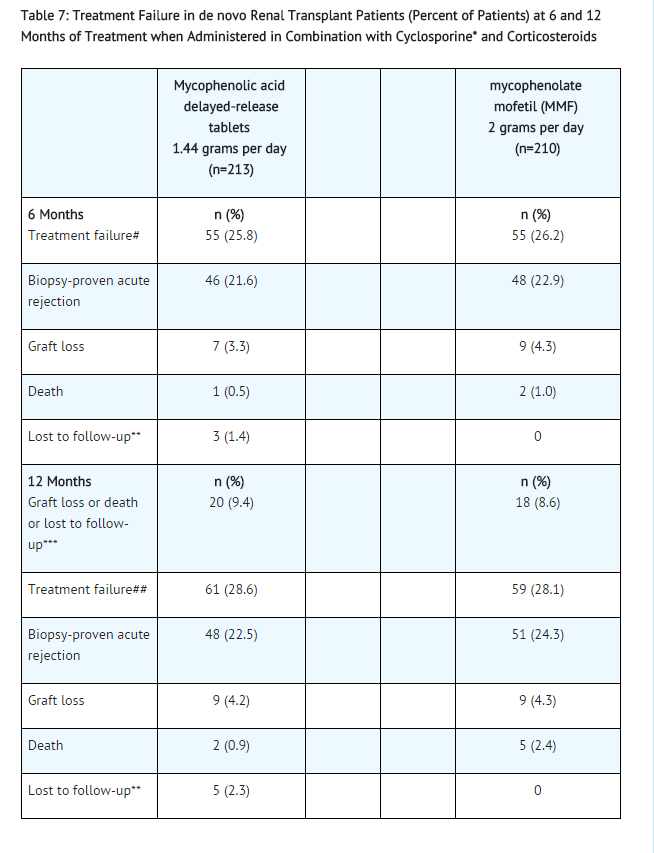
- USP MODIFIED**Lost to follow-up indicates patients who were lost to follow-up without prior biopsy-proven acute rejection, graft loss or death
- Lost to follow-up indicates patients who were lost to follow-up without prior graft loss or death (9 mycophenolic acid delayed-release tablets patients and 4 MMF patients)
- 95% confidence interval of the difference in treatment failure at 6 months (mycophenolic acid delayed-release tablets – MMF) is (-8.7%, 8.0%).
- 95% confidence interval of the difference in treatment failure at 12 months (mycophenolic acid delayed-release tablets – MMF) is (-8.0%, 9.1%).
- The conversion trial was conducted in 322 renal transplant patients (ages 18–75 years), who were at least 6 months post-transplant and had undergone primary or secondary, deceased donor, living related, or unrelated donor kidney transplant, stable graft function (serum creatinine <2.3 mg/mL), no change in immunosuppressive regimen due to graft malfunction, and no known clinically significant physical and/or laboratory changes for at least 2 months prior to enrollment. Patients were excluded if they had 3 or more kidney transplants, multiorgan transplants (e.g., kidney and pancreas), previous organ transplants, evidence of graft rejection or who had been treated for acute rejection within 2 months prior to screening, clinically significant infections requiring continued therapy, presence of severe diarrhea, active peptic ulcer disease, or uncontrolled diabetes mellitus.
- Patients received 2 grams per day MMF in combination with cyclosporine USP MODIFIED, with or without corticosteroids for at least two weeks prior to entry in the trial. Patients were randomized to mycophenolic acid delayed-release tablets 1.44 grams per day or MMF 2 grams per day for 12 months. The trial was conducted in Austria, Belgium, Canada, Germany, Italy, Spain, and USA. Treatment failure was defined as the first occurrence of biopsy-proven acute rejection, graft loss, death, or lost to follow-up at 6 and 12 months.
- The incidences of treatment failure at 6 and 12 months were similar between mycophenolic acid delayed- release tablets - and MMF-treated patients (Table 8). The cumulative incidence of graft loss, death and lost to follow-up at 12 months is also shown in Table 8.
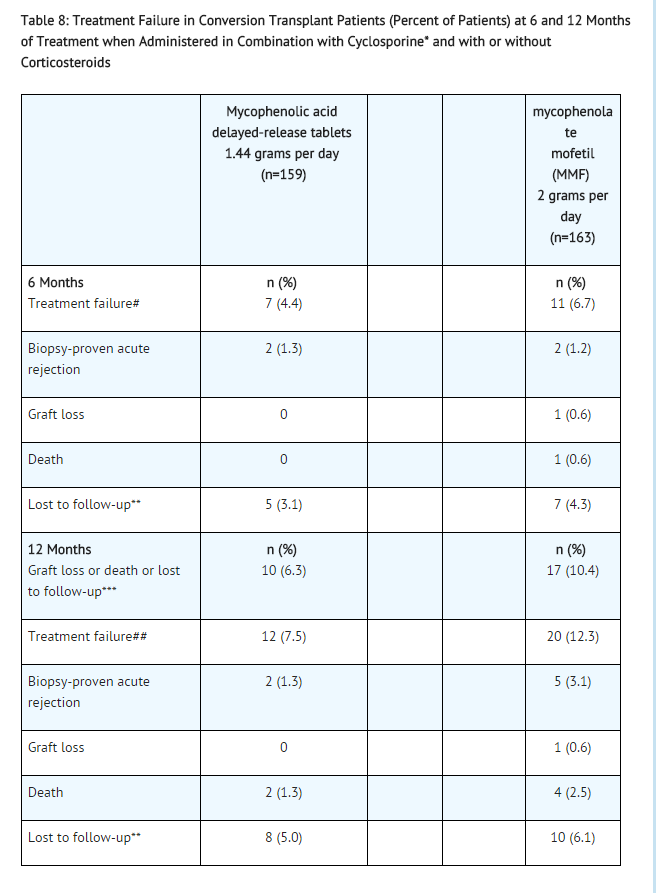
- USP MODIFIED**Lost to follow-up indicates patients who were lost to follow-up without prior biopsy-proven acute rejection, graft loss, or death
- Lost to follow-up indicates patients who were lost to follow-up without prior graft loss or death (8 mycophenolic acid delayed- release tablets patients and 12 MMF patients)
- 95% confidence interval of the difference in treatment failure at 6 months (mycophenolic acid delayed-release tablets – MMF) is (-7.3%, 2.7%).
- 95% confidence interval of the difference in treatment failure at 12 months (mycophenolic acid delayed-release tablets – MMF) is (-11.2%, 1.8%).
How Supplied
- Mycophenolic Acid Delayed-Release Tablets are supplied as:
180 mg tablet: Light green, round, slightly biconvex beveled edge enteric coated tablet, engraved “MYC” over “180” on one side, “APO” on the other side, containing 180 mg mycophenolic acid (MPA) as mycophenolate sodium.
Bottles of 120……………………………………………….… NDC 60429-016-12
360 mg tablet: Light pink, oval, biconvex enteric coated tablet, engraved “APO” on one side, “MYC 360” on the other side, containing 360 mg mycophenolic acid (MPA) as mycophenolate sodium.
Bottles of 120……………………………………………….… NDC 60429-017-12
Storage
- Store at 25°C (77°F); excursions permitted to 15 to 30°C (59 to 86°F) [see USP Controlled Room Temperature]. Protect from moisture. Dispense in a tight container (USP).
Images
Drug Images
{{#ask: Page Name::Mycophenolate sodium |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Mycophenolate sodium |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Embryofetal Toxicity
- Inform pregnant women and females of reproductive potential that use of mycophenolic acid delayed-release tablets in pregnancy is associated with an increased risk of first trimester pregnancy loss and an increased risk of congenital malformations.
- In the event of a positive pregnancy test, discuss the risks and benefits of mycophenolic acid delayed-release tablets with the patient. Encourage her to enroll in the pregnancy registry. (1-800-617-8191).
Pregnancy Exposure Prevention and Planning
- Discuss pregnancy testing, pregnancy prevention and planning with females of reproductive potential.
- Inform females of reproductive potential must use acceptable birth control during entire mycophenolic acid delayed-release tablets therapy and for 6 weeks after stopping mycophenolic acid delayed-release tablets, unless the patient chooses to avoid heterosexual sexual intercourse completely (abstinence).
- For patients who are considering pregnancy, discuss appropriate alternative immunosuppressants with less potential for embryofetal toxicity. Risks and benefits of mycophenolic acid delayed-release tablets should be discussed with the patient.
Nursing Mothers
- Advise patients that they should not breastfeed during mycophenolic acid delayed-release tablets therapy.
Development of Lymphoma and Other Malignancies
- Inform patients they are at increased risk of developing lymphomas and other malignancies, particularly of the skin, due to immunosuppression.
- Advise patients to limit exposure to sunlight and ultraviolet (UV) light by wearing protective clothing and use a sunscreen with a high protection factor.
Increased Risk of Infection
- Inform patients they are at increased risk of developing a variety of infections, including opportunistic infections, due to immunosuppression and to contact their physician if they develop any symptoms of infection.
Blood Dyscrasias
- Inform patients they are at increased risk for developing blood dyscrasias (e.g., neutropenia or anemia) and to immediately contact their healthcare provider if they experience any evidence of infection, unexpected bruising, bleeding, or any other manifestation of bone marrow suppression.
Gastrointestinal Tract Complications
- Inform patients that mycophenolic acid delayed-release tablets can cause gastrointestinal tract complications including bleeding, intestinal perforations, and gastric or duodenal ulcers. Advise the patient to contact their healthcare provider if they have symptoms of gastrointestinal bleeding or sudden onset or persistent abdominal pain.
Immunizations
- Inform patients that mycophenolic acid delayed-release tablets can interfere with the usual response to immunizations and that they should avoid live vaccines.
Administration Instructions
- Advise patients to swallow mycophenolic acid delayed-release tablets whole, and not crush, chew, or cut the tablets. Inform patients to take mycophenolic acid delayed-release tablets on an empty stomach, 1 hour before or 2 hours after food intake.
Drug Interactions
- Patients should be advised to report to their doctor the use of any other medications while taking mycophenolic acid delayed-release tablets. The simultaneous administration of any of the following drugs with mycophenolic acid delayed-release tablets may result in clinically significant adverse reactions:
Antacids with magnesium and aluminum hydroxides
Azathioprine
Cholestyramine
Hormonal Contraceptives (e.g., birth control pill, transdermal patch, vaginal ring, injection, and implant)
Precautions with Alcohol
Alcohol-Mycophenolic acid interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- MYCOPHENOLIC ACID
Look-Alike Drug Names
There is limited information regarding Mycophenolate sodium Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.